The introduction of electromagnetic navigation bronchoscopy for the diagnosis of small pulmonary peripheral lesions in an Asian population
Introduction
The diagnosis of early stage lung cancer, especially small pulmonary peripheral lesions (SPPLs), has great significance for increasing the percentage of operable lung cancer lesions and improving patients’ life quality (1). With advances made in diagnostic techniques, the detection rate of SPPLs has gradually increased. The accurate diagnosis of SPPLs, which requires and places a higher demand on pulmonary doctors and techniques, can greatly improve the early diagnosis rate of lung cancer (2). However, the current diagnostic techniques for SPPLs are still far from satisfactory. The main limitations include low accuracy and precision, frequent complications, and the requirement of a large incision.
The emergence of electromagnetic navigation bronchoscopy (ENB) (3-5), a key breakthrough in the diagnosis of SPPLs, provided a solution to this problem. This image-guided localization device could reportedly reach the peripheral lung lesions and obtain biopsy tissues (6,7). Thus far, however, the results, and ramifications of the benefits of ENB are still under debate (8). The accuracy and efficiency of ENB in the diagnosis of SPPLs has not been investigated in Asian populations. Shanghai Pulmonary Hospital (Tongji University), the first hospital in Asia carrying ENB technology, has already diagnosed several cases using ENB. In this study, the performance of ENB in a Chinese population was accessed through a retrospective study.
Methods
Ethical approval, consent and permissions
The protocol of this study was conducted according to the revised Declaration of Helsinki and approved by the Institutional Review Board (IRB) of Shanghai Pulmonary Hospital (Tongji University) (No. 2013-007). Informed consent was obtained from all participants.
Patients
Consecutive SPPL patients from our department who had indications were recruited into this study from May 2014 to April 2015. The conditions of these patients were discussed at department meetings; the decision to proceed with ENB was authorized by the Department Chief. A positive bronchus sign was a prerequisite for our ENB operation. Patients with the following conditions were excluded: (I) myocardial infarction or cardiothoracic surgery within 3 months; (II) hemoptysis within 2 weeks; (III) cardiopulmonary insufficiency; (IV) unstable angina; (V) coagulation disorders; (VI) lesions in the lumen; or (VII) the presence of chest pain.
ENB operation
The protocol followed the recommendations of the manufacturer and a previous report (9). The version number of the SuperDimension system used is 6.1.3. Prior to the ENB operation, a chest CT scan was used to generate a 3D channel. During the initial planning phase, the CT scan data was loaded into the manufacturer’s software (SuperDimension). At least five anatomical marks were chosen as the virtual reference points. The operation was performed through a laryngeal mask airway under general anesthesia. The CT images and 3D virtual airways were linked to the controllable probe with the help of the preset landmarks in patient’s airways. The steerable guide catheter of SuperDimension was inserted through the working channel of the scope. We monitored the operation through R-EBUS and X-ray and confirmed that the bronchoscopist was at the lesion. If the bronchoscopist did not reach the lesion, two more attempts to reach it were made. After confirming arrival at the lesion, tissue sampling was prepared for biopsy through brush biopsy, biopsy forceps biopsy or fine-needle aspiration biopsy.
To assure accuracy, registration errors were calculated using computer software. These errors represented the radius of the expected difference between the tip of the sensor probe and its expected location in the patient. Further, a navigation error was defined as the discrepancy in the distance between the sensor probe and the lesion. Navigation was deemed successful if the specified distance was less than 10 mm from the lesion.
Clinicopathological features
Confirmation of the final diagnosis was ascertained through a histopathological examination in all cases. Diagnostic yield, lesion size, shape, and location, and complications were documented. The follow-up of all patients was 12 months or more.
Statistical analysis
χ2 test was used to analyze the associations between the variables. All data were calculated by the SPSS. A P value <0.05 was considered statistically significant.
Results
Patients’ information
ENB was performed on 78 consecutive patients during the twelve months specified (Table 1). They had 84 SPPLs (four patients had more than one SPPL). Most patients were male. The average age was 53.52 years old (range, 24–82 years). Most lesions were detected in the upper lobes [22 located in the left upper lobe (LUL) and 35 in the right upper lobe (RUL)].
