Simultaneous unilateral anterior thoracoscopy with transcervical thyroidectomy for the resection of large mediastinal thyroid goiter
Introduction
Thyroid goiters with mediastinal extension are relatively common entities. In areas where iodine deficiency is common, up to 25% of thyroid goiters may have a retrosternal or substernal component (1). Thyroid goiter with mediastinal extension presents a unique challenge from the preoperatively planning and intraoperative management standpoint. Traditionally, endocrine surgeons have recommended resection for all large goiters whether symptomatic or asymptomatic. However, increased risk of complications for resection of larger goiters in asymptomatic patients, particularly those with significant mediastinal extension, has led some surgeons to take a less aggressive stance in the surgical management of these patients.
The vast majority of thyroid goiters with mediastinal extension may be resected via the standard transverse cervical collar incision approach by bluntly delivering the mediastinal component into the neck. Approximately 11% of mediastinal goiters require additional exposure of the mediastinum either via a thoracotomy or sternotomy in order to resect the goiter (2). In 5% to 37% of cases, thoracic exposure is required for resection of reoperative cases for recurrent or residual disease where simple cervical approach is not possible (3). The most common approach for mediastinal extension is a complete or partial sternotomy which carries with a non-insignificant morbidity including postoperative pain, mediastinitis, sternal dehiscence, bleeding, and infection.
Minimally invasive approaches to the thorax and mediastinum have gained popularity in recent years due to the decreased incidence of postoperative pain, bleeding and pulmonary morbidity associated with thoracoscopy in comparison to thoracotomy and sternotomy. Thoracoscopy and more recently, robotic assisted thoracoscopy have been used with increasing frequency to approach lesions in the mediastinum. Thoracoscopy allows excellent access to the anterior, middle, and posterior compartments of the mediastinum. Whereas a sternotomy provides adequate exposure of the anterior mediastinum, it does not provide adequate exposure of the posterior and middle mediastinal compartments. Therefore, goiters with retrotracheal, paratracheal, para-aortic, and retroesophageal extension would best be approached by a thoracotomy or thoracoscopy. Al-Mufarrej et al. described two cases of combined mediastinal goiter resection using robotic assisted lateral thoracoscopy for mobilization followed by patient repositioning and cervical exploration for completion of resection. This did not add significantly to operative time and limited the morbidity of combined cervical exploration and median sternotomy (4). The limitation of this approach is the need to reposition the patient intraoperatively.
We typically approach mediastinal masses via anterior thoracoscopy in the inframammary crease. We found this approach to be versatile for excellent access to all compartments of the mediastinum without the need for patient repositioning and have found that mediastinal goiters can easily be approached this way as well with simultaneous cervical exploration. We present here our experience with seven consecutive patients with large mediastinal goiters with variable mediastinal extension who underwent resection via a simultaneous combined cervical exploration and unilateral anterior thoracoscopy.
Methods
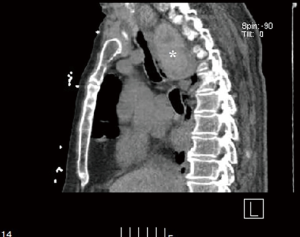
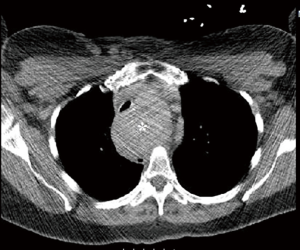
Patients
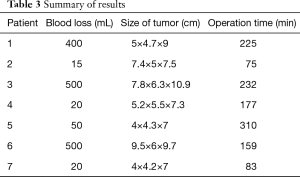
Institutional review board exemption was obtained prior to commencing this study (IRB 2014-12-15). Consent from the patient was not required because the information is recorded by the investigator in such a manner that research participants cannot be identified, directly or through identifiers linked to the research participant. Between 2012 and 2015, 280 thyroidectomies were performed of which 45 (16%) had a retrosternal component. Thirty-nine out of 45 (86%) retrosternal goiters were anterior mediastinal, only one of which required thoracoscopy. Six of 45 (13%) were middle/posterior mediastinal. Out of 7 retrosternal goiter that required thoracoscopic approach, 1 was anterior mediastinal and 6 were middle/posterior mediastinal. Seven patients with large mediastinal goiters, particularly those with atypical mediastinal extension (paratracheal, retroesophageal, etc.) were evaluated by a thoracic surgeon preoperatively and selected for simultaneous unilateral thoracoscopy and cervical thyroidectomy (Table 1, Figures 1,2) . Patient age range was 57 to 91. Six of the patients were female. Only one of the patients had clinical hyperthyroidism while the remainder of patients was euthyroid. Two patients had goiters that extended into the right paratracheal region, two patients had goiter extension to the left paratracheal/subaortic region, one patient had goiter extension to the retrotracheal region and one patient had extension of the left thyroid lobe to the right hemithorax via the retroesophageal plane. The last patient had a large substernal calcified thyroid goiter extending from the left lobe. Seven patients had respiratory symptoms with stridor and tracheomalacia. Two patients required perioperative mechanical ventilation and one required an emergency tracheostomy on presentation. The patient with a retroesophageal goiter also had symptoms of dysphagia. The patient with clinical hyperthyroidism presented with new onset atrial fibrillation. None of the patients had malignancy. All patients underwent preoperative stabilization prior to elective resection.

