Foreign body aspiration in adult airways: therapeutic approach
Introduction
Foreign body (FB) aspiration is an uncommon but potentially life-threatening event, accounting for 0.16–0.33% of adult bronchoscopic procedures (1). While the majority of accidental aspiration events occur in children, adults represent up to 25% of cases (2,3). Adult FB aspiration typically presents with a choking event followed by persistent coughing but, not uncommonly, can mimic more chronic diseases such as COPD, asthma, and obstructive pneumonia when the initial event goes unnoticed (e.g., elderly patient with altered mental status) (1,2,4-7). When the diagnosis is not established immediately, retained FBs may lead to recurrent pneumonias, bronchiectasis, recurrent hemoptysis, pneumothorax, lung abscesses, pneumomediastinum, or other complications (8). Extraction of aspirated FBs should be undertaken as soon as possible to alleviate acute symptoms and prevent long term complications.
The first successful FB extraction was performed by Gustav Killian in 1897. He extracted a bone from the right mainstem bronchus of a 63-year-old man using an esophagoscope heralding a new era in medical procedures (9). Following this, rigid bronchoscopy became the procedure of choice for removal of airway FBs, virtually eliminating the high mortality rate previously associated with this condition, and remained the most common indication for bronchoscopy until the advent of flexible bronchoscopy in the early 1970s. Flexible bronchoscopy broadened the scope of bronchoscopic interventions to the peripheral airway, allowing removal of foreign bodies lodged more distally with a large variety of dedicated flexible instruments (7). As technology advanced, technique spread, and practitioners became more experienced, flexible bronchoscopy gradually supplanted rigid bronchoscopy as the most commonly used technique in adults and has de facto become the modality of choice for a majority of patients (1,10-13). Albeit rigid bronchoscopy remains the traditional gold standard, particularly in children (2).
Symptoms and initial evaluation
Patient history is helpful in the evaluation of patients with suspected FB aspiration. The classically described “penetration syndrome,” consisting of a choking episode followed by intractable cough is more common in children than in adults. Patient recollection of FB aspiration was variable over multiple series in adults but surprisingly low, averaging about 50% (1,5,7,12-17). Patients over the age of 65 years old are less likely to remember the aspiration event, with only 30% supplying a history consistent with an aspiration event prior to bronchoscopy (7). This often hinders early diagnosis and can lead to a significant increase in potentially life-threatening complications. Multiple case series have documented cough as the most common symptom of FB aspiration, occurring in 58–96% of patients (4-6,15,16). Less common symptoms include wheezing, dyspnea, hemoptysis, chest pain, and recurrent pneumonia. These symptoms are determined by the size of the FB and the location in which it becomes lodged. Impaction in the trachea leads to a more dramatic presentation of inspiratory stridor with frequent coughing, while occlusion of the lower bronchi can result in coughing, wheezing, dyspnea, or hemoptysis, and may be mistaken for an alternative diagnosis (10). Respiratory symptoms are more common in those who have pre-existing pulmonary conditions. Between 2% and 10% of patients may be asymptomatic with a FB only incidentally identified on imaging (4-6). A good history may be able to identify the type of FB likely to be encountered in the airway. For example, nails, hair pins, and pen caps can be aspirated if they are placed into the mouth while working. Knowledge of the meal being eaten when a choking event occurs can identify likely FBs as well.
FB aspiration is slightly more common in males (1,6,12). The vast majority of adult patients with FB aspiration have obvious risk factors for aspiration including neurological deficits with swallowing difficulties or altered mental status, neuromuscular disease, intoxication, or have an iatrogenic cause. Still, 10% of adult patients with FB aspiration have no known risk factors (6,16-18). The average age of affected patients in most studies is between 50 and 60 years old, and FB aspiration risk appears to increase with age (4,7,17). Iatrogenic FB aspiration in adults is most commonly related to dental procedures requiring local anesthesia and supine positioning, or is associated with tracheostomy care (such as cleaning the tracheostomy with a curette). Traumatic airway management can lead to aspiration of teeth as well (6,18). The majority of FBs become lodged in the right bronchial tree, favoring the bronchus intermedius and the basal segments of the right lower lobe, owing to a more vertical course of the right mains stem bronchus. Interestingly, this anatomic asymmetry is not true in children in whom FBs may be found on both sides with equal likelihood. In adults, approximately 40% of FBs are found in the left bronchial tree and only 5–11% remain in the trachea (5-7,12-14).
Physical examination in a patient with suspected FB aspiration may be normal or may reveal nonspecific findings such as cough and hoarseness, especially if the FB is small. These symptoms may persist for a few days even if the FB was spontaneously expectorated. A patient with a FB lodged in the trachea or mainstem bronchi may present with stridor, persistent cough, significant dyspnea, loud wheezing localized to the side of the FB impaction, or absence of breath sounds on the affected side. Auscultation with the patient in the lateral decubitus positions may bring out wheezing on the dependent side. Hyperinflation on the side of the FB impaction, due to the ball-valve phenomenon, may lead to a larger appearing chest cage on that side. Conversely, complete airway obstruction by a FB with resultant atelectasis can present with absent breath sounds on the affected side.