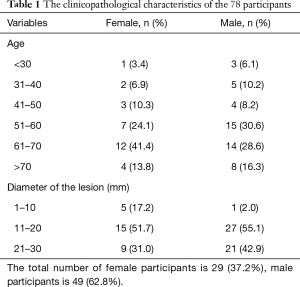
Full table
Efficiency
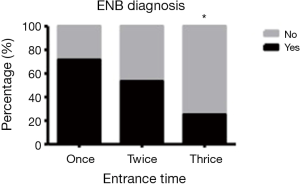
When ENB was applied in clinical practice, its efficiency was the first indicator we wanted to analyze. The ENB navigation successfully reached 81 lesions (39 were reached in the first attempt, 30 lesions were reached after two attempts and 12 needed three tries to reach the lesion during the same operation) of 75 patients. The mean diameter of these lesions was 19±6.16 mm. The number of attempts correlates with whether the ENB procedure would make the diagnosis (Figure 1). The diameter of the lesions did not affect the number of attempts. Adequate biopsy samples were harvested after reaching the lesions. The ENB navigation took an average of 10.8 minutes to complete. Timing was more efficient when it succeeded on the first attempt. However, the complications of bleeding and pneumothorax all occurred in groups that needed shorter navigation times. Therefore, whether the ENB procedure would make a diagnosis was not affected by the navigation time (Figure 2). The navigation failed in three cases. The distance between the sensor probe and the lesion was 8.02±2.85 mm in average. The sensor probe was mostly located within 8 mm from the lesion. It was affected by the diameter of the lesion. Furthermore, the volume of the lesion did not affect the navigation time, the number of attempts, or the occurrence of complications (Figure 3).


Accuracy and safety
The diagnosis accuracy and safety of ENB was another crucial concerns when it was applied in practice. Our results suggested that ENB diagnosis had identical results with histopathology examination in 78 lesions (37 lung cancer and 41 non-lung cancer) (Table 2). The sensitivity of ENB was 92.86% (78 out of 84 lesions) in this study. The diagnosis of non-malignant lesions included non-specific inflammation, granuloma gangraenescens, tuberculosis and atypical hyperplasia. The three falsely diagnosed lesions by ENB were fiber connective tissue hyperplasia in the pathological analysis. Complications, including one case of bleeding and one pneumothorax, were reported in two patients.
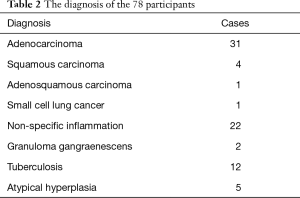
Full table
Discussion
The malignancy rate for small periphery lesions (between 0.8 and 2.0 cm) was previously reported to be approximately 18% (10). Underscoring the potential benefit of the diagnosis and treatment of early stage lung cancer, evaluation of SPPLs highlights the importance of the pulmonologist’s early and accurate diagnosis. However, the early and accurate diagnosing process, and the imaging instruments now used are still particularly challenging for clinicians.
Presently, reaching the lesion and successfully obtaining adequate biopsy tissue samples remains a difficult task. The conventional diagnostic technology, including bronchoscopy, has not been suitable for SPPLs. Currently, suspicious SPPLs are often biopsied using more invasive methods, such as CT-guided aspiration (which increases the risk of pneumothorax) or surgical biopsy. Thus a new, more accurate yet less invasive, diagnostic process is needed.
The introduction of ENB contributes to providing an accurate, navigational and steerable technique to localize small lung lesions. This new technology has been successfully used on animal models since 2003; the first human study was performed in 2005; and to date, over 20,000 procedures have been performed (4,11). During the procedure, ENB-aided diagnostics yielded approximately 75% accuracy and the occurrence of pneumothorax was less than 5% in most studies (12). Thus far, it has become a most suitable assessment tool for SPPLs.
One of the main practical advantages of ENB is the detection of peripheral lesions in upper lobes, which are less detectable through CT scan-guided biopsies. The three greatest advantages of ENB are as follows: (I) it is less invasive; (II) it is more comfortable; and (III) it develops minimal complications. Furthermore, ENB guarantees on-site examination, which significantly improves the accuracy of diagnosis while also decreasing operative time. It is also conducive to improving the skills of the bronchoscopist.
To the best of our knowledge, no report has ever assessed the efficiency and safety of ENB among Asian patients. To answer this question, we designed this study following previously reported instructions (12). Three physicians from our hospital have been using ENB since 2013. It is an efficient and manageable technology. There was no significant difference among operators. We did not set up many thresholds except for a positive bronchus sign in the inclusion criteria. We analyzed both the efficiency and safety of ENB in this study. We were most concerned about the efficiency indicators. We employed ENB procedures deemed medically expedient and efficient. Suspect small lung cancer lesions were difficult to reach by conventional techniques; however, ENB provided a less invasive method to reach and extract sample tissue. In our study, most lesions were accurately determined by the magnetic field of the ENB procedure. ENB diagnosis could be potentially affected by navigation time, attempt frequency, and actual navigation error. In the current study, ENB diagnosis also yielded several non-malignant diagnoses, which were confirmed by pathological examination and followed up.
Effective treatment plans for lung cancer depend on accurate, histologic classification. Presently, lung cancer treatment is based on the histologic subtyping of NSCLC (13,14). Our study strongly suggests that ENB is an outstanding technique that can aid pulmonary physicians in small lung lesions diagnosis. With the assistance of ENB, the samples of 81 lesions were successfully biopsied; normally these are not accessible by routine instruments. Our data also suggested that the diagnostic accuracy of ENB was reliable. It was concordant with the pathological results in 92.86% (78 out of 81) of lesions. The early diagnosis would greatly improve accurate, timely, and successful treatment. In addition to these positive factors, these ENB procedures were deemed satisfactorily safe, which mirrored the previous report (15,16). During the study, only two complications appeared in our participants.
