A case report of giant esophageal neurofibroma
Introduction
Benign esophageal tumors are rare in comparison to esophageal malignancies. Attah found only 26 cases of benign esophageal tumors in a 30-year review of 15,454 autopsies, with a prevalence of 0.17% (1). Leiomyoma is the most common benign esophageal tumor in both surgical and autopsy series, while hemangioma, hamartoma and neurofibroma are rarely seen (2). Neurofibromas are generally associated with hereditary diseases and usually have a manifestation of von Recklinghausen disease (VRD) (3). Sex hormones play a potential role in etiology, and the male preponderance was found (4). About half of the patients with benign esophageal tumor are asymptomatic. Smaller lesions are detected accidentally, while the larger ones can cause compressive symptoms. Variety of surgical treatments has been reported to remove these lesions (5-7). Successful surgical resection of the giant neurofibroma forms the basis of present report.
Case presentation
A 63-year-old Chinese man was admitted to our hospital because of dysphagia, belching and retrosternal pain for over half a year. He has been hypertensive for 5 years and has been on antihypertensive medication for that time. His family history was unremarkable. Results of his physical and systemic examination were normal.
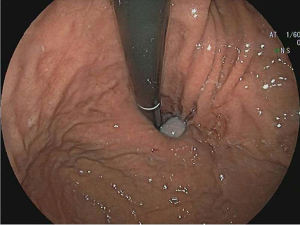
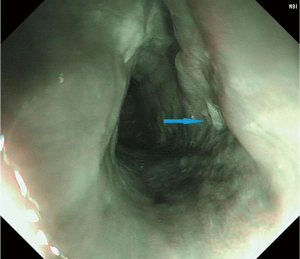
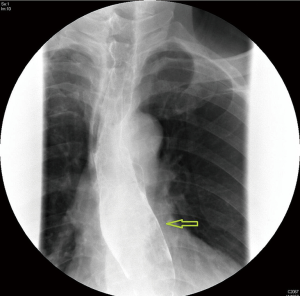
Upper gastrointestinal tract endoscopy disclosed a giant submucosal mass with a smooth surface that was located 18 to 40 cm from the incisors. Multiple biopsy specimens revealed inflamed mucosa with hyperaemia. There was no evidence of malignancy. Ultrasonic gastroscopy disclosed a giant protrusion of the esophagus located 18 cm from the incisors that originated from the submucous and was suspected to be a neurofibroma because of its homogeneous and hypoechoic lesion with clear margins. Distal esophagus and gastroesophageal junction was normal (Figures 1,2). A barium swallow showed a large intraluminal mass of the upper esophagus and compensatory dilatation of the proximal esophagus. A slightly irregular mucosal surface indicated a probable benign esophageal tumor (Figure 3). The patient underwent cervical, cardiac and abdominal ultrasound, which were unremarkable. Blood counts, biochemistry values and tumor markers levels were all found to be within normal limits.

After preoperative preparation, surgery of a thoracotomy was performed under general anesthesia. The patient was placed in the left lateral position. A small incision was made at the right posterolateral in the fourth intercostal space. Exploration revealed that the tumor had filled up the entire thoracic esophageal lumen. The pleura mediastinum was incised above the arch of the azygos vein to expose the upper segment of the esophagus. The longitudinal esophageal muscle and mucosa was dissected to expose the narrow pedicle (5 mm × 5 mm × 5 mm) of the tumor. Except the pedicle, which was a base of attachment to the esophageal submucosa, the rest of the tumor was isolated from the esophagus. Cut off the pedicle after ligating nutrient vessels in it and pulled up the tumor intactly. A nasogastric tube was indwelled (45 cm). The esophagus was closed longitudinally in three layers: a mucosal and submucosal layer of interrupted sutures of 3-0 silk, a muscular layer and an adventitial layer of interrupted sutures of 2-0 silk. A 28# chest tube was inserted in the seventh intercostal space along the anterior axillary line. The operation approximately took 60 min to complete and estimated intraoperative blood loss was 50 mL.