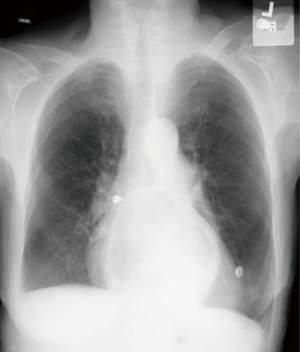
Standard postero-anterior and lateral chest radiographs should be obtained in all patients in whom FB aspiration is suspected. Radiographs directly identify the FB in 25% of patients, as only a minority of FBs such as coins, nails, teeth, or dental appliances are radiopaque (Figure 1). Most FBs are organic and radiolucent (such as food), and therefore not directly visible on chest radiograph (Figure 2). Nonetheless, chest radiographs demonstrate indirect, albeit non-specific, findings of atelectasis, hyperinflation, bronchiectasis, or lobar consolidation in the majority of patients (18-22). Expiratory films can assess for focal hyperinflation related to ball-valve phenomena caused by a FB that is partially obstructing an airway on inhalation and completely obstructing an airway on expiration (20). In 14–35% of patients the chest radiograph will be entirely normal (1,6,16,20-23).
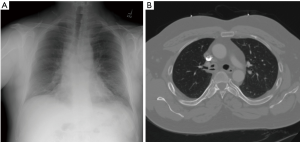
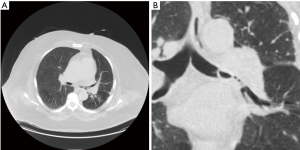
Chest computed tomography (CT) is more sensitive for identification of FBs, helps with procedural planning, and has become the gold standard of imaging studies when a FB aspiration is suspected (Figure 3). In addition, virtual bronchoscopy via CT has been shown to have sensitivity of 100% and specificity of 75% in patients who were being evaluated for suspected FB aspiration. This can also be helpful in procedural planning as it can help predict which tools may be needed prior to bronchoscopy (23-27). Additional findings on CT of the chest can include: atelectasis, focal hyperlucency, bronchiectasis, lobar consolidation, tree-in-bud infiltrates, ipsilateral pleural effusion, ipsilateral hilar adenopathy, and thickened bronchial walls (23).
Pre-procedural planning
The most important aspect of successful FB extraction is pre-procedural planning. This should involve the entire procedural team including the bronchoscopist, bronchoscopy assistants, nurses and anesthesiologist. Planning should involve discussion of the characteristics of the FB (organic, inorganic, metallic, plastic, smooth, friable, etc.), size, location in the airway, the anticipated step-wise approach to FB removal including back-up plans, as well as consideration of the patient’s co-morbid conditions. Working knowledge of the available bronchoscopy tools likely to be used is paramount in planning for FB removal. In addition, clearly defined contingency plans to maintain a patent airway and adequate ventilation throughout the case need to be carefully delineated, as interruption of a stable airway may be required during the procedure. Health care providers with expertise in airway management should be available to provide emergency airway management if needed (28,29).
Anesthesia and airway management
A variety of sedation approaches are possible including conscious sedation with spontaneous ventilation, general anesthesia with laryngeal mask airway or endotracheal intubation with positive pressure ventilation, or rigid bronchoscopy with jet ventilation (28,29). Each of these methods has advantages and disadvantages that need to be balanced in light of specific patient needs and anticipated FB characteristics. Use of conscious sedation and spontaneous respiration allows for the retrieval of objects through the mouth (the nose is too small to extract most foreign bodies) without the need for positive pressure or jet ventilation. This may obviate the need for general anesthesia and complete airway management but may require a level of cooperation from the patient only possible in selected cases. Patients may, for example, be asked to hold their breath during extraction to decrease airway movements for critical portions of the procedure. Endotracheal tubes provide a stable airway and allow for positive pressure ventilation which can be helpful in those patients in which hypoxemia may become an issue. However, the inner diameter is frequently too small for a FB to pass through, often necessitating removal en-bloc with the bronchoscope, retrieval device, and FB. In this situation, loss of airway control must occur temporarily to allow FB extraction. Laryngeal mask airways and rigid bronchoscopy also provide stable airways with larger inner lumens through which some FBs may be extracted without the need for extubation, thus eliminating the period of potential loss of airway. Rigid bronchoscopy also has the benefit of protecting the vocal cords from potential injury from a sharp FB. Larger objects still need to be removed en-bloc, resulting in temporary loss of airway control. Positive pressure and jet ventilation may need to be held though critical portions of FB extraction, including grasping of the FB and passage through the glottis (28). Spontaneous ventilation can sometimes lead to more collapsed airways thus making it more difficult to remove FBs, and positive pressure ventilation and jet ventilation can occasionally result in distal migration and more difficult FB removal (28,29). Constant communication between the bronchoscopist and the anesthesia team before and during the procedure is important to ensure safe and successful FB extraction.
