Endoscopic diverticulotomy with a stapler can be an effective and safe treatment for Killian-Jamieson diverticulum
Introduction
Since its first report by Ekberg and Nylander in 1983 (1), Killian-Jamieson diverticulum (KJD), a rare and unfamiliar entity of esophageal disease, is recognized via pharyngoesophagography. KJD arises through a muscle gap between the cricopharyngeus muscle superiorly, the longitudinal muscle of the esophagus laterally, and the circular muscle of the esophagus inferiorly. The gap known as the Killian-Jamieson area is distinctively different from the Killian’s triangle, an anatomically weak zone just above the cricopharyngeus muscle on the posterior aspect of the upper esophagus that is responsible for the development of Zenker’s diverticulum (ZD). ZD is the most common type of esophageal diverticulum with four times the incidence of KJD (2), and it is also associated with a larger size and more clinically apparent symptoms than KJD.
Open surgical approach is the key means of managing pharyngoesophageal diverticulum due to possible nerve injury. Both KJD and ZD are in close proximity to the recurrent laryngeal nerve (RLN), which ascends in the tracheoesophageal groove, traveling in a caudocranial direction. Recently, a minimally invasive endoscopic technique for treatment of ZD has gained in popularity due to the ease of use and shorter recovery time. Endoscopic management of pharyngoesophageal diverticulum was first described by Mosher in 1917 and reintroduced by Dohlman and Mattsson in 1960 (3). In addition to open surgery, outcomes of endoscopic surgery for KJD remain sketchy because of its rare incidence and inherent risk of nerve injury. Herein, we present a case of an elderly man who was diagnosed as having symptomatic KJD, and underwent endoscopic diverticulotomy successfully with favorable outcomes.
Case presentation
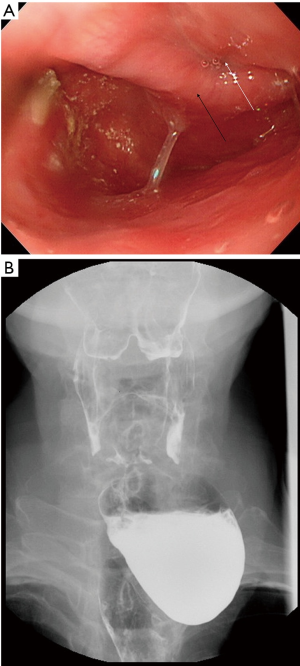
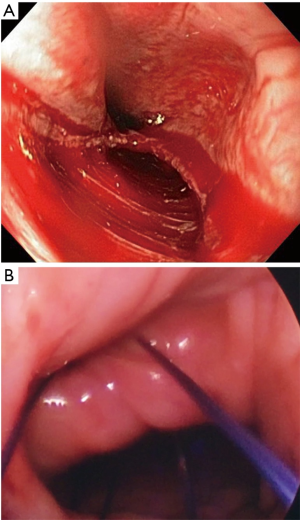
An 88-year-old man presented to our chest surgery outpatient department with complaints of solid dysphagia, globus sensation, and food regurgitation for a 6-month period. He denied having odynophagia, halitosis, and gastroesophageal reflux symptoms. He had a history of myocardial infarction and a post coronary artery stent implantation 6 years ago. As symptoms deteriorated, he underwent upper endoscopic assessment. Upper endoscopy revealed a wide-mouthed esophageal sac below the upper esophageal sphincter with food retention (Figure 1A). An antero-posterior projection of a barium swallow pharyngoesophagogram demonstrated a large left-sided diverticulum, 5.4 cm in diameter, in the region of the pharyngoesophageal junction with contrast pooling, indicating KJD (Figure 1B). Endoscopic intervention was offered because the patient refused a transcervical approach. In addition, he was concerned that due to his cardiovascular condition, he could not remain under general anesthesia for a long time and deal with the subsequent postoperative recovery. After he provided informed written consent for endoscopic diverticulotomy, the procedure was performed under general anesthesia with the patient in supine position. During the surgery, the septum between the esophagus and the diverticulum was clearly identified via a rigid laryngoscope, and the septum was retracted toward to the operator slightly using silk suture to obtain good visualization and a better operation field (Figure 2A). A linear endo-stapler (Endo-GIA 45-4.8® Covidien, Minneapolis, MN, USA) was then gently introduced at the midline of the septum and down into the diverticulum sac, and the cutting depth was about 2 cm without touching the bottom. After opening up the common wall of the diverticulum sac and esophagus, we confirmed that there’s no leakage or massive bleeding (Figure 2B). The total operation time from endotracheal tube intubation to extubation was 58 min. The patient was started on a clear liquid diet postoperative day 1 and discharged home on the postoperative day 3 without procedure-related complications. A barium swallow esophagogram obtained 1 month after surgery showed a small remaining diverticulum, 3 cm in size (Figure 3), and the patient reported complete resolution of the previous symptoms. Additionally, his voice was unaffected and intact recurrent laryngeal function was revealed by stroboscopy.

