Two cases of pulmonary cysticercosis manifesting as pleural effusion: case report and literature review
Introduction
Human cysticercosis is a serious public health problem, especially in developing countries. It is caused by the presence of the larval stage of the pork tapeworm (Taenia solium) in the tissue. It occurs when humans ingest undercooked pork, contaminated food stuffs or water which harbors eggs of the tapeworm. Most cases involve the neurologic, muscular, dermatologic, and ophthalmologic systems, and so on. Pulmonary involvement has been seen in many cases of disseminated cysticercosis, but isolated pulmonary involvement is seldom reported. We present two cases in which pleural effusion due to cysticercosis were detected on chest X-ray and computed tomography (CT) scan. During the past 20 years, only 4 cases of isolated pulmonary involvement have been reported in literature, with one of lung cavity with pleural effusion. Pleural effusion as the main performance is making these cases unique because the usual manifestation of cysticercosis in lungs is presence of pulmonary nodules.
Case presentation
Case 1
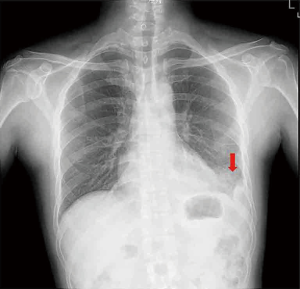
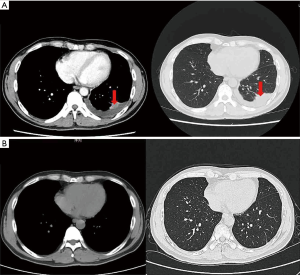
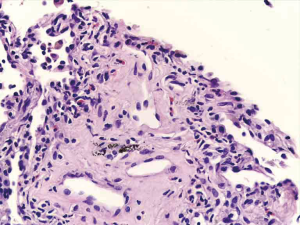
A 47-year-old man presented with complaints of the left chest pain and tightness for a week. The pain was dull aching and continuous with the back radiation. Chest X-ray PA view revealed left pleural effusion (Figure 1). He was started on using of levofloxacin injection in the local hospital. He showed no response to 1 week of antibiotic therapy. A chest ultrasound examination revealed the amount of pleural effusion. Two months earlier he had a pleural effusion and did not review after a pleural puncture pumping liquid treatment. He has no history of any chronic medical illness. Physical examination revealed decreased breathing sounds in his lower left lung to auscultation. The remainder of the examination was unremarkable. Investigations revealed an Hb of 14.1 g/dL, total leucocyte count of 6,100 cells/cu.mm, with neutrophils 43.1%, lymphocytes 35.4%, eosinophils 11.8% and monocytes 8.8%. The erythrocyte sedimentation rate was 29 mm/h. CRP was 30.1 mg/L, Routine biochemical investigations revealed normal glucose levels and renal and liver function tests. ANA was negative. Tests for human immunodeficiency virus 1 and hepatitis B surface antigen and hepatitis C virus were negative. Electrocardiogram was normal. Sputum for acid-fast bacilli was negative. PPD-test was negative. Full set of tumor markers were all normal. Defecate normal looking with no eggs. USG guided aspiration of around 280 mL of Pale yellow-colored pleural fluid was done from the pleural space which revealed protein of 4.7 mg/dL, albumin (ALB) 3.0 mg/dL, lactate dehydrogenase (LDH) 384 U/L, sugar 115 mg/dL, adenosine deaminase (ADA) of 14 IU/L, differentials showing 18% lymphocytes, 41% eosinophils, 6% monocytes and rest neutrophils. CEA 1.48 mg/mL. Chest CT scan (Figure 2) revealed left pleural effusion (22 mm thick) with atelectasis and a 12×20×25 mm3 high density seepage nodule was seen in the posterior basal segment of the left lower lobe, which is low reinforcement, the borderline between nodule and pulmonary atelectasis areas is clearly defined (Figure 2A). CT-guide percutaneous lung puncture from the nodule revealed a small amount of lung tissue and eosinophil infiltration (Figure 3). Serum IgG antibodies (ELISA) for cysticercosis returned positive. Magnetic resonance imaging (MRI) of brain and eye was then done and no evidence of cysticercosis infection was found in other sites. He has a history of eating pork and only has one chopping board in his home. He was then treated with praziquantel (60 mg/kg/day for 3 days) and with oral Dexamethasone tablets 1.5 mg given for 3 days to contain the inflammatory response caused by dead cysticerci. After 3 days of praziquantel therapy, the patient showed drastic improvement both clinically as well as with laboratory index. Both his Peripheral blood and pleural effusion of eosinophils returned to normal. Chest CT after 4 weeks of therapy showed the pleural effusion and the pulmonary shadow were almost fully absorbed (Figure 2B). Chest CT check after half a year was normal.