A carefully defined back-up plan for re-establishing an airway emergently should always be discussed before FB removal, including delineating which provider will be responsible for replacing an airway device that must be removed to deliver a large FB. It is also possible for the FB to become lodged in the subglottic region or in the retropharynx upon attempted removal resulting in complete airway obstruction. Preparation should include a plan for establishing a surgical airway in such an event (30). Magill forceps under direct or video laryngoscopic visualization can occasionally salvage such situations and obviate the need for emergent tracheostomy or cricothyroidotomy, and should always be kept on hand.
Flexible versus rigid bronchoscopy
Flexible bronchoscopy has, in general, supplanted rigid bronchoscopy as the initial procedure for evaluation and management of FB aspiration. Flexible bronchoscopy allows for a more comprehensive airway survey and has an overall 90% success rate for retrieval (1,5,11-16,31). Flexible bronchoscopy is sometimes the only possible option, such as in the case of trauma patients with neck immobilization. It is noteworthy that rigid bronchoscopy is still considered the standard of care in pediatric patients by many bronchoscopists due to its intrinsic ability to provide ventilation and lesser chance of complete airway obstruction that may occur when a loose FB gets lodged in the sub-glottis, the narrowest portion of a child’s airway (10,31). Some FBs such as glass, nails, or thumbtacks may need to be shielded by an endotracheal tube or steel barrel of a rigid bronchoscope to avoid damaging the vocal cords during extraction (31). However, caution should be exercised when attempting to retrieve a FB through an endotracheal tube as it may result in FB impaction and precipitate acute respiratory distress. Significant bleeding, while a rare complication, is much easier to manage via rigid bronchoscopy, the barrel of which can be used to mechanically tamponade a bleed in accessible large airways and which allows for easy passage of adjunctive tools including large suction catheters and bronchial blockers (10). In general, rigid bronchoscopy is preferred in cases of acute respiratory distress (stridor, asphyxia), when retrieval via flexible bronchoscopy is expected to be particularly challenging, or when flexible bronchoscopy has failed. Rigid bronchoscopy should always be available as a backup for any case in which flexible bronchoscopy is chosen as the initial procedure. The advantages and disadvantages of flexible versus rigid bronchoscopy are summarized in Table 1.
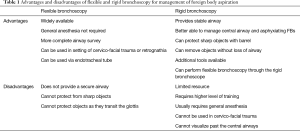
Full table
FB removal
In the absence of an asphyxiating FB, every case should start with a thorough airway survey. Care must be taken to asses both sides of the bronchial tree as 3–6% of patients may have bilateral FBs (31,32). In addition, coughing can result in expectoration of the FB or movement of the FB into an alternate airway than the one identified on CT scan. After the airway survey has been completed and the FB has been identified, the process of FB extraction can begin. In general, the bronchoscopist is responsible for maneuvering the bronchoscope into position and the first assistant is tasked with opening and closing the retrieval device. Care must always be taken to prevent pushing the FB more distally into the airway. More distal objects may need to be pulled back into the main airways where they can be grasped more easily by forceps or caught in baskets. This can be done by passing a Fogarty balloon catheter or flexible forceps beyond the object, inflating the balloon or opening the forceps, and then withdrawing the device to dislodge the FB more proximally. Once the FB is in the larger airways, a myriad of tools are available to the bronchoscopist for extraction. If the FB is not being extracted through a rigid bronchoscopy, care must be taken not to dislodge the FB from the extraction device as it passes through the glottis and the retropharynx by keeping it in view at all times as it is very carefully withdrawn (30). All attempts should be made to keep the FB from touching the walls of the trachea, vocal cords, or epiglottis during extraction as these are common reasons for displacement of the FB from the grasping instrument. Magill forceps should be available in the event that the FB is dislodged into the oropharynx.
Instruments
Forceps
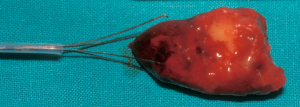
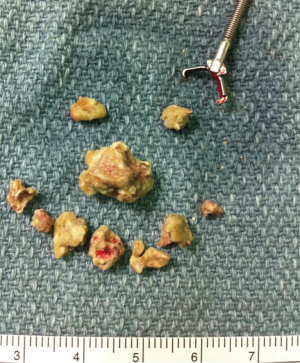
Forceps are the most utilized tools for FB extraction (1,5,12). They come in multiple configurations of teeth and bite diameters to accommodate objects of varying size and texture, and are best used for extraction of objects with thin edges. Shark tooth, rat tooth, and alligator tips allow for the grasping of coins, plastic objects, and other non-friable organic FBs such as bones (Figure 4). Rubberized tips are best utilized for grasping more delicate objects or relatively smooth objects, and they can also be used to grasp sharp objects, thus protecting the airway mucosa from trauma caused by an exposed edge or point. Standard cupped forceps used for endobronchial biopsy are not as useful as the previously listed forceps. Forceps should generally not be used for removal of particularly friable objects such as food matter as this is likely to result in disruption of the FB into multiple fragments that may migrate into distal airways (31,33).
