Lung metastases in an atypical type A thymoma variant
Introduction
Type A thymomas have long been considered benign tumors because their clinical progression is so slow (1), but occasionally, cases of local recurrence or distant metastases have been reported (2,3). A pathological review of type A thymomas with postoperative tumor recurrence identified an aggressive subset of tumors; this atypical type A thymoma variant category was added to the WHO classification in 2015 (4).
Case presentation
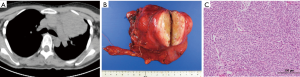
A mediastinal tumor had been discovered during routine X-ray screening in 2010 in a 35-year-old woman. A chest computerized tomography (CT) scan revealed a 6 cm non-invasive lobular tumor in the anterior mediastinum (Figure 1A). Although acetylcholine receptor antibody titers were elevated at 2.0 nmol/L, no signs of autoimmune disease such as myasthenia gravis were present. Extensive thymothymectomy was performed under median sternotomy allowing complete excision of the tumor with an adequate margin (Figure 1B). Pathologically, proliferation of spindle-shaped cells and oval-shaped cells were observed (Figure 1C), with no invasion into the fibrous capsules. Based on these findings, the patient was diagnosed with type A Masaoka Stage I thymoma. She was discharged 8 days after surgery, and followed at 6-month intervals.
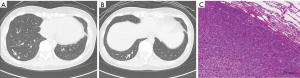
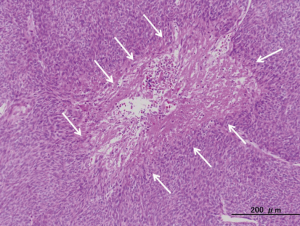
In 2014, a small nodule was discovered in the right lung at the 4-year post-surgical CT examination. In 2015, another small nodule was found in the right lung. In 2016, 6 years after surgery, a CT revealed that these two nodules were growing (Figure 2A,B), so the lung was partially resected for diagnosis and treatment. Oval-shaped small cells similar to those observed during the previous surgery were discovered (Figure 2C) and she was diagnosed with metastases of the type A thymoma. Since distant metastases were present, the primary tumor could have been an atypical type A thymoma variant. Previous pathological examinations were re-evaluated, revealing coagulative necrosis in the previous specimen (Figure 3), and the primary tumor was determined to be an atypical type A thymoma variant. The patient was discharged 4 days after surgery, and will continue to be followed.
Discussion
Type A thymomas are generally considered benign tumors because of their excellent prognosis (1). However, there have been a few reports of postoperative recurrence and distant metastases (2,3). In the wake of these reports, an atypical type A thymoma variant was added to the WHO classification as a new subtype in 2015 (4). Of note, diagnoses are based on pathological findings alone. The diagnostic criteria are as follows: (I) moderate to severe nuclear atypia; (II) increased mitotic activity; and (III) signs of necrosis (4,5).
Proliferation of oval-shaped tumor cells was confirmed histologically in the resected lung specimen and it appears certain that this was a recurrence. Although there was no concept of atypical type A thymoma variant when the primary tumor was initially treated, the pathology findings were re-evaluated since recurrence suggested it might be an atypical type A thymoma variant. Findings of mitosis and necrosis led to a diagnosis of atypical type A thymoma variant. Vladislav et al. reviewed their cases and reported that atypical type A thymoma accounted for 3.8% (23/600) of the 600 cases of type A thymoma they had experienced (2). Pathology findings should be re-evaluated since although the prevalence is low, it is highly likely that some of the cases diagnosed as type A thymoma in 2014 and earlier are actually this variant.
Vladislav et al. also reported that the recurrence rate of atypical type A thymoma variant was 43% (10/23) (2). These included 5 cases of lung metastasis and 4 cases of liver metastasis. Necrosis was the only factor associated with a poor prognosis of postoperative recurrence. Surprisingly, they reported that there was no significant correlation between the resection margin and tumor recurrence (2). In the present case, distant metastases occurred despite extended thymothymectomy with a sufficient margin. This supports the view that regardless of margin, necrosis is associated with a poor prognosis.
In summary, pathology should be re-evaluated in type A thymoma cases diagnosed in 2014 or earlier since these may include patients who actually have the more aggressive atypical type A thymoma. Patients with intratumoral necrosis diagnosed with atypical type A thymoma are at high risk of recurrence and will need careful follow-up. Type A thymoma has been considered as benign tumor because of its clinical progression (1), but there are reports of cases that developed local recurrence or distant metastasis (2,3). Analyzing pathological findings among type A thymoma with postoperative tumor recurrence, atypical type A thymoma variant was newly added in WHO classification as a thymoma family of small subset of aggressive tumors in 2015 (4).
Acknowledgements
The authors would like to thank Kenji Maehara and his co-worker for the review and advice in writing English.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Okumura M, Ohta M, Tateyama H, et al. The World Health Organization histologic classification system reflects the oncologic behavior of thymoma: a clinical study of 273 patients. Cancer 2002;94:624-32. [Crossref] [PubMed]
- Vladislav IT, Gökmen-Polar Y, Kesler KA, et al. The role of histology in predicting recurrence of type A thymomas: a clinicopathologic correlation of 23 cases. Mod Pathol 2013;26:1059-64. [Crossref] [PubMed]
- Nonaka D, Rosai J. Is there a spectrum of cytologic atypia in type a thymomas analogous to that seen in type B thymomas? A pilot study of 13 cases. Am J Surg Pathol 2012;36:889-94. [Crossref] [PubMed]
- Marx A, Chan J, Coindre JM, et al. The 2015 World Health Organization Classification of Tumors of the Thymus: Continuity and Changes. J Thorac Oncol 2015;10:1383-95. [Crossref] [PubMed]
- Hashimoto M, Shimizu S, Takuwa T, et al. A case of atypical type A thymoma variant. Surg Case Rep 2016;2:116. [Crossref] [PubMed]