Discussion
KJD is a rare condition of the upper esophageal diverticulum, with scarce reporting since Ekberg and Nylander in 1983 (1). The pathogenesis of KJD is remains unclear, and acquired dyscoordination of pharyngeal and esophageal muscle may be responsible for its development, given its distribution among the elderly (4,5). KJD is often misdiagnosed as ZD upon endoscopy examination, and the gold standard for differentiating these two types of diverticulum is barium swallow pharyngoesophagogram. Although ZD and KJD are due to hypopharynx or esophagus anatomical weakness, their location is distinctly different. According to Rubesin and Levine (2), a total of 16 patents with KJD and 26 patients with ZD were reviewed and analyzed. Radiographically, ZD was located just above the cricopharyngeal bar, with the sac protruding posteriorly to the esophagus, whereas KJD located below the cricopharyngeus muscle, with the sac outpouching laterally to the cervical esophagus. The disorder of cricopharyngeal sphincter function is thought to be associated with ZD. In addition, according to the different anatomical relationship with the cricopharyngeus muscle of the two types of diverticulum, ZD was found to be more symptomatic than KJD, especially dysphagia and troubling aspiration pneumonia.
Surgical resection of hypopharyngeal diverticulum is the key for treatment in the past century, and development of minimally invasive intervention for ZD with endoscopic technique has gained in popularity since 1960 when Dohlman and Mattsson introduced the new transoral method (3). Endoscopic diverticulotomy using a stapler, CO2-laser, or energy device is more advantageous compared with an open approach, including shorter operation time, absence of neck incision, quicker recovery to diet toleration, and shorter hospital stay. A recent review article by Leong et al. (6) demonstrated a total number of 540 patients with ZD underwent endoscopic stapling, and more than 90% of patients reported resolved or significantly improved symptoms, with an overall complication rate of 9.6%. A major observed complication was iatrogenic perforation (26 of 52, 50%), and no postoperative nerve injury was observed. Unlike ZD, endoscopic treatment has still not been widely accepted in KJD, since it is rare and relatively unfamiliar to clinicians. In addition, a smaller diverticulum limits the operation field, thus making it difficult to access the small pouch. Most importantly, high risk of possible nerve injury while performing blind cutting should be taken into account.
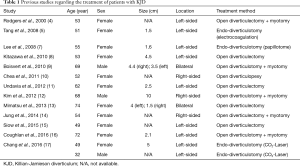
The present study was a case report of an 88-year-old patient with symptomatic KJD treated with endoscopic diverticulotomy and compared with previous 14 patients with KJD in literature (Table 1). This is the fifth case of endoscopic diverticulotomy for a KJD patient and also the first case using a stapler division. To avoid RLN injury, a detailed preoperative plan and cautious intraoperative manipulation was essential. Our first and foremost strategy was to use silk suture at both ends of the septum between the esophagus and diverticulum, making a counter-traction force that created more space to allow application of a stapler cartridge while lifting the septum away from RLN. According to Undavia et al., the RLN traveling in the proximal tracheoesophageal groove can be either anterior or posterior to the base of KJD (11), and midline division would lower the possibility of RLN injury. The same concept was also presented by Lee et al. and Chang et al. (7,17), who performed a mid-point cutting using a CO2-laser and isolated-tip needle-knife papillotome, respectively. Furthermore, the direction of division should be in a vertical manner due to the longitudinal course of the RLN and its proximity to the KJD (5). Finally, a diverticulotomy is considered and performed to create a communication between the esophagus and the diverticulum, making an adequate auto-drainage of food material and saliva from the diverticular sac to the esophageal lumen. Therefore, a slight division is good enough to create a communication and avoid deeper the division as well as possible nerve injury.