When using forceps, fluoroscopy can be a useful adjunct to help identify more distal airway foreign bodies that are radiopaque such as pins and nails (34-36). There is one report of the use of navigational bronchoscopy to extract a distal airway pin (37). While these techniques can be useful in guiding retrieval, extreme caution should be taken to ensure that the object is not advanced into a distal airway beyond where it can be directly visualized by the bronchoscope.
Magnetic
Magnetic probes can be used for the retrieval of ferromagnetic objects in the airway. These probes can be advanced toward the FB until the magnet comes into contact with the FB and then slowly withdrawn towards the central airways. Magnetic probes do not provide a strong grasp on objects and loss of the FB in the upper airway on attempted retrieval is common. For this reason, they are typically used to move more distal FBs into the mainstem airways where a forceps or baskets are more effective (33,38-40).
Snares
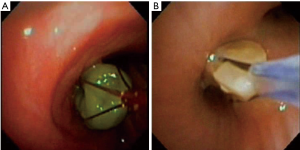
Multi-prong snares are available for the extraction of larger objects (5,33). These consist of multiple thin wires with grasping tips that are pushed out into the airway and come together upon withdrawal of the instrument. The FB is then trapped in arms of the snare and withdrawn (Figure 5). Snares do not have the grasping power of typical forceps but the barbed tips allow for grasping of larger soft objects. Snares work best when the object has been pulled into the mainstem bronchi to allow room for the snare to maneuver and expand around the FB.
Baskets
Baskets are the second most commonly used retrieval instrument in flexible bronchoscopy (1,5,12). They come in many shapes and sizes and provide a method for the removal of friable objects from the airway without breaking off pieces of the FB (Figure 6). In addition, these are helpful in the removal of round objects or objects that are too large for forceps to grasp. Baskets are typically composed of 3–8 wires attached to a lead point. The catheter is initially passed beyond the FB. Following this, the basket is deployed to allow it to open distal to the object. The basket is then withdrawn slowly. Minor twisting or flexing manipulations may be necessary for the FB to fall into the basket. Once the object is in the basket, it is pulled taught and the object, basket, and flexible bronchoscope are removed together. The number of wires in the basket should be determined by the size of the object. Fewer wires allows for larger objects to be caught in the basket, however, it will also make it easier for smaller FBs to fall out.
Fish net baskets can be used for larger objects or those that are difficult to trap in the wire basket (33). The net can be extended out of the working channel after which the bronchoscope is used to manipulate the net over the object. Once the object is within the net, the wire net is drawn back, trapping the object. The entire assembly including the bronchoscope can then be removed.
Balloon catheter
A Fogarty arterial embolectomy balloon catheter is especially useful for objects that have been aspirated into the deeper airways. The catheter and balloon can be advanced beyond the object at which point the balloon is inflated and pulled back to displace the FB towards the mainstem airways. From the mainstem airways or the trachea, the FB can be grasped with forceps or caught in a basket. In addition, objects with central lumens, such as beads, may allow passage of the Fogarty catheter through the object allowing it to be removed without additional instrumentation (41-45). Fogarty catheters can also be advanced alongside the bronchoscope, which allows for the working channel of the bronchoscope to remain open for other tools such as baskets and forceps. Care must be taken with use of the Fogarty catheter, as aggressive attempts at withdrawal have resulted in failure of the device as well as pneumothoraces (46).
Cryoprobe
The use of the flexible cryoprobe for removal of foreign bodies has been shown to be very effective, especially for organic objects and those with significant surrounding granulation tissue (33,47-50). Cryoprobes can be used with both flexible and rigid bronchoscopy (Figure 7). In this technique, the cryoprobe is advanced towards the FB through the working channel. After coming into contact, the probe is activated to rapidly freeze the object and cause it to adhere to the cryoprobe tip. Once cryoadhesion has occurred, the object can be gently removed from the airway. Care must be taken not to touch the probe to the bronchial walls during this procedure as this can result in removal of bronchial tissue, bleeding and rarely airway perforation. The ability of FBs to cryoadhere is primarily based on the water content of the object with objects of higher water content being more likely to adhere. Fruchter and Kramer evaluated the use of a flexible cryoprobe extraction in vitro with commonly aspirated objects (51). They demonstrated that 5 seconds of cold time lead to cryoadhesion of bones, vegetable matter, pills, and a few thin metal objects (paperclips, hair pins, stapler pins). Hard organic objects with lower water contents such as nuts were not adherent. Other objects that were not adherent included chewing gum, teeth, dental caps, nails, screws, metal coins, glass, and pen caps. Ten seconds of cold time did not improve cryoadherence nor did saline rinsing prior to applying cryo. Prior to bronchoscopy, testing of a known FB for cryoadherence can determine if this will be a particularly useful technique. One must keep in mind that organic objects will often cause a significant local tissue reaction with granulation tissue and mucus production, which may allow for cryo-adhesion even if in vitro testing does not support this (51).