Case 2
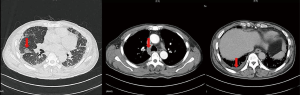
A 57-year-old man was admitted to our department with complaints of recurrent chest tightness for 20 days, he was an office worker and no other disease history. At the local hospital, the chest CT revealed multiple patchy infiltrating shadows especially in the peripheral zone of lower lung. The lymph nodes are slightly enlarged. Thickened interlobular septa are visible in the bilaterally subpleural. A small amount of pleural effusion in both side (Figure 4). He showed no response to 2 weeks of antibiotic therapy. A physical examination showed decreased breathing sounds in his lower right lung to auscultation. In addition, routine blood eosinophilic cells in moderately elevated (15.8%, the absolute value of 0.94×109/L), his other routine blood examination was normal. Under the bronchoscope lavage fluid examination, eosinophilic cells showed a significant increase (45%). Serum IgG antibodies (ELISA) for cysticercosis came out to be positive. Cysticercosis common infringement of site assessment, including the head, eyes, skin, etc., found no lesions. He was then treated with praziquantel (60 mg/kg/day for 3 days) and with intravenous injection of dexamethasone injection of 5 mg for 3 days. His clinical symptoms improved rapidly. Chest-CT check after 4 weeks found that his lesions had been completely absorbed.
Discussion
Cysticercosis, the infection by the larval stage of the tapeworm Taenia solium, is a serious public health problem in several countries in Latin America, Asia, and Africa - especially in developing countries (1,2). Infection occurs by the ingestion of tapeworm larvae via contaminated food, water or improperly cooked pork. Auto infection can also occur in humans by reverse peristalsis. This disease also has a feco-oral route of transmission (3). The coating around the eggs is dissolved by the gastrointestinal tract, allowing them to enter the bloodstream via the hepatoportal system to the tissues and organs of the body (4). Larvae remain viable for years, and multiple mechanisms of host immune tolerance have been postulated. The cystic larvae (cysticerci) develop in multiple sites but are commonly found in the central nervous system (brain, spinal cord) and skeletal muscle. The heart, lungs or the other tissues are occasionally affected. The clinical features depend on the location of the cysticerci, the cysticerci burden and the host reaction (5). The rarity of pulmonary involvement by cysticerci can be explained by the life cycle of Taenia solium parasite. Humans may be an intermediate host for the adult larvae which mostly favors muscle and brain tissue to complete their life cycle. Another theory is that the lung cysticercosis are rarely in clinical related six hooks difficult to larva through blood-gas barrier (6). Moreover, pulmonary involvement is mostly overlooked because the patient usually presents with neurological symptoms and other clinical features which are more prominent. The radiological appearance of cysticercus lesions mimics many other diseases. The lung damage is mainly located in the middle and lower lateral zone and under the pleural membrane. This is because microvascular rich in these places. The relatively narrow diameter and the slow flow of blood, which is conducive to the retention of the Six hook larva. Six hooks larvae just stay period. Local lesions produce inflammation, seepage, stimulate the pleural effusion formation. After developed into cysticercoid, it would Stimulate local fiber package formation and then formation of nodules (7). This is a process that constantly stimulates the formation of the eosinophil infiltration and pleural effusion. Perhaps the closer the lesion is to the pleura, the longer the stimulation time, the more breast water. But no relevant documents have been found. Diagnostic criteria per “Harrison’s principles of internal medicine” textbook is by demonstration of cysticerci through histologic or microscopic examination of biopsy material (absolute criteria) and by demonstration of antibodies to cysticerci in serum by