Should sinus of Valsalva be preserved in patients with bicuspid aortic valve and aortic dilation?
Introduction
Bicuspid aortic valve (BAV) is the most common type of congenital valvular heart disease, affecting 0.9% to 2.0% of the general population (1). BAV disease is a well-recognized risk factor for aortic dilation, aneurysm formation, dissection, and rupture (2,3). Aggressive intervention for BAV aortopathy is recommended by the current guidelines, but few studies have listed exact criteria regarding interventions targeting the sinuses of Valsalva in patients with BAV who have undergone selective aortic valve surgery. Although the risk of progressive dilatation of the ascending segment after replacement of the aortic valve and ascending aorta is well documented, the risk of progressive dilatation of the sinuses of Valsalva is less clear. The purpose of this study was to assess the risk of progressive sinus of Valsalva dilatation and dissection after replacement of the aortic valve and ascending aorta and to determine the threshold diameter at which the aortic root should be replaced in BAV patients.
Methods
This study was approved by the Ethic Committee of Zhongshan Hospital of Fudan University (approval number: B2016-193). All patients signed an informed consent before participating.
We identified 156 patients (age 56.2±10.8 years old, 46 females) who underwent aortic valve replacement (AVR) and supracoronary ascending aorta replacement in our institution from 2010–2014 via a search of our computerized clinical database. Patients with connective tissue disorders (Marfan syndrome, Loeys-Dietz syndrome, and Ehlers-Danlos syndrome) and a history of root replacement (Bentall, Cabrol, David, or Yacoub procedure) were excluded from the study. Perioperative data were collected from the database and via retrospective reviews of patient medical records, including transthoracic echocardiographic reports, pathology reports, and all operative records. Aortic root and ascending aortic size were determined from preoperative and the most recent echocardiograms. There is no uniform policy regarding the size at which the sinuses must be replaced at out institution; therefore, it is likely that some mildly or even moderately enlarged sinuses were left intact. Long-term follow-up information was obtained via outpatient follow-up visits and telephone surveys. The date of last known clinical contact was used for patients who were “alive”.
Descriptive statistics were presented as the mean ± standard deviation (SD) for continuous variables and as frequencies and percentages for categorical variables. Comparisons of categorical variables were performed with Chi-square or Fisher exact tests, and continuous variables were analyzed with paired t-tests. All statistical tests were 2-sided, and an alpha level of 0.05 was considered statistically significant. Analysis was performed using SPSS version 21.0 (IBM Inc., Armonk, NY, USA).
Results
The preoperative demographics of the cohort are displayed in Table 1. Of these patients, 124 (79%) patients had BAV disease. The remaining 32 (21%) patients had tricuspid aortic valve (TAV) disease. Depending on the origins of the coronary arteries, BAVs were divided into the following two groups: BAV-AP group (82/124), which comprised BAVs exhibiting fusion of right and left coronary cusps, and BAV-RL group (42/124), which comprised BAVs exhibiting fusion of the right or left coronary cusp and the noncoronary cusp. In the entire study population, 58 (37.2%) patients had aortic stenosis, 34 (21.8%) patients had aortic regurgitation, and 64 (41.0%) patients had a mixed lesion. The aortic valve was replaced with a stented tissue valve in 28 (17.9%) patients and a mechanical valve in 128 (82.1%) patients. The mean labeled valve size was 23.7±1.6 mm. All patients received a straight Dacron graft with a mean size of 29.3±2.1 mm.
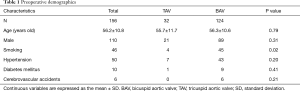
Full table
The in-hospital mortality rate in the entire study population was 1.3% (two patients). The intraoperative and postoperative outcomes for both study groups are list in Table 2. The in-hospital mortality rate was comparable between the study groups (0.8% in the BAV group vs. 3.3% in the TAV group, P=0.29). The cause of death in both patients was a fatal arrhythmia. The reoperation rates for bleeding, respiratory dysfunction, stroke, and renal dysfunction were not significantly different between the BAV and TAV groups.