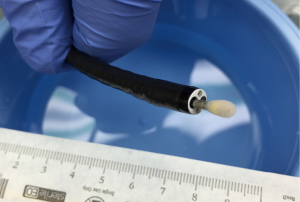
In addition to direct retrieval of foreign bodies, the cryoprobe can be used for the destruction of surrounding granulation tissue which can free embedded objects (52).
Patient positioning
Patient positioning can be manipulated to improve the success of the procedure. Trendelenburg positioning can be useful in allowing FBs that are in the main airways to fall towards the upper airways rather than towards the lower airways thus allowing increased working space (53,54). This is especially useful when working with round objects such as beads and certain nuts which will tend to roll back down to the distal bronchi in supine positioning. Using a rigid bronchoscope, it is possible to use the Trendelenburg position to manipulate the FB into the barrel of the bronchoscope where it can be extracted without the use of forceps (54). In patients where the FB is soft and has been moved to the central airways but cannot be extracted, upright positioning and vigorous coughing may dislodge the object as well (33).
Post-retrieval care
After the FB has been retrieved, it is imperative that the bronchoscopist perform a repeat airway survey. A full airway survey should be completed to assess for additional FBs, which are identified in 3–6% of patients (31,32). Review of the area in which the FB was lodged should be done to assess for retained fragments of the original FB, bronchial stenosis, granulation tissue, or bleeding. If there are mucopurulent or purulent secretions, as are often found in chronic FB impaction with complications such as bronchiectasis and lung abscess, they should be collected for culture. Bleeding has been shown to occur in 1–5% of bronchoscopies for FB extraction and is often related to significant granulation tissue that can be highly vascular (1,6,12,14). This is often self-abating but sometimes requires management with topical epinephrine, electrocautery, Nd:YAG or Nd:YAP lasers, or by argon plasma coagulation (5,16,31,55).
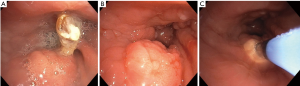
Granulation tissue occurs as a localized reaction to FB aspiration in up to 76% of patients and is noted with increasing frequency with longer duration between aspiration event and FB retrieval (Figure 8) (5,52). Some organic FBs and certain pill aspirations may result in exuberant granulation tissue within a few hours of aspiration. Peanuts, for example, have a high oil content that leads to an exuberant reaction (31,56). Occasionally objects can become embedded in the bronchial wall by granulation tissue. A short course of glucocorticoids, such as prednisone or methylprednisolone 0.5–1 mg/kg × 24 hours, has been reported to reduce granulation tissue and improve extraction in several case studies but evidence driving timing and dose of steroids is lacking (1,57). Granulation tissue can also be removed with electrocautery, laser, argon plasma coagulation, or cryoprobe prior to attempted removal to free the object from the bronchial wall (5,52). Care must be taken not to damage the bronchial wall with these maneuvers. After removal of a FB, residual granulation tissue can lead to persistent airway obstruction. In prior studies, residual granulation tissue often improves with steroids and time. However, if there is significant bronchial stenosis or obstruction caused by granulation tissue, removal at the time of initial bronchoscopy is warranted (1,5). Follow up imaging and/or bronchoscopy is should be performed to ensure resolution of granulation tissue.
Significant bronchial stenosis can occur around, proximal, or distal to the FB related to inflammatory reaction and granulation tissue. Proximal airway stenosis can hinder the extraction of FBs and can be treated with balloon dilation prior to attempted extraction (58). Care must be taken to avoid compression of the FB by the dilation balloon during this procedure. Again, re-evaluation of the airway post-procedure should be complete and true airway stenosis should be treated with balloon dilation and/or destructive techniques as listed above to achieve airway patency (1,5).
Challenges and complications
Sharp FBs such as nails, pins, and needles should be extracted by grasping the sharp point if possible. This protects the sharp end of the object while it is being retracted through the airway (Figure 9) (33). Attempts to grab the shaft of these objects leaves the free sharp end unprotected and injury to the bronchial and tracheal walls may occur. These objects also need to be pulled through the vocal cords and this is often only possible in their narrowest dimension to allow passage and reduce the risk of vocal cord and oropharyngeal injury. Rigid bronchoscopy should be considered in these instances, as this allows the bronchoscopist to guard the sharp aspect of the FB with the barrel of the rigid bronchoscope.

Few objects are so excessively large that they are unable to be grasped with forceps or caught in a basket. These objects are quite difficult to remove and may require more coordinated care. Sehgal et al. reported the removal of a 4.5-cm long fruit from the left mainstem bronchus using a cryoprobe (59). This object would not have fit into any basket and was friable and likely to be fragmented by forceps. Nd:YAG lasers have been used to break apart solid organic objects, such as bones, to facilitate extraction (5,60).