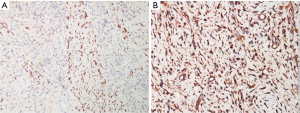
The tumor was soft in elasticity; it measured 12 cm × 3 cm × 2 cm, with an ellipsoidal shape (Figure 4). On microscopic examination of the tumor, there was no cellular atypia or areas of necrosis, and no mitotic activity. The overlying stratified squamous epithelium was seen stretched over the mass which composed of spindle cells organized in whorls. The immunohistochemical staining suggested that the tumor was positive for PGP 9.5 and Vimentin, partially positive for CD56 and Nestin, but negative for SMA, CD34, CD117, Desmin, S-100, NSE, EMA. The proliferation rate measured by detection of Ki-67 antigen expression was very low (approximately positive in 2% tumor cells) (Figure 5). Based on these features, the pathological diagnosis was neurofibroma.
The chest tube was removed on the 4th postoperative day. We performed a barium swallow of the upper digestive tract on the 7th postoperative day to examine the recovery of gastrointestinal function after surgery and it suggested satisfactory digestive system recovery (Figure 6). The postoperative course was uneventful, and the patient was discharged on the 10th postoperative day. The patient was seen at one-month follow-up and found to be doing well with no complaints. An endoscopy showed no evidence of anastomotic leakage and esophageal narrowing (Figure 7). Dysphagia, and retrosternal discomfort had completely relieved and he was able to have regular diet without nausea and vomiting. He was instructed to follow up in 1-year time.
Discussion
Benign esophageal tumors are rare, asymptomatic and usually found incidentally during investigations for other pathology or at the autopsy table. Tumors usually localized in an area of the esophageal wall and seldom involved the entire circumference of the esophagus (8). Large intramural masses tend to be symptomatic. The mean diameter of tumors in symptomatic patients was 5.3 cm (9). Dysphagia is most common clinical manifestation in patients with benign esophageal tumors. Other symptoms include vomiting, regurgitation, and retrosternal pain. Bleeding, compression of adjacent mediastinal structures causing airway obstruction and superior vena cava syndrome are included in unusual complications (2). No clear relationship has been demonstrated between tumor size and symptom duration.
Of the 504 esophageal tumors specimen, collected from the New York Medical College, Metropolitan Medical Center files of 19,982 consecutive autopsies over a period of 50 years, 90 (17.8%) were benign tumors. Of these benign esophageal tumors only 1 (1%) was a neurofibroma (8). There are 3 types of neurofibromas: localized, diffuse and plexiform. Most of esophageal neurofibromas are benign tumors and classified as granular cell tumors, which typically manifest as a 3 to 8 mm submucosal nodule found accidentally in the distal esophagus during gastroscopy (10). In our presented case, a neurofibroma occurred as a 12 cm submucosal tumor in the upper thoracic esophagus was rarely seen. As Reynolds reported, neurofibroma is the most typical characteristic of neurofibromatosis type 1 (VRD). Discrete benign neurofibromas within the dermis could be found in about 95% of patients. Nodular neurofibromas can arise at any site of peripheral nerves. Tumors affect long portions of nerves; infiltrate the nerve and surrounding tissues, which may cause disfiguration and mechanical complications. And these tumors are the primary reasons of morbidity and death. Nodular and plexiform neurofibromas could transform into malignant nerve tumors in about 2–16% of patients (11).
Because of the lesion has the potential for further enlargement to cause compress symptoms and even malignant transformation, it is recommended that esophageal neurofibromas should be surgically excised when found, especially associated with VRD (12). A previous report suggested esophagectomy was performed in a case of esophageal neurofibromatosis in VRD, and reconstruction was made through a gastric tube anastomosed to the cervical esophagus (13). In our case, we selected surgical treatment because the tumor had enlarged to the extent of leading to symptoms of dysphagia and regurgitation. Besides, persistent gastroesophageal reflux could be a risk factor of esophageal carcinoma.
Esophageal lesions greater than 10 cm in diameter are generally classified as giant tumor (14). Giant esophageal tumor was classically treated by open thoracotomy, either a right thoracotomy for tumors of the upper and middle third of the esophagus, or a left thoracotomy or transhiatal approach via laparotomy for lower third and esophagogastric junction (15). Although the minimally invasive surgery has developed rapidly, the indications of thoracoscopic approach still remain controversial, which depends on the size and location of the lesion and experience of the surgeon (16). In the case presented, the pedicle of the giant tumor was located in the upper thoracic esophagus. Besides, the patient had a long history of smoking and hypertension, his pulmonary and cardiac function was not optimistic. After comprehensive evaluation, a right posterolateral thoracotomy was considered as the most appropriate approach performed to remove the lesion. As the tumor enlarges, it tends to vascularity and displacement of adjacent structures. Consequently, a careful attention should be paid to hemostasis and protect adjacent viscera.
