The Redax® Coaxial Drain in pulmonary lobectomy: a study of efficacy
Introduction
Drainage of the pleural cavity after thoracic surgery is usually accomplished by using one or two large bore chest tubes (CTs). Due to the large diameter and limited flexibility of these tubes, patients often complain of intercostal pain at the insertion site, increasing the need of pain control drugs. An inadequate pain control might cause alterations in the pattern of breathing: the patient generates low tidal volumes, increasing the risk of atelectasis. The problem is compounded by cough suppression, which, in the presence of increased secretions, will further worsen atelectasis.
In the past decade, some papers reported the use of flexible silastic chest drains in patients undergoing thoracotomy for different pleural or pulmonary pathologies. These publications reported about the safety and efficacy of these drains (1-7).
Recently, a new flexible, fluted, coaxial silastic drain has been released by Redax® (Mirandola, Italy) (Figure 1).

In this paper, we have studied the characteristics of safety and efficacy of the aforementioned CT in patients undergoing pulmonary lobectomy.
Methods
The study has been approved by the Institutional Ethics Committee of the University of Eastern Piedmont. Due to its retrospective nature, an informed consent from each patient was deemed unnecessary.
Surgical patient population
Since February 2010, intra-operative and post-operative management of patients undergoing pulmonary lobectomy and lymph nodes dissection for clinical stage I or II primary lung cancer in our Institution has been standardized as follows.
Open pulmonary lobectomy is performed through a lateral muscle-sparing thoracotomy at 5th intercostal space, whereas video-assisted thoracic surgery (VATS) lobectomy is performed through an anterior three-portal approach (8). Open or VATS approach was carried out on the basis of the surgeon’s choice. After removal of the specimen, the air leak from the bronchial stump and residual lung parenchyma is checked by soaking the re-inflated residual lobe/s in warm saline solution under a 30 cmH2O internal airway pressure; if air leaks are found, the damaged area is secured with appropriate sutures or application of sealant materials. At the end of the operation, a 24-F CT is inserted in 7th intercostal space at the anterior axillary line in open surgery or through the anterior-inferior port (the camera port) in VATS lobectomies; in all cases the tip of the tube is positioned at the apex of the chest cavity, regardless of the type of lobectomy performed. CTs are connected to water-seal immediately after surgery.
Post-operative pain management is provided by infusion of levobupivacaine/sufentanyl through an epidural thoracic catheter in open lung surgery and by subarachnoid analgesia (morphine injection) plus oral paracetamol in VATS. Visual analog scale (VAS) score is used to quantify post-operative pain at rest and while coughing is induced by the respiratory therapist.
Fluid drainage (blood or serum), and the presence of air leaks from the CT at rest and while coughing is recorded every 12 h and registered; the occurrence of clinically evident subcutaneous emphysema is registered too. At post-operative day 1 (POD1), a routine chest X-ray is carried out and evidence of not completely expanded residual lobe(s) due to pneumothorax or fluid accumulation is recorded; in case of tension pneumothorax or increasing subcutaneous emphysema the tube is connected to an active suction system with a continuous negative pressure of 20 cmH2O, until resolution; in cases where the use of suction proves ineffective, a second CT is inserted at the appropriate site on the basis of the radiological indication.
Tubes are usually removed when there is no residual air-leak and the amount of drained fluid is <250 mL/day. Another chest X-ray is carried out the day following CT removal and residual pleural cavity or fluid accumulation is recorded.
Study population
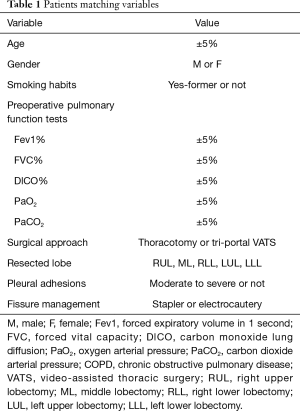
During the period between 1st August 2016 and 25th January 2017, 52 patients undergoing pulmonary lobectomy and lymph nodes dissection for primary lung cancer (32 open surgery and 20 VATS) received a single 24-F Redax® Coaxial Drain (CD) (Redax, Mirandola, Italy) in order to drain the pleural cavity after resection (group A). Each of these patients has been matched, on the basis of some variables, with 2 patients who were operated for primary lung cancer during the previous 4 years in the same department and who had been treated with a single 24-F large bore standard CT (group B); matching variables are listed in Table 1 (the matching process was conducted by two surgeons—Ottavio Rena, Sara Parini—blinded of the post-operative events). Characteristics of matched groups are listed in Table 2.
Full table

Full table
We retrospectively collected and analyzed data from the in-hospital medical records of the two groups of patients: duration of surgery, post-operative morbidity and mortality, amount of chest-drained fluid (rate of drained fluid during POD0/total drained fluid), and postoperative air-leak presence and duration, POD1 chest X-ray demonstration of pneumothorax or pleural fluid accumulation, occurrence of post-operative tension pneumothorax or increasing subcutaneous emphysema, chest-drain duration, occlusion of chest drain by fibrin or blood clots at removal, VAS score on POD1 and 2, chest X-ray detection of pleural residual cavity or fluid accumulation after tube removal.