Attempted removal of a large object that leads to tracheal obstruction could lead to rapid inability to ventilate and an emergency situation. This is especially concerning in the subglottic area where FBs may become dislodged from forceps or baskets and remain high in the trachea. If this occurs, the FB should be pushed distally into one mainstem bronchus with the bronchoscope where it will not cause bilateral obstruction (30,31). Once this is completed and ventilation is re-established, repeat attempts at extraction can be undertaken. Strong consideration should be given to the use of rigid bronchoscopy for improved airway protection during subsequent attempts at extraction.
Loss of objects in the oropharynx can lead to repeat aspiration and tracheal obstruction/asphyxiation or can lead to the FB entering the esophagus. For loss above the glottis, Magill forceps should be available for prompt removal under direct or video laryngoscopy. If the FB is causing asphyxiation and cannot be immediately extracted, providers should be prepared to perform emergent tracheostomy or cricothyroidotomy (28,29). In the case of a FB entering the esophagus, transit through the GI tract is safe in most cases (as the majority of FBs are organic) with the exception of large or sharp objects. If this occurs, consultation with a gastroenterologist or general surgeon for further management is recommended.
In the event that a FB cannot be removed by flexible or rigid bronchoscopy, the procedure should be terminated and consultation with thoracic surgeon should be performed. This should represent the vast minority of cases (1,5,11-18). Thoracic surgery should also be available at the time of the procedure in the event of a significant complication, such as bronchial wall lacerations or airway compromise.
Conclusions
FB aspiration, while uncommon in adults, still accounts for about 1 in 400 bronchoscopic procedures. This makes it difficult for an individual provider to develop experience with the available tools and techniques required for successful FB extraction. An experienced team including a bronchoscopist, bronchoscopy assistants, nurse, and anesthesiologist are required for successful extraction of airway FB. The vast majority of FBs can be extracted safely with flexible bronchoscopy and the use of forceps and baskets. However, the use of more advanced tools often not available in the community setting and the occasional need to utilize rigid bronchoscopy suggests that FB extraction should be performed in a facility that has advanced tools and trained personnel available whenever possible.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Sehgal IS, Dhooria S, Ram B, et al. Foreign Body Inhalation in the Adult Population: Experience of 25,998 Bronchoscopies and Systematic Review of the Literature. Respir Care 2015;60:1438-48. [Crossref] [PubMed]
- Baharloo F, Veyckemans F, Francis C, et al. Tracheobronchial foreign bodies: presentation and management in children and adults. Chest 1999;115:1357-62. [PubMed]
- Hsu Wc, Sheen Ts, Lin Cd, et al. Clinical experiences of removing foreign bodies in the airway and esophagus with a rigid endoscope: a series of 3217 cases from 1970 to 1996. Otolaryngol Head Neck Surg 2000;122:450-4. [PubMed]
- Boyd M, Watkins F, Singh S, et al. Prevalence of flexible bronchoscopic removal of foreign bodies in the advanced elderly. Age Ageing 2009;38:396-400. [Crossref] [PubMed]
- Dong YC, Zhou GW, Bai C, et al. Removal of tracheobronchial foreign bodies in adults using a flexible bronchoscope: experience with 200 cases in China. Intern Med 2012;51:2515-9. [Crossref] [PubMed]
- Limper AH, Prakash UB. Tracheobronchial foreign bodies in adults. Ann Intern Med 1990;112:604-9. [Crossref] [PubMed]
- Lin L, Lv L, Wang Y, et al. The clinical features of foreign body aspiration into the lower airway in geriatric patients. Clin Interv Aging 2014;9:1613-8. [PubMed]
- al-Majed SA, Ashour M, al-Mobeireek AF, et al. Overlooked inhaled foreign bodies: late sequelae and the likelihood of recovery. Respir Med 1997;91:293-6. [Crossref] [PubMed]
- Killian G. Meeting of the Society of Physicians of Freiburg, Freiburg. 1897, Dec 17. Munchen Med Wschr 1898;45:378.