Full table
Surgical procedures
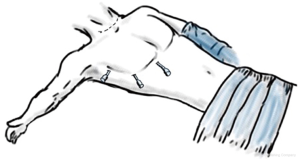
All patients were positioned supine with a shoulder roll beneath the scapulae with the neck extended. When feasible, a double lumen endotracheal tube was used with full lung isolation. When a tracheostomy was present, the tracheostomy tube was removed and the patient was intubated with a single lumen endotracheal tube and a bronchial blocker with single lung ventilation. The patient’s upper extremity on the side of surgery was abducted 45 degrees. The endocrine surgery team was positioned cephalad to and the thoracic surgery team was positioned caudad to the upper extremity, the latter with surgeon and assistant on the same side. Mediastinal goiter was approached via a right anterior thoracoscopy in four of the patients and via the left in three patients.
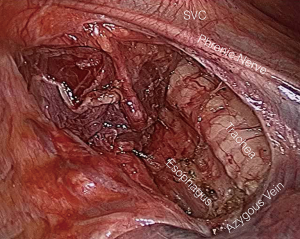
Anterior thoracoscopy and cervical exploration were begun simultaneously. Cervical exploration was performed through a standard transverse collar incision in all cases. Anterior thoracoscopy was performed using three 5-mm ports along the inframammary crease (Figure 3). Visualization and exposure was augmented using carbon dioxide insufflation to a pressure of 8 mmHg. The mediastinal thyroid goiter was easily identified in all cases and exposed by dividing the overlying mediastinal pleura. After mediastinal pleura were opened, sharp dissection was used to separate the goiter from mediastinal structures. Once adhesions to the thyroid capsule were freed, the goiter was delivered bluntly. Vessels were encircled as necessary in order to provide countertraction for goiter dissection. However, gentle traction and manipulation of the goiter alone allows for a safe mediastinal dissection. Care was taken to avoid violation of the thyroid capsule. After all the structures were dissected up to the thoracic inlet, then traction from the cervical incision was applied to pull the specimen through the thoracic inlet safely and under direct vision (Figures 4,5).
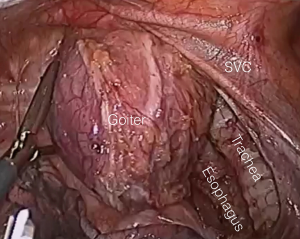
Once the mediastinal goiter was delivered through to the cervical incision, the lung was re-expanded and pleural space drained with a small bore chest drain brought out through a port site. Transcervical thyroidectomy was completed in standard fashion. The thoracic drain was removed the following day in all patients.
Results
The mediastinal goiter was able to be completely resected in all patients. Three patients underwent thyroid lobectomy and the remaining patients underwent subtotal thyroidectomy. These procedures were performed largely for aerodigestive obstructive symptoms associated with the goiter. Subtotal thyroidectomy was performed in order to remove as much as necessary in order to alleviate the symptoms and preserve parathyroid function. Mediastinal goiter recurrence is unlikely. Pathology confirmed non-toxic nodular goiter in all patients.
The addition of anterior thoracoscopy did not increase the length of the procedures. In all cases, the thoracoscopic portion of the procedure starts at the time of cervical incision and is completed after the goiter is delivered through the cervical incision. At no time was there a delay or idle time during the transcervical thyroidectomy while waiting for the thoracoscopic mobilization of the mediastinal goiter to be completed. Therefore, operative time was determined by the complexity of the cervical portion of the operation. No comparison can be made to other cases in which thoracoscopy was not used for this reason.
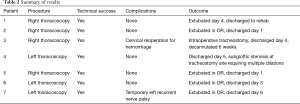
There were no postoperative mortalities. There were no pulmonary or mediastinal injuries in any of the patients. One patient required cervical re-exploration for hemorrhage on the first postoperative day. Cervical venous bleeding was identified and controlled without any transfusion requirement. One patient had transient postoperative hoarseness with evidence of left recurrent nerve palsy which resolved within 4 weeks of surgery. None of the remaining patients had any procedure related complications.