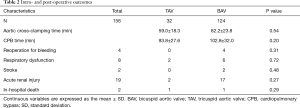
Full table
The aortic root characteristics of both study groups are listed in Table 3. The mean preoperative aortic root diameters of the TAV and BAV groups were 42.2±5.4 and 37.5±5.4 mm, respectively (P=0.69). The mean preoperative ascending aorta diameters of the TAV and BAV groups were 51.2±5.2 and 49.2±6.2 mm, respectively (P=0.79). After operation, most of the patients had decreased aortic root sizes, as the TAV and BAV groups exhibited mean postoperative root diameters of 39.6±5.2 and 35.7±5.1 mm, respectively (P=0.99). A total of 16 patients had a preoperative root diameter greater than 45 mm (mean root diameter of 48.8±3.2 mm). The postoperative root diameter of those patients was 44.4±5.2 mm, for a reduction of 4.1±3.6 mm. Regarding the effects of BAV type on preserved aortic sinus growth, there was no significant difference between the BAV-AP and BAV-RL groups (P=0.20).
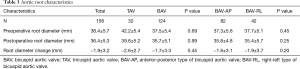
Full table
The mean follow-up time was 34.4±22.3 months (0.1–75.2 months), and 97% of patients completed the follow-up. During a follow-up period of up to 75.2 months, there were no late reoperations for aortic root dissection or rupture. Even among the 16 patients who had a preoperative root diameter greater than 45 mm, no adverse events were observed. One patient died of a cerebrovascular accident during the follow-up period.
Discussion
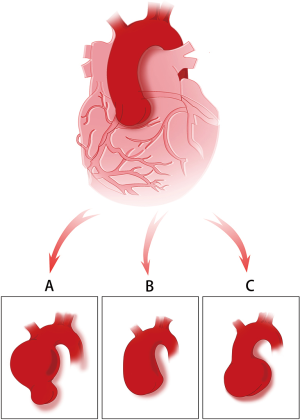
Although it is well recognized that BAV is frequently complicated by aortopathy (2,3) and that aggressive interventions are recommended for dilated ascending aorta by both the European and American guidelines (4,5), treatment of the sinuses of Valsalva in patients with BAV is controversial. The 2010 American guidelines for thoracic aortic disease recommended concomitant aortic replacement at a diameter of 45 mm (class I, evidence level C) (4). However, the same condition was changed to class IIa in the 2014 American VHD guidelines (6). In the 2016 statement regarding aortic dilatation in patients with BAV, the condition was still categorized as class IIa (7). None of these guidelines provided exact criteria regarding intervention for the sinuses of Valsalva in patients with BAV who have undergone selective aortic valve surgery. Definitive data regarding the risk of progressive sinus of Valsalva dilatation and dissection after AVR in patients with BAV are lacking. As we all know, the patterns of bicuspid aortopathy are not identical and there are mainly three types (Figure 1). The patients enrolled in this study presented with dilated ascending aorta and relatively normal or mild dilated sinuses (Figure 1A). The results of our study indicated that in this patient population, the risk of progressive sinus of Valsalva dilatation and dissection after aortic valve and ascending aorta replacement is very low. During a follow-up period of up to 75.2 months, there were no late complications related to root rupture or dissection, and no evidence of progressive sinus enlargement was noted by echocardiographic studies. In addition, the results of the comparisons between preoperative and postoperative root diameters showed mild reductions in both study groups (1.7±3.3 for BAV vs. 2.6±2.7 for TAV, P=0.45). Even among patients with mild dilated root (≥45 mm), a reduction of 4.1±3.6 mm in sinus of Valsalva diameter was also observed and no adverse events occurred during the follow-up. Therefore, separate valve and graft replacements remain appropriate procedures for the BAV patients with dilated ascending aorta and relatively normal or slight dilated aortic root.
The findings of this study are consistent with those of several earlier studies from other institutions (8,9). Park and colleagues (10) reported a 5% incidence of late reoperations, but they did not report any late reoperations for aortic root dissection or rupture. The most common reasons for reoperation in their study were prosthetic valve endocarditis or prosthesis-patient mismatch. The only patient who required reoperation for late dilatation of the aortic root underwent AVR and aortoplasty during the primary operation. We attribute this finding to the fact that the aortopathy associated with BAV is phenotypically heterogeneous, as some aneurysms appear to be entirely supracoronary, and others involve the root, as one may see in Marfan syndrome. The results of our study, as well as those of the aforementioned previous studies by Sundt et al. and Park et al. (9,10), suggest that in clinical practice, those sinuses that are not thought to be sufficiently enlarged to justify formal root replacement by an operating surgeon at the time of AVR and supracoronary aortic replacement seldom lead to reoperation or late death.