- Dikensoy O, Usalan C, Filiz A. Foreign body aspiration: clinical utility of flexible bronchoscopy. Postgrad Med J 2002;78:399-403. [Crossref] [PubMed]
- Rodrigues AJ, Oliveira EQ, Scordamaglio PR, et al. Flexible bronchoscopy as the first-choice method of removing foreign bodies from the airways of adults. J Bras Pneumol 2012;38:315-20. [Crossref] [PubMed]
- Swanson KL, Prakash UB, McDougall JC, et al. Airway foreign bodies in adults. J Bronchol 2003;10:107-11. [Crossref]
- Debeljak A, Sorli J, Music E, et al. Bronchoscopic removal of foreign bodies in adults: experience with 62 patients from 1974-1998. Eur Respir J 1999;14:792-5. [Crossref] [PubMed]
- Blanco Ramos M, Botana-Rial M, García-Fontán E, et al. Update in the extraction of airway foreign bodies in adults. J Thorac Dis 2016;8:3452-6. [Crossref] [PubMed]
- Chen CH, Lai CL, Tsai TT, et al. Foreign body aspiration into the lower airway in Chinese adults. Chest 1997;112:129-33. [Crossref] [PubMed]
- Mise K, Jurcev Savicevic A, Pavlov N, et al. Removal of tracheobronchial foreign bodies in adults using flexible bronchoscopy: experience 1995-2006. Surg Endosc 2009;23:1360-4. [Crossref] [PubMed]
- Boyd M, Chatterjee A, Chiles C, et al. Tracheobronchial foreign body aspiration in adults. South Med J 2009;102:171-4. [Crossref] [PubMed]
- Ramos MB, Fernández-Villar A, Rivo JE, et al. Extraction of airway foreign bodies in adults: experience from 1987-2008. Interact Cardiovasc Thorac Surg 2009;9:402-5. [Crossref] [PubMed]
- Goyal R, Nayar S, Gogia P, et al. Extraction of tracheobronchial foreign bodies in children and adults with rigid and flexible bronchoscopy. J Bronchology Interv Pulmonol 2012;19:35-43. [Crossref] [PubMed]
- Kavanagh PV, Mason AC, Müller NL. Thoracic foreign bodies in adults. Clin Radiol 1999;54:353-60. [Crossref] [PubMed]
- Pinto A, Scaglione M, Pinto F, et al. Tracheobronchial aspiration of foreign bodies: current indications for emergency plain chest radiography. Radiol Med 2006;111:497-506. [Crossref] [PubMed]
- Sersar SI, Rizk WH, Bilal M, et al. Inhaled foreign bodies: presentation, management and value of history and plain chest radiography in delayed presentation. Otolaryngol Head Neck Surg 2006;134:92-9. [Crossref] [PubMed]
- Zissin R, Shapiro-Feinberg M, Rozenman J, et al. CT findings of the chest in adults with aspirated foreign bodies. Eur Radiol 2001;11:606-11. [Crossref] [PubMed]
- Adaletli I, Kurugoglu S, Ulus S, et al. Utilization of low-dose multidetector CT and virtual bronchoscopy in children with suspected foreign body aspiration. Pediatr Radiol 2007;37:33-40. [Crossref] [PubMed]
- Haliloglu M, Ciftci AO, Oto A, et al. CT virtual bronchoscopy in the evaluation of children with suspected foreign body aspiration. Eur J Radiol 2003;48:188-92. [Crossref] [PubMed]
- Huang HJ, Fang HY, Chen HC, et al. Three-dimensional computed tomography for detection of tracheobronchial foreign body aspiration in children. Pediatr Surg Int 2008;24:157-60. [Crossref] [PubMed]
- Tong B, Zhang L, Fang R, et al. 3D images based on MDCT in evaluation of patients with suspected foreign body aspiration. Eur Arch Otorhinolaryngol 2013;270:1001-7. [Crossref] [PubMed]
- Fidkowski CW, Zheng H, Firth PG. The anesthetic considerations of tracheobronchial foreign bodies in children: a literature review of 12,979 cases. Anesth Analg 2010;111:1016-25. [PubMed]
- Kendigelen P. The anaesthetic consideration of tracheobronchial foreign body aspiration in children. J Thorac Dis 2016;8:3803-7. [Crossref] [PubMed]
- Pawar DK. Dislodgement of bronchial foreign body during retrieval in children. Paediatr Anaesth 2000;10:333-5. [Crossref] [PubMed]
- Swanson KL. Airway foreign bodies: what's new? Semin Respir Crit Care Med 2004;25:405-11. [Crossref] [PubMed]
- Rodríguez H, Passali GC, Gregori D, et al. Management of foreign bodies in the airway and oesophagus. Int J Pediatr Otorhinolaryngol 2012;76 Suppl 1:S84-91. [Crossref] [PubMed]
- Mehta AC, Rafanan AL. Extraction of Airway Foreign Body in Adults. J Bronchol 2001;8:123-31. [Crossref]
- Gill SS, Pease RA, Ashwin CJ, et al. Respiratory-aspirated 35-mm hairpin successfully retrieved with a Teflon® snare system under fluoroscopic guidance via a split endotracheal tube: a useful technique in cases of failed extraction by bronchoscopy and avoiding the need for a thoracotomy. Br J Radiol 2012;85:e756-9. [Crossref] [PubMed]
- Yüksel M, Ozyurtkan MO, Laçin T, et al. The role of fluoroscopy in the removal of tracheobronchial pin aspiration. Int J Clin Pract 2006;60:1451-3. [Crossref] [PubMed]