Three patients were primarily extubated at the conclusion of the procedure. The third patient was found to have significant tracheomalacia at cervical exploration and underwent elective tracheostomy placement at the conclusion of resection. That patient was subsequently decannulated as an outpatient 6 weeks postoperatively. The patient with a retroesophageal goiter was electively extubated on the fourth postoperative day with resolution of his dysphagia symptoms. The patient who underwent emergency tracheostomy has subsequently undergone multiple endoscopic dilation and laser ablation procedures for a subglottic stenosis at the tracheostomy site and is planned for future decannulation. The results are summarized in Tables 2 and 3.
Full table
Full table
Discussion
Intrathoracic or mediastinal goiters comprise 6 to 30% of all thyroid goiters (5). Of these, 75 to 90% extend to the anterior mediastinum retrosternally while 5 to 25% extend into the posterior mediastinum frequently extending along the paratracheal plane or along the tracheoesophageal groove (6,7). Rarely, the mediastinal goiter can take a retrotracheal and retroesophageal path as it enlarges. Symptoms are based on anatomic location and can range from no symptoms to dyspnea with stridor from tracheal compression and dysphagia from esophageal compression.
Approximately 90% of anterior mediastinal goiters may easily be resected through a transcervical approach (8). This is particularly true of goiters that extend into the immediate retrosternal space and have no extension or involvement of the middle or posterior mediastinal compartments. However, deep mediastinal extension and involvement of and adherence to critical vascular or aerodigestive structures present a challenge to the thyroid surgeon. Conventional exposure to allow safe dissection of and delivery of these goiters requires either a sternotomy or a high thoracotomy. Madjar et al. performed 40 thyroidectomies for mediastinal goiter over a 22-year period with 4 patients requiring a sternotomy and 2 patients with retroesophageal goiters requiring a posterolateral thoracotomy for resection (8). DeAndrade et al. performed sternotomy with high thoracotomy in 6 of 128 patients, all of which had goiters with significant posterior mediastinal extension (9).
A sternotomy allows for excellent exposure to the anterosuperior mediastinum and the great vessels. For retrosternal goiters, a complete or even a partial sternotomy to the second intercostal space allows for safe dissection of the goiter from innominate vessels and pericardium. A partial sternotomy is ideal in that the complications of sternal dehiscence, mediastinitis, hemorrhage and pain, are minimized when compared to a full median sternotomy. However, sternotomy provides limited access to middle and posterior mediastinal compartments. Only a high thoracotomy would provide adequate access to these areas at the expense of pain, pulmonary morbidity and the need for intraoperative patient repositioning. There is no hard pre-operative indication for sternotomy. Yet, preoperative clinical and radiologic factors can help predict the need for sternotomy or thoracotomy. Harder thyroid tissue density, posterior mediastinal extension, sub-carinal location, dumbbell shape, thoracic component larger than thoracic inlet increases the chance of sternotomy, therefore these patients should be counseled preoperatively for thoracoscopy (10) (McKenzie & Rook, 2014). In our case, all retrosternal goiters with a significant mediastinal component, particularly with middle/posterior mediastinal extension or extension to level of carina or aortic arch were selected for simultaneous thoracoscopic and cervical approach. These were consecutive cases and as such, the decision to perform combined cervical and thoracoscopic approach was determined preoperatively by both surgical teams. In no case did intraoperative findings change the operative approach. We had no conversion to sternotomy or thoracotomy during the study period.
The desire for a minimally invasive approach to mediastinal goiter access is driven by the extensive added morbidity of the open thoracic approach. The advent of thoracoscopy has minimized postoperative pain, pneumonia, and pulmonary complications. Data from pulmonary resections comparing thoracotomy with thoracoscopy showed a 45% complication rate and 3.6% mortality rate versus a 28% complication rate and 0% mortality rate respectively (11).
Standard lateral thoracoscopy is performed with the patient in a lateral decubitus position. While this approach allows excellent access to the lungs and as well as the mediastinum, it is limited in exposure to the anterior mediastinum and there is a need for intraoperative patient repositioning for cervical exploration. With anterior thoracoscopy, access to lower thoracic structures is limited but full access to the mediastinum is possible while allowing for two surgical teams to work simultaneously, therefore limiting anesthesia time. We were able to perform all dissection of the goiter with unilateral approach but if difficult, bilateral thoracoscopic approach can be performed for further mobilization but is often unnecessary. We have found that the side of thoracoscopy should be the side of the lobe of the thyroid with the mediastinal extension. This is particularly true with goiters in the paratracheal and posterior mediastinal extension. Bilateral thoracoscopy may be beneficial in the setting of crossover of the goiter to the contralateral side. This was the case in our first patient who had a goiter extending from the left thyroid lobe and crossing over into the right hemithorax in a retroesophageal fashion. However, in this case, a right thoracoscopic approach provided excellent exposure for separation of this goiter from the posterior esophagus to the thoracic inlet.