Our findings may differ from those of other studies, whose authors have recommended full root replacement in patients with BAV with aortic valve dysfunction combined with ascending aortic dilatation greater than 4 to 4.5 cm (11). Russo and colleagues (12) reported a 6% aortic reoperation rate after AVR in patients with BAV over a 20-year period. Borger and colleagues (13) reported an 11% incidence of ascending aortic complications during 10 years of follow-up after AVR for BAV. However, on closer inspection, there were no cases of aortic root pathology in either of these studies. Furthermore, in an older study regarding patients with aneurysms with diverse causes, in which the long-term results of separate valve and graft replacements were compared with those of composite replacements, the Stanford group reported that 49 of 255 patients undergoing separate valve and ascending aortic repair underwent late reoperation. Thirty-five of those reoperations were performed on the valve itself, and 7 of those operations were performed for aneurysmal dilatation of the sinuses of Valsalva. Of the 7 patients who underwent reoperation for aneurysmal dilatation, 5 had acute or chronic dissections, and 4 had Marfan syndrome (14). The data supporting routine composite root replacements in BAV aortopathy are scarce.
Composite root replacement is a well-established procedure that can be accomplished with very low operative risk under elective circumstances (15). Compared with separate AVR and supracoronary aortic replacement, however, composite root replacement is technically more challenging and carries risks of coronary ostial complications, including bleeding, kinking, and false aneurysm formation. The overall operative mortality rate after composite root replacement ranges from 1.5% to 11.7% (15,16). However, separate AVR and supracoronary aortic replacements are safer procedures. Peterss and colleagues (17) reported no increase in operative risk after the addition of a root-sparing ascending aorta replacement compared with isolated AVR. Studies from the University of Virginia, University of Toronto, Northwestern University, and University of Udine focusing on bicuspid valves demonstrated similarly favorable results and confirmed the safety of the root-sparing approach (18-21). In our cohort, the overall in-hospital mortality rate after separate AVR and ascending aortic replacement was 1.3%, which is a very acceptable result.
This was a retrospective study exhibiting the inherent limitations of such an analysis. In addition, although the maximum follow-up duration was 74.2 months, the mean follow-up duration was considerably shorter at 34.4±22.3 months, which placed significant constraints on our ability to predict with certainty the likelihood of root dilatation over a prolonged period of time. Nevertheless, this was a relatively large series whose results, which demonstrated that mild reductions in aortic root diameter occurred after separate aortic valve and graft replacements, were promising.
Conclusions
In summary, to avoid the risks associated with aortic root replacement, it is reasonable to spare the aortic root in the setting of separate valve and graft replacement for BAV with a dilated ascending aorta and relatively normal sinuses of Valsalva.
Acknowledgements
Funding: This work was supported by the Shanghai Municipal Commission of Health and Family Planning (No. W2014-009 to C Wang) and the Fudan University Zhongshan Hospital Youth Research Fund (No. 2016ZSQN24 to Y Lin).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This study was approved by the Ethic Committee of Zhongshan Hospital of Fudan University (approval number: B2016-193) and written informed consent was obtained from all patients.