Statistical analysis
Data have been processed with a statistical computing software [Statistica (version 9), StatSoft Inc., Tulsa, OK, USA]. Results are reported as percentage, mean ± standard deviation (SD) for normally distributed variables. Chi-square and Student’s t-test were used to compare percentages and mean values; a P-value of 0.05 or less has been considered significant.
Results
Post-operative data are reported in Table 3. No difference was recorded between the two groups in terms of occurrence of post-operative complications and mortality rates (specifically considering atelectasis and sputum retention).

Full table
Mean fluid evacuation was higher for group A patients, though not significant, whereas the rate of drained fluid at POD0/total drained fluid was significantly higher for group A patients. The highest amount of fluid drainage without occlusion for group A patients was 1,650 mL in 12 h.
Chest drain air-leak rate was 36% in group A and 34% in group B and the mean duration of the post-operative air-leak was similar in the two groups. No cases of tension pneumothorax were registered, whereas the rate of occurrence of post-operative subcutaneous emphysema was 1.9% and 3.8% in group A and B respectively (no differences recorded). In cases with increasing subcutaneous emphysema we applied 20 cmH2O external suction according to our standard protocol, and we observed that the complication has been solved after a median of 7 days; only in one case of group B a second CT was inserted due to the malfunction of the first one.
At POD1 chest X-ray, pneumothorax rate is slightly lower in group A, and the same group has a significantly lower pleural fluid retention rate.
We registered no cases of tube occlusion by clots in group A, whereas in group B, 6/104 patients showed occlusion of the CT at the removal.
Mean POD-1 and 2 VAS score is slightly lower in group A both at rest and while coughing, but if we consider only patients who have undergone VATS (sub-group A: 20 patients and sub-group B: 40 patients), group A patients complained a significantly lower post-operative pain.
Mean chest drain duration was slightly lower for group A patients (5.2 vs. 5.5 days).
Chest X-ray after tube removal showed a similar rate of residual pleural cavity in the two groups, but a significantly lower rate of pleural fluid accumulation in group A.
Discussion
After lung resections, drainage of the pleural cavity is necessary in order to remove blood, other fluids and air, thus preventing lung collapse due to pleural effusion, haemothorax or pneumothorax, and to monitor postoperative bleeding and air leak.
Over the past decades, surgeons routinely used stiff CTs made of polyvinyl chloride that might be associated with complications and have several undesirable features.
Because of the size, stiffness and in case of more than one tubes, the standard CTs can hinder post-operative recovery by limiting early ambulation and deep breathing.
In some cases, thrombus formation within the drain might hamper further drainage and promote residual collection of fluid within the pleural space, which can lead to acute or chronic consequences.
In the last decades, some authors proved that a single CT may be sufficient to evacuate fluid and air-leak from pleural cavity after a pulmonary lobectomy (9-10); other authors demonstrated that a single chest drain under water-seal is more useful than suction to seal post-operative air-leak (11-12). Following the above-mentioned studies, since 2010, our institution adopted a standardized protocol for intra-operative and post-operative management of post-lobectomy air-leak and chest drain: all our patients received a single 24-F CT under water-seal.
During the last years, some authors reported about the use of silastic drains that are round or flat, flexible and grooved, that may apply constant suction over the entire fluted portion of the tube (1-7). All the above papers concluded that, after lung surgery, the use of fluted drains is safe and useful in both fluid and air evacuation.
Recently, a new silastic drain has been developed (Redax® CD). The new drain has a grooved round profile associated with an internal coaxial lumen; it is made of pure biocompatible silicone and is composed by: (I) a fluted tube section that allows effective drainage by effect of the capillary action and prevents tube occlusion following traction and/or torsion; (II) a round lumen, coaxial to the grooved section which allows separate air evacuation from the thoracic cavity draining it directly from the distal end through specifically created holes.
As for the others fluted drains used in the past, the surface area provided by the Redax® CD is considerably more extended than the actual area of evacuation through the side holes of a standard CT. These non-collapsible long channels for drainage should be resistant to occlusion with thrombus.
We conducted a comparison study about the safety and efficacy of a 24-F Redax® CD versus a 24-F standard CT.
The first variable we studied is the capability of the new drain to evacuate post-operative fluid collections from the pleural cavity. In the group of patients receiving Redax® CD we recorded a higher (though not significant) total amount of drained fluid after surgery; a significant lower rate of residual fluid in the pleural cavity on POD1 chest X-ray and a lower rate of residual pleural effusion viewed on chest x-ray after tube removal. In particular, when the rate of fluid drainage during the POD0/total drainage was considered, Redax® CD warranted an evacuation rate significantly higher than that of the standard CT. When compared with a standard CT, the design of fluted surface allowed a faster fluid evacuation from the pleural cavity.