To date, there have only been four cases reported of mediastinal goiters resected with thoracoscopy (4,12,13). The first three cases utilized robotic assisted thoracoscopy to mobilize large posterior mediastinal goiters in the lateral decubitus position prior to repositioning and transcervical resection. The robotic approach, even if done as an anterior thoracoscopy is limited by the bulk of the da Vinci robot and inability of a second surgical team to perform a cervical exploration simultaneously. Bhargav et al. described a case of a goiter with significant posterior mediastinal extension that was unable to be delivered through the transcervical approach. Intraoperative right anterior thoracoscopy was performed in order to deliver the goiter into the cervical incision (13). To our knowledge, this is the first case series of elective simultaneous anterior thoracoscopy and transcervical resection for large mediastinal goiters.
Conclusions
Simultaneous unilateral anterior thoracoscopy in the inframammary crease and transcervical thyroidectomy has shown to be a safe and effective technique for the resection of large thyroid goiters with significant mediastinal extension without adding significant morbidity to the procedure. The technique does not add any additional operative time to the procedure and may in fact decrease procedure time by facilitating transcervical delivery of the mediastinal component of the goiter. We believe that mediastinal goiters, particularly posterior mediastinal goiters, may be approached this way electively if there are any question as to the resectability of these goiters by transcervical approach alone exists preoperatively.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: Institutional review board exemption was obtained prior to commencing this study (IRB 2014-12-15). Consent from the patient was not required because the information is recorded by the investigator in such a manner that research participants cannot be identified, directly or through identifiers linked to the research participant.
References
- Katlic MR, Wang CA, Grillo HC. Substernal goiter. Ann Thorac Surg 1985;39:391-9. [Crossref] [PubMed]
- Huins CT, Georgalas C, Mehrzad H, et al. A new classification system for retrosternal goitre based on a systematic review of its complications and management. Int J Surg 2008;6:71-6. [Crossref] [PubMed]
- White ML, Doherty GM, Gauger PG. Evidence-based surgical management of substernal goiter. World J Surg 2008;32:1285-300. [Crossref] [PubMed]
- Al-Mufarrej F, Margolis M, Tempesta B, et al. Novel thoracoscopic approach to posterior mediastinal goiters: report of two cases. J Cardiothorac Surg 2008;3:55. [Crossref] [PubMed]
- Cichoń S, Anielski R, Konturek A, et al. Surgical management of mediastinal goiter: risk factors for sternotomy. Langenbecks Arch Surg 2008;393:751-7. [Crossref] [PubMed]
- Chong CF, Cheah WK, Sin FL, et al. Posterior mediastinal goiter. Asian Cardiovasc Thorac Ann 2004;12:263-5. [Crossref] [PubMed]
- Cho HT, Cohen JP, Som ML. Management of substernal and intrathoracic goiters. Otolaryngol Head Neck Surg 1986;94:282-7. [Crossref] [PubMed]
- Madjar S, Weissberg D. Retrosternal goiter. Chest 1995;108:78-82. [Crossref] [PubMed]
- De Andrade MA. A review of 128 cases of posterior mediastinal goiter. World J Surg 1977;1:789-97. [Crossref] [PubMed]
- McKenzie GA, Rook W. Is it possible to predict the need for sternotomy in patients undergoing thyroidectomy with retrosternal extension? Interact Cardiovasc Thorac Surg 2014;19:139-43. [Crossref] [PubMed]
- Cattaneo SM, Park BJ, Wilton AS, et al. Use of video-assisted thoracic surgery for lobectomy in the elderly results in fewer complications. Ann Thorac Surg 2008;85:231-5; discussion 235-6. [Crossref] [PubMed]
- Podgaetz E, Gharagozloo F, Najam F, et al. A novel robot-assisted technique for excision of a posterior mediastinal thyroid goiter: a combined cervico-mediastinal approach. Innovations (Phila) 2009;4:225-8. [Crossref] [PubMed]
- Bhargav PR, Bhagat SD, Kishan Rao B, et al. Combined Cervical and Video-assisted Thoracoscopic Thyroidectomy (CAVATT): A Simplified and Innovative Approach for Goiter with Posterior Mediastinal Extension. Indian J Surg 2010;72:336-8. [Crossref] [PubMed]