References
- Biner S, Rafique AM, Ray I, et al. Aortopathy is prevalent in relatives of bicuspid aortic valve patients. J Am Coll Cardiol 2009;53:2288-95. [Crossref] [PubMed]
- Larson EW, Edwards WD. Risk factors for aortic dissection: a necropsy study of 161 cases. Am J Cardiol 1984;53:849-55. [Crossref] [PubMed]
- Roberts CS, Roberts WC. Dissection of the aorta associated with congenital malformation of the aortic valve. J Am Coll Cardiol 1991;17:712-6. [Crossref] [PubMed]
- Hiratzka LF, Bakris GL, Beckman JA, et al. 2010 ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM guidelines for the diagnosis and management of patients with Thoracic Aortic Disease: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, American Association for Thoracic Surgery, American College of Radiology, American Stroke Association, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology, Society of Thoracic Surgeons, and Society for Vascular Medicine. Circulation 2010;121:e266-369. [Crossref] [PubMed]
- Erbel R, Aboyans V, Boileau C, et al. 2014 ESC Guidelines on the diagnosis and treatment of aortic diseases: Document covering acute and chronic aortic diseases of the thoracic and abdominal aorta of the adult. The Task Force for the Diagnosis and Treatment of Aortic Diseases of the European Society of Cardiology (ESC). Eur Heart J 2014;35:2873-926. [Crossref] [PubMed]
- Nishimura RA, Otto CM, Bonow RO, et al. 2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 2014;129:e651. [Crossref]
- Hiratzka LF, Creager MA, Isselbacher EM, et al. Surgery for Aortic Dilatation in Patients With Bicuspid Aortic Valves: A Statement of Clarification From the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol 2016;67:724-31. [Crossref] [PubMed]
- Adams RD, Goldin MD, Najafi H. Selectivity in aortic root reconstruction. J Card Surg 1994;9:500-7. [Crossref] [PubMed]
- Sundt TM 3rd, Mora BN, Moon MR, et al. Options for repair of a bicuspid aortic valve and ascending aortic aneurysm. Ann Thorac Surg 2000;69:1333-7. [Crossref] [PubMed]
- Park CB, Greason KL, Suri RM, et al. Fate of nonreplaced sinuses of Valsalva in bicuspid aortic valve disease. J Thorac Cardiovasc Surg 2011;142:278-84. [Crossref] [PubMed]
- Etz CD, Homann TM, Silovitz D, et al. Long-term survival after the Bentall procedure in 206 patients with bicuspid aortic valve. Ann Thorac Surg 2007;84:1186-93. [Crossref] [PubMed]
- Russo CF, Mazzetti S, Garatti A, et al. Aortic complications after bicuspid aortic valve replacement: long-term results. Ann Thorac Surg 2002;74:S1773-6; discussion S1792-9.
- Borger MA, Preston M, Ivanov J, et al. Should the ascending aorta be replaced more frequently in patients with bicuspid aortic valve disease? J Thorac Cardiovasc Surg 2004;128:677-83. [Crossref] [PubMed]
- Yun KL, Miller DC, Fann JI, et al. Composite valve graft versus separate aortic valve and ascending aortic replacement: is there still a role for the separate procedure? Circulation 1997;96:II-368-75. [PubMed]
- Gott VL, Greene PS, Alejo DE, et al. Replacement of the aortic root in patients with Marfan's syndrome. N Engl J Med 1999;340:1307-13. [Crossref] [PubMed]
- Caceres M, Ma Y, Rankin JS, et al. Mortality characteristics of aortic root surgery in North America. Eur J Cardiothorac Surg 2014;46:887-93. [Crossref] [PubMed]
- Peterss S, Charilaou P, Dumfarth J, et al. Aortic valve disease with ascending aortic aneurysm: Impact of concomitant root-sparing (supracoronary) aortic replacement in nonsyndromic patients. J Thorac Cardiovasc Surg 2016;152:791-8.e1. [Crossref] [PubMed]
- Vendramin I, Meneguzzi M, Sponga S, et al. Bicuspid aortic valve disease and ascending aortic aneurysm: should an aortic root replacement be mandatory? Eur J Cardiothorac Surg 2016;49:103-9. [Crossref] [PubMed]
- Reece TB, Singh RR, Stiles BM, et al. Replacement of the proximal aorta adds no further risk to aortic valve procedures. Ann Thorac Surg 2007;84:473-8. [Crossref] [PubMed]
- Sioris T, David TE, Ivanov J, et al. Clinical outcomes after separate and composite replacement of the aortic valve and ascending aorta. J Thorac Cardiovasc Surg 2004;128:260-5. [Crossref] [PubMed]
- Rinewalt D, McCarthy PM, Malaisrie SC, et al. Effect of aortic aneurysm replacement on outcomes after bicuspid aortic valve surgery: validation of contemporary guidelines. J Thorac Cardiovasc Surg 2014;148:2060-9. [Crossref] [PubMed]