enzyme linked immunoelectrotransfer blot (major criteria). Lesions responding to albendazole (15 mg/kg) or praziquantel therapy (50 mg/kg) is also one of the major diagnostic criteria for diagnosis of cysticercosis (8). Salaria et al. had reported one case of an unknown association of eosinophilia, pleural effusion and cysticercosis in 2001 (9). Until now only one case of isolated pulmonary involvement in cysticercosis is available on PUBMED and web of science searches (6). Referring to nearly 20 years of literatures domestically and abroad, including Wanfang database, PUBMED, MEDLINCE, etc., human infection with diffuse cysticercosis has more than 50 cases. However isolation lung cysticercosis reports are rare and only 4 cases were reported in literature (6,10-11). Most lung lesions were characterized by nodules. We access one case which was characterized with pulmonary cavity and pleural effusion by Gupta et al. in 2015 from PUBMED and Medline. But pleural effusion and exudative lesions is reported for the first time. In this paper, the main performance of the two cases was pulmonary effusion and exudative lesions. Eosinophilic cells were found to have an unusually high proportion in peripheral blood and pleural effusion or bronchial lavage. The serum cysticercosis IgG antibodies were positive. The source of infection in our two cases is not particularly clear, perhaps associated with bad living habits, such as only using one Chopping board in first case. Both have no basic diseases and atypical clinical symptoms, so they were misdiagnosed as other diseases at first. After anti-Parasitic infection treatment, symptoms improved significantly within a short time and lesions were completely absorbed 4 weeks after. In this paper, two cases were diagnosed by antibody detection and effective treatment, although no histologic diagnosis and microbiological diagnosis, but according to “Harrison’s principles of internal medicine”, the diagnosis was established. Through literature review we found that when unexplained eosinophilic cells increased to not ignore the possibility of parasitic infection, such as cysticercosis and so on.
To the best of our knowledge no cases of isolated pulmonary cysticercosis presenting as exudative lesions with pleural effusion have been reported in literature until now.
Acknowledgements
We thank the patients give us her consent for publication of this case.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patients for publication of this manuscript and accompanying images.
References
- Garcia HH, Del Brutto OH. Taenia solium cysticercosis. Infect Dis Clin North Am 2000;14:97-119. [Crossref] [PubMed]
- White AC Jr. Neurocysticercosis: updates on epidemiology, pathogenesis, diagnosis, and management. Annu Rev Med 2000;51:187-206. [Crossref] [PubMed]
- Muray PR, Rosenthal KS, Pfaller MA. Cestodes. In: Murray PR, editor. Medical Microbiology, 5th ed. USA: Elsevier Mosby, 2005:908
- Lam JC, Robinson SR, Schell A, et al. Pulmonary neuroendocrine carcinoma mimicking neurocysticercosis: a case report. J Med Case Rep 2016;10:144. [Crossref] [PubMed]
- Banu A, Veena N. A rare case of disseminated cysticercosis: case report and literature review. Indian J Med Microbiol 2011;29:180-3. [Crossref] [PubMed]
- Gupta N, Meena M, Harish S, et al. A rare case of pulmonary cysticercosis manifesting as lung cavity with pleural effusion. Lung India 2015;32:515-7. [Crossref] [PubMed]
- Pei Y, Deng D, Long L, et al. The performance of the X-ray of pulmonary cysticercosis. Chin J Radiol 2002;5:468-9.
- Braunwald E, Fauci AS, Kasper DL, et al. Harrison's Principles of Internal Medicine. 15th ed. Beijing: McGraw-Hill Professional Publishing, 2001:755:1185-6.
- Salaria M, Parmar V, Kochar S, et al. Eosinophilia, pleural effusion and cysticercosis--unknown association? Indian Pediatr 2001;38:671-4. [PubMed]
- Li J, Wang W. Misdiagnosis analysis in 3 cases of Lung cysticercosis with pulmonary symptoms. Journal of Pathogen Biology 2006;3:240.
- He Z. One case of lung cysticercosis misdiagnosed to tuberculosis. Guangdong Medical Journal 2006;10:1590.