- Hamamoto Y, Fukusumi M, Takeoka S, et al. Successful removal of a distally located foreign body using a guide sheath. J Bronchology Interv Pulmonol 2013;20:352-4. [Crossref] [PubMed]
- Karpman C, Midthun DE, Mullon JJ. A distal airway foreign body removed with electromagnetic navigation bronchoscopy. J Bronchology Interv Pulmonol 2014;21:170-2. [Crossref] [PubMed]
- Mayr J, Dittrich S, Triebl K. A new method for removal of metallic-ferromagnetic foreign bodies from the tracheobronchial tree. Pediatr Surg Int 1997;12:461-2. [Crossref] [PubMed]
- Saito H, Saka H, Sakai S, et al. Removal of broken fragment of biopsy forceps with magnetic extractor. Chest 1989;95:700-1. [Crossref] [PubMed]
- Hsu AA. Endoscopic intervention of lower airway foreign matter in adults-a different perspective. J Thorac Dis 2015;7:1870-7. [PubMed]
- Bawa M, Kalawant A, Vinod MS, et al. Unsuccessful Retrieval of Impacted Foreign Body Bronchus: Think about Fogarty Catheter. Indian J Pediatr 2016;83:744-5. [Crossref] [PubMed]
- Elsharkawy H, Abd-Elsayed AA, Karroum R. Management challenges in the passing-through technique using a fogarty catheter to remove an endobronchial foreign body from an infant. Ochsner J 2015;15:110-3. [PubMed]
- Landy C, Massoure PL, Gauthier J, et al. Use of a Fogarty catheter after tracheobronchial inhalation of a bead. Trop Doct 2012;42:219-20. [Crossref] [PubMed]
- Mackle T, Russell J. The combined use of a Fogarty balloon with extraction forceps for the controlled retrieval of an endobronchial foreign body. Int J Pediatr Otorhinolaryngol 2001;60:163-5. [Crossref] [PubMed]
- Wankhede RG, Maitra G, Pal S, et al. Successful Removal of Foreign Body Bronchus Using C-arm-guided Insertion of Fogarty Catheter through Plastic Bead. Indian J Crit Care Med 2017;21:96-8. [Crossref] [PubMed]
- Treen DC Jr, Falterman KW, Arensman RM. Complications of the Fogarty catheter technique for removal of endobronchial foreign bodies. J Pediatr Surg 1989;24:613-5. [Crossref] [PubMed]
- Schumann C, Kropf C, Rüdiger S, et al. Removal of an aspirated foreign body with a flexible cryoprobe. Respir Care 2010;55:1097-9. [PubMed]
- Sehgal IS, Dhooria S, Behera D, et al. Use of cryoprobe for removal of a large tracheobronchial foreign body during flexible bronchoscopy. Lung India 2016;33:543-5. [Crossref] [PubMed]
- Sriratanaviriyakul N, Lam F, Morrissey BM, et al. Safety and Clinical Utility of Flexible Bronchoscopic Cryoextraction in Patients With Non-neoplasm Tracheobronchial Obstruction: A Retrospective Chart Review. J Bronchology Interv Pulmonol 2015;22:288-93. [Crossref] [PubMed]
- Zhang L, Yin Y, Zhang J, et al. Removal of foreign bodies in children's airways using flexible bronchoscopic CO2 cryotherapy. Pediatr Pulmonol 2016;51:943-9. [Crossref] [PubMed]
- Fruchter O, Kramer MR. Retrieval of various aspirated foreign bodies by flexible cryoprobe: in vitro feasibility study. Clin Respir J 2015;9:176-9. [Crossref] [PubMed]
- Fang YF, Hsieh MH, Chung FT, et al. Flexible bronchoscopy with multiple modalities for foreign body removal in adults. PLoS One 2015;10:e0118993. [Crossref] [PubMed]
- Huang PM, Kao MW. Endobronchial foreign body removed by flexible bronchoscopy using the Trendelenburg position. Thorac Cardiovasc Surg 2012;60:545-7. [PubMed]
- Sersar SI. The Egyptian technique revisited (Sersar-Mansoura technique). How to remove some inhaled foreign bodies through rigid bronchoscopy without using a forceps. Rev Port Pneumol 2011;17:222-4. [Crossref] [PubMed]
- Sachdeva A, Pickering EM, Lee HJ. From electrocautery, balloon dilatation, neodymium-doped:yttrium-aluminum-garnet (Nd:YAG) laser to argon plasma coagulation and cryotherapy. J Thorac Dis 2015;7:S363-79. [PubMed]
- Mehta AC, Khemasuuwan D. A foreign body of a different kind: Pill aspiration. Ann Thorac Med 2014;9:1-2. [Crossref] [PubMed]
- Lando T, Cahill AM, Elden L. Distal airway foreign bodies: Importance of a stepwise approach, knowledge of equipment and utilization of other services' expertise. Int J Pediatr Otorhinolaryngol 2011;75:968-72. [Crossref] [PubMed]
- Thornton CS, Yunker WK. Rigid bronchoscopy and balloon dilation for removal of aspirated thumbtacks: case series and literature review. Int J Pediatr Otorhinolaryngol 2015;79:1541-3. [Crossref] [PubMed]
- Sehgal IS, Dhooria S, Behera D, et al. Use of cryoprobe for removal of a large tracheobronchial foreign body during flexible bronchoscopy. Lung India 2016;33:543-5. [Crossref] [PubMed]
- Boelcskei PL, Wagner M, Lessnau KK. Laser-assisted removal of a foreign body in the bronchial system of an infant. Lasers Surg Med 1995;17:375-7. [Crossref] [PubMed]