A second variable analyzed to evaluate the efficacy of the new drain is the occlusion rate at removal; Redax® CD was never found to be occluded by thrombus or fibrin clots at removal whereas 5.8% of cases occurred in the group of the standard chest drain; its material and tube design are demonstrated efficient to prevent tube occlusion even when a large amount of fluid had to be expelled.
In terms of capability of air-leak evacuation, the Redax® CD was similar to the 24-F standard chest drain: no event of tension pneumothorax occurred and the frequency of subcutaneous emphysema is similar in the two groups. The rate of POD1 pneumothorax (incomplete re-expansion of the residual lobe/s after lobectomy) is similar to that observed for standard CTs such as the frequency of residual pleural cavity at discharge. This is probably caused by other factors such as a fixed pleural space deficit that may exist secondary to the lack of compliance of the residual lung parenchyma, the patient’s chest wall mechanic and other complex factors, many of which have absolutely nothing to do with the flow characteristics of the chest drain.
The flexible and soft material of the new drain seemed to be responsible of a lower mean VAS score reported during the entire chest drain permanence when compared to standard. Although it is difficult to distinguish the pain due to thoracotomy from pain related to the tube, the difference is easily appreciated after VATS surgery, when the drain is inserted in one of the VATS access port, instead of through an additional incision. It should be concluded that Redax® CD proves more comfortable for patients than the standard CTs.
The present study has some limitations particularly due to its retrospective nature and absence of randomization, but the comparison of two matched groups may be useful to reach the following conclusions: in terms of evacuation of fluid, Redax® CD is superior to the standard large bore CTs while it is not inferior to the standard tubes in terms of air-leak evacuation; the tube design and used material is useful to prevent occlusion of the tube by thrombus or fibrin clots; the flexibility and softness of its material allows a good tolerability.
Conclusions
The Redax® CD has been demonstrated safe and effective in draining the pleural cavity after pulmonary lobectomy. Further randomized studies are needed to confirm the above conclusions.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethics statement: The study was approved by our Institutional Ethics Committee of the University of Eastern Piedmont, Novara, Italy (No. 19746). Due to its retrospective nature, an informed consent from each patient was deemed unnecessary.
References
- Kejriwal NK, Newman MA. Use of a single silastic chest drain following thoracotomy: initial evaluation. ANZ J Surg 2005;75:710-2. [Crossref] [PubMed]
- Terzi A, Feil B, Bonadiman C, et al. The use of flexible spiral drains after non-cardiac thoracic surgery. A clinical study. Eur J Cardiothorac Surg 2005;27:134-7. [Crossref] [PubMed]
- Stolz AJ, Lischke R, Simonek J, et al. Comparison study on the use of tubular and spiral thoracic drains following lung resections. A prospective study. Rozhl Chir 2005;84:529-32. [PubMed]
- Ishikura H, Kimura S. The use of flexible silastic drains after chest surgery: novel thoracic drainage. Ann Thorac Surg 2006;81:331-3. [Crossref] [PubMed]
- Icard P, Chautard J, Zhang X, et al. A single 24F Blake drain after wedge resection or lobectomy: a study on 100 consecutive cases. Eur J Cardiothorac Surg 2006;30:649-51. [Crossref] [PubMed]
- Nakamura H, Taniguchi Y, Miwa K, et al. The use of Blake drains following general thoracic surgery: is it an acceptable option? Interact Cardiovasc Thorac Surg 2009;8:58-61. [Crossref] [PubMed]
- Sakakura N, Fukui T, Mori S, et al. Fluid drainage and air evacuation characteristics of Blake and conventional drains used after pulmonary resection. Ann Thorac Surg 2009;87:1539-45. [Crossref] [PubMed]
- Hansen HJ, Petersen RH. Video-assisted thoracoscopic lobectomy using a standardized three-port anterior approach - The Copenhagen experience. Ann Cardiothorac Surg 2012;1:70-6. [PubMed]
- Gómez-Caro A, Roca MJ, Torres J, et al. Successful use of a single chest drain postlobectomy instead of two classical drains: a randomized study. Eur J Cardiothorac Surg 2006;29:562-6. [Crossref] [PubMed]
- Okur E, Baysungur V, Tezel C, et al. Comparison of the single or double chest tube applications after pulmonary lobectomies. Eur J Cardiothorac Surg 2009;35:32-5; discussion 35-6. [Crossref] [PubMed]
- Cerfolio RJ, Bass C, Katholi CR. Prospective randomized trial compares suction versus water seal for air leaks. Ann Thorac Surg 2001;71:1613-7. [Crossref] [PubMed]
- Marshall MB, Deeb ME, Bleier JI, et al. Suction vs water seal after pulmonary resection: a randomized prospective study. Chest 2002;121:831-5. [Crossref] [PubMed]