The lesions should be differentiated from other esophageal tumors by histopathologic diagnosis. The histopathologic characteristic appearance of neurofibroma was spindle-shaped cells associated with collagen fibrils.
Additionally, immunohistochemical staining helps to distinguish neurogenic from myogenic or other submucosal tumors. In our current report, the tumor comprised of fibrillary collagen and spindle cells organized in whorls, and it was positive for PGP 9.5 and Vimentin, but negative for SMA, CD34, CD117, Desmin, S-100, NSE, EMA.
Conclusions
In conclusion, giant neurofibroma of the esophagus is a rare condition and usually detected after significant enlargement with development of compressive symptoms. Surgical procedures can be performed in a manner similar to the present case used for neurofibroma and other benign tumors. Tumors are often diagnosed by immunohistochemical staining. We reported an additional case treated by complete surgical resection and primary repair of the esophagus. And further clinical evidence with larger samples is needed to prove its further efficacy.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
References
- Attah EB, Hajdu SI. Benign and malignant tumors of the esophagus at autopsy. J Thorac Cardiovasc Surg 1968;55:396-404. [PubMed]
- Choong CK, Meyers BF. Benign esophageal tumors: introduction, incidence, classification, and clinical features. Semin Thorac Cardiovasc Surg 2003;15:3-8. [Crossref] [PubMed]
- Hochberg FH, Dasilva AB, Galdabini J, et al. Gastrointestinal involvement in von Recklinghausen's neurofibromatosis. Neurology 1974;24:1144-51. [Crossref] [PubMed]
- Hyland PL, Freedman ND, Hu N, et al. Genetic variants in sex hormone metabolic pathway genes and risk of esophageal squamous cell carcinoma. Carcinogenesis 2013;34:1062-8. [Crossref] [PubMed]
- Macke RA, Nason KS. Minimally Invasive Resection of Benign Esophageal Lesions. Oper Tech Thorac Cardiovasc Surg 2014;19:396-413. [Crossref] [PubMed]
- Cheng BC, Chang S, Mao ZF, et al. Surgical treatment of giant esophageal leiomyoma. World J Gastroenterol 2005;11:4258-60. [Crossref] [PubMed]
- Hu X, Lee H. Complete thoracoscopic enucleation of giant leiomyoma of the esophagus: a case report and review of the literature. J Cardiothorac Surg 2014;9:34. [Crossref] [PubMed]
- Plachta A. Benign tumors of the esophagus. Review of literature and report of 99 cases. Am J Gastroenterol 1962;38:639-52. [PubMed]
- Mutrie CJ, Donahue DM, Wain JC, et al. Esophageal leiomyoma: a 40-year experience. Ann Thorac Surg 2005;79:1122-5. [Crossref] [PubMed]
- Goldblum JR, Rice TW, Zuccaro G, et al. Granular cell tumors of the esophagus: a clinical and pathologic study of 13 cases. Ann Thorac Surg 1996;62:860-5. [Crossref] [PubMed]
- Reynolds RM, Browning GG, Nawroz I, et al. Von Recklinghausen's neurofibromatosis: neurofibromatosis type 1. Lancet 2003;361:1552-4. [Crossref] [PubMed]
- Nishikawa K, Omura N, Yuda M, et al. Video-assisted thoracoscopic surgery for localized neurofibroma of the esophagus: case report and review of the literature. Int Surg 2013;98:461-5. [Crossref] [PubMed]
- Sica GS, Sujendran V, Warren B, et al. Neurofibromatosis of the esophagus. Ann Thorac Surg 2006;81:1138-40. [Crossref] [PubMed]
- Karagülle E, Akkaya D, Türk E, et al. Giant leiomyoma of the esophagus: a case report and review of the literature. Turk J Gastroenterol 2008;19:180-3. [PubMed]
- Ramos D, Priego P, Coll M, et al. Comparative study between open and minimally invasive approach in the surgical management of esophageal leiomyoma. Rev Esp Enferm Dig 2016;108:8-14. [PubMed]
- Chen X, Xi Y, Wang H, et al. Minimally invasive surgery for giant esophageal leiomyoma: a case report & review of the literatures. J Thorac Dis 2017;9:E26-E31. [Crossref] [PubMed]