We realize that two factors limited our study: first, our overall actual number of cases was limited; second, the specific groups such as automated implantable cardioverter-defibrillator patients, who also had successful guidance by ENB (17), were excluded. We will continue to monitor the efficiency and safety of ENB in the future.
Conclusions
In conclusion, our experience using ENB indicated that this procedure was both efficient and accurate for the diagnosis of SPPLs. ENB also provided a practicable method for the bronchoscopist to address the SPPLs. Finally, ENB appears to have performed very well in both navigating and aiding in the diagnosis of SPPLs in this Asian population.
Acknowledgements
We appreciate the patients and their families for participating in this study.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The protocol of this study was conducted according to the revised Declaration of Helsinki and approved by the Institutional Review Board (IRB) of Shanghai Pulmonary Hospital (Tongji University) (No. 2013-007). Informed consent was obtained from all participants.
References
- International Early Lung Cancer Action Program Investigators, Henschke CI, Yankelevitz DF, et al. Survival of patients with stage I lung cancer detected on CT screening. N Engl J Med 2006;355:1763-71. [Crossref] [PubMed]
- Krimsky W, Seijo LM. Bronchoscopy and the peripheral nodule in the age of lung cancer screening and targeted therapies. Curr Respir Care Rep 2012;1:67-71. [Crossref]
- Lamprecht B, Porsch P, Wegleitner B, et al. Electromagnetic navigation bronchoscopy (ENB): Increasing diagnostic yield. Respir Med 2012;106:710-5. [Crossref] [PubMed]
- Leong S, Ju H, Marshall H, et al. Electromagnetic navigation bronchoscopy: A descriptive analysis. J Thorac Dis 2012;4:173-85. [PubMed]
- Mahajan AK, Patel S, Hogarth DK, et al. Electromagnetic navigational bronchoscopy: an effective and safe approach to diagnose peripheral lung lesions unreachable by conventional bronchoscopy in high-risk patients. J Bronchology Interv Pulmonol 2011;18:133-7. [Crossref] [PubMed]
- Bechara R, Parks C, Ernst A. Electromagnetic navigation bronchoscopy. Future Oncol 2011;7:31-6. [Crossref] [PubMed]
- Ha D, Choi H, Almeida FA, et al. Histologic and molecular characterization of lung cancer with tissue obtained by electromagnetic navigation bronchoscopy. J Bronchology Interv Pulmonol 2013;20:10-5. [Crossref] [PubMed]
- Chee A, Stather DR, Maceachern P, et al. Diagnostic utility of peripheral endobronchial ultrasound with electromagnetic navigation bronchoscopy in peripheral lung nodules. Respirology 2013;18:784-9. [Crossref] [PubMed]
- Quinn CC. Diagnostic approach to pulmonary nodules in the postpneumonectomy patient. Semin Thorac Cardiovasc Surg 2010;22:345-8. [Crossref] [PubMed]
- Leef JL 3rd, Klein JS. The solitary pulmonary nodule. Radiol Clin North Am 2002;40:123-43. [Crossref] [PubMed]
- Schwarz Y, Greif J, Becker HD, et al. Real-time electromagnetic navigation bronchoscopy to peripheral lung lesions using overlaid CT images: the first human study. Chest 2006;129:988-94. [Crossref] [PubMed]
- Folch EE, Bowling MR, Gildea TR, et al. Design of a prospective, multicenter, global, cohort study of electromagnetic navigation bronchoscopy. BMC Pulm Med 2016;16:60. [Crossref] [PubMed]
- Bulman W, Saqi A, Powell CA. Acquisition and processing of endobronchial ultrasound-guided transbronchial needle aspiration specimens in the era of targeted lung cancer chemotherapy. Am J Respir Crit Care Med 2012;185:606-11. [Crossref] [PubMed]
- Cooper WA, O'toole S, Boyer M, et al. What's new in non-small cell lung cancer for pathologists: the importance of accurate subtyping, EGFR mutations and ALK rearrangements. Pathology 2011;43:103-15. [Crossref] [PubMed]
- Seijo LM, de Torres JP, Lozano MD, et al. Diagnostic yield of electromagnetic navigation bronchoscopy is highly dependent on the presence of a Bronchus sign on CT imaging: results from a prospective study. Chest 2010;138:1316-21. [Crossref] [PubMed]
- Brownback KR, Quijano F, Latham HE, et al. Electromagnetic navigational bronchoscopy in the diagnosis of lung lesions. J Bronchology Interv Pulmonol 2012;19:91-7. [Crossref] [PubMed]
- Khan AY, Berkowitz D, Krimsky WS, et al. Safety of pacemakers and defibrillators in electromagnetic navigation bronchoscopy. Chest 2013;143:75-81. [Crossref] [PubMed]