Full table
Although minimally invasive treatment with endoscopic stapling is a safe and effective method for the treatment of ZD, illustrating good outcomes and low complication rates (6), the operation should be performed in KJD with extreme care and precaution since its inherent possibility of nerve injury as aforementioned. Our case offers a choice of quicker and less invasive means to address KJD under properly selected circumstances. However, the real efficacy and further understanding of complications of endoscopic stapling for the treatment of KJD should be determined via larger patient cohorts and longer follow-up periods for such patients.
Conclusions
Endoscopic stapling can be a safe and effective choice of treatment for selected patients with symptomatic KJD in need of a surgical intervention.
Acknowledgements
The authors thank the thoracic surgery team at the Tri-Service General Hospital, Taiwan, for their perioperative support and participation.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this case report and the accompanying images.
References
- Ekberg O, Nylander G. Lateral diverticula from the pharyngo-esophageal junction area. Radiology 1983;146:117-22. [Crossref] [PubMed]
- Rubesin SE, Levine MS. Killian-Jamieson diverticula: radiographic findings in 16 patients. AJR Am J Roentgenol 2001;177:85-9. [Crossref] [PubMed]
- Dohlman G, Mattsson O. The endoscopic operation for hypopharyngeal diverticula: a roentgencinematographic study. AMA Arch Otolaryngol 1960;71:744-52. [Crossref] [PubMed]
- Rodgers PJ, Armstrong WB, Dana E. Killian-Jamieson diverticulum: a case report and a review of the literature. Ann Otol Rhinol Laryngol 2000;109:1087-91. [Crossref] [PubMed]
- Tang SJ, Tang L, Chen E, et al. Flexible endoscopic Killian-Jamieson diverticulotomy and literature review (with video). Gastrointest Endosc 2008;68:790-3. [Crossref] [PubMed]
- Leong SC, Wilkie MD, Webb CJ. Endoscopic stapling of Zenker's diverticulum: establishing national baselines for auditing clinical outcomes in the United Kingdom. Eur Arch Otorhinolaryngol 2012;269:1877-84. [Crossref] [PubMed]
- Lee CK, Chung IK, Park JY, et al. Endoscopic diverticulotomy with an isolated-tip needle-knife papillotome (Iso-Tome) and a fitted overtube for the treatment of a Killian-Jamieson diverticulum. World J Gastroenterol 2008;14:6589-92. [Crossref] [PubMed]
- Kitazawa M, Koide N, Saito H, et al. Killian-Jamieson diverticulitis with cervical cellulitis: report of a case. Surg Today 2010;40:257-61. [Crossref] [PubMed]
- Boisvert RD, Bethune DC, Acton D, et al. Bilateral Killian-Jamieson diverticula: a case report and literature review. Can J Gastroenterol 2010;24:173-4. [Crossref] [PubMed]
- Chea CH, Siow SL, Khor TH, et al. Killian-jamieson diverticulum: the rarer cervical esophageal diverticulum. Med J Malaysia 2011;66:73-4. [PubMed]
- Undavia S, Anand SM, Jacobson AS. Killian-Jamieson diverticulum: a case for open transcervical excision. Laryngoscope 2013;123:414-7. [Crossref] [PubMed]
- Kim DC, Hwang JJ, Lee WS, et al. Surgical treatment of killian-jamieson diverticulum. Korean J Thorac Cardiovasc Surg 2012;45:272-4. [Crossref] [PubMed]
- Mimatsu K, Oida T, Kano H, et al. Killian-jamieson diverticula presenting synchronously with thyroid adenoma. Case Rep Gastroenterol 2013;7:188-94. [Crossref] [PubMed]
- Jung WS, Cho JH. Incidentally found Killian-Jamieson diverticulum due to an embedded fish bone. J Craniofac Surg 2014;25:515-6. [PubMed]
- Siow SL, Mahendran HA, Hardin M. Transcervical diverticulectomy for Killian-Jamieson diverticulum. Asian J Surg 2017;40:324-328. [Crossref] [PubMed]
- Coughlan CA, Verma SP. The Utility of Recurrent Laryngeal Nerve Monitoring During Open Pharyngeal Diverticula Procedures. Ann Otol Rhinol Laryngol 2016;125:648-51. [Crossref] [PubMed]
- Chang YC, Chi CY, Lee CJ. Rigid endoscopic LASER diverticulotomy for lateral pharyngoesophageal diverticuli: cases presentation and discussion. Eur Arch Otorhinolaryngol 2016;273:4637-4642. [Crossref] [PubMed]


