Anatomical considerations in bronchoscopy
Introduction
Bronchoscopy allows endoscopic examination of the tracheobronchial tree and is an essential modality in the diagnosis and treatment of abnormalities within or adjacent to the airways. A firm understanding of the normal anatomy and relationship to adjacent structures allows physicians to avoid complications and achieve optimal performance during endoscopic procedures.
Structural anatomy of airways
The trachea is a continuation of the larynx that extends from the lower border of the cricoid cartilage to the carina. An adult trachea averages 11.8 cm in length (1,2). Variations in length and diameter of the trachea correlate with the size and gender of the individual. Coronal dimensions in men range between 13 and 25 mm, with corresponding values in women ranging from 10 to 21 mm (2). The sagittal dimensions in men and women are 13 to 27 mm and 10 to 23 mm, respectively (2). The trachea is composed of approximately 17 to 21 C-shaped cartilaginous rings, each averaging 4 mm in size, that form the anterior and lateral walls. The membranous posterior wall is supported by the trachealis muscle, which can be identified by its longitudinal striations. These supporting structures give the tracheal lumen an ovoid shape in adults. Orientation within the trachea during the procedure can be determined by identifying the characteristic features of the tracheal walls. Alterations in tracheal diameter or shape may be resultant of aging or indicate the presence of a pathological condition. For example, chronic obstructive pulmonary disease may cause a softening of the tracheal rings, leading to a decrease in the anteroposterior diameter whereas Mounier-Kuhn syndrome may result in tracheal dilation (1,3,4).
As a bronchoscope proceeds down the trachea, the lumen narrows slightly as it approaches the carina. The carina, an important landmark, is a sharply demarcated, cartilaginous projection separating the orifices of the right and left mainstem bronchi (5). The bifurcation of the trachea can be estimated by the sternal angle, anteriorly and by the 5th thoracic vertebrae, posteriorly. Morphological changes in the carina are important diagnostic signs. If the carina is distorted or widened posteriorly, it may indicate subcarinal disease or mass involvement of the proximal airway (2).
At the carina, the trachea bifurcates into the right and left mainstem bronchus. The right mainstem bronchus lies in a more vertical orientation relative to the trachea, branching at an angle of about 25 degrees (1,2). In men and women, the average length from the carina to the take-off of the right upper lobe bronchus averages 2.0 and 1.5 cm, respectively (3). The right upper lobe bronchus trifurcates into the apical, posterior, and anterior divisions. In 3% of the population, an anatomical aberration occurs in which the right upper lobe bronchus originates from the trachea at the level of the carina (2). The right mainstem bronchus continues as the bronchus intermedius which gives rise to the middle lobe bronchus and lower lobe bronchus. The middle lobe bronchus bifurcates into medial and lateral branches. Segmental bronchi off the right lower lobe bronchus include the superior, anterior basal, medial basal, lateral basal and posterior basal divisions. The left main stem bronchus is more horizontally oriented relative to the trachea, branching at an angle of about 45 degrees (1,2). It is almost twice as long as the right mainstem bronchus, averaging 5.0 cm in men and 4.5 cm in women (3). Thus, distinctions between the right and left mainstem bronchus can be made based on orientation and length. The left mainstem bronchus divides into the upper lobe bronchus and lower lobe bronchus. The left upper lobe bronchus has a superior division and inferior division (also called the lingular bronchus), that supply the upper lobe and lingula, respectively. The superior division bifurcates into the apicoposterior segmental bronchus and anterior segmental bronchus. The lingular bronchus bifurcates into superior and inferior lingular segmental bronchi. The lower lobe bronchus consists of superior, lateral basal, anteromedial basal, and posterior basal segmental bronchi.
Relationship to adjacent structures
The relationship of the trachea with surrounding structures within the mediastinum is of important concern when performing more invasive procedures such as transbronchial needle aspiration (TBNA) or cervical mediastinoscopy. The esophagus and trachea share a common embryonic origin and remain in close proximity. The membranous posterior wall of the trachea rests on the esophagus, beginning at the level of the cricoid cartilage to the bifurcation at the carina. The proximal esophagus lies at the left, posterior border but at times may assume a more lateral position (1). Vertebral bodies lie on the right, posterior border of the trachea. The isthmus of the thyroid crosses anterior to the trachea at the level of the 2nd cartilaginous ring, with the right and left lobes of the gland sitting laterally. Several vessels off the aortic arch pass anterior to the mid-trachea distal to the thyroid. The first branch off the arch, the innominate artery, crosses the trachea obliquely from left to right before dividing into the right common carotid artery and right subclavian artery. Slightly left of the midline of the trachea, the aortic arch gives off its second branch, the left common carotid artery. Directly anterior to both the innominate artery and left common carotid artery, the left innominate vein crosses the trachea from right to left. Structures lateral to the trachea on the right side include the superior vena cava, azygos vein, and right innominate vein. The right recurrent laryngeal nerve branches from the vagus nerve and passes beneath the right subclavian artery before ascending lateral to the trachea and entering the larynx between the cricoid and thyroid cartilages. The azygos vein arches directly superior to the right mainstem bronchus at the level of the carina, before joining the superior vena cava. Structures lateral to the trachea on the left side include the arch of the aorta and left common carotid artery. The left mainstem bronchus passes beneath the aortic arch. The left recurrent laryngeal nerve originates from the vagus nerve at the level of the aortic arch and passes beneath the arch before it ascends laterally in the tracheoesophageal groove to the larynx. Anterior to the carina, the pulmonary trunk bifurcates, with the right and left pulmonary arteries passing anterior to the right and left mainstem bronchi, respectively. During mobilization of subcarinal and tracheobronchial lymph nodes, care must be taken as to not injure the pulmonary trunk. Branches of the pulmonary arteries generally follow the branching of the bronchopulmonary segments, with vasculature found anterior to the corresponding airways.
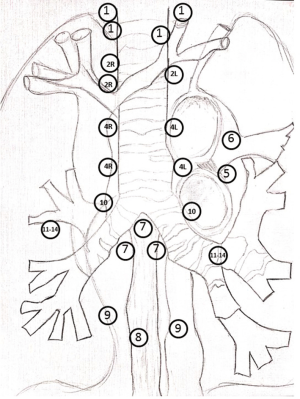
Lymphatic drainage follows the bronchi and pulmonary vessels, with multiple lymph node stations situated along the tracheobronchial tree and adjacent structures. Situated most peripherally are the subsegmental lymph nodes (station 14), segmental lymph nodes (station 13) and lobar lymph nodes (station 12). The interlobar nodes (stations 11R and 11L) lie between the origin of the lobar bronchi, with station 11Rs between the upper lobe bronchus and bronchus intermedius and station 11Ri between the middle and lower lobe bronchus. The hilar lymph nodes (station 10), also called the bronchopulmonary lymph nodes, lie immediately adjacent to the hilar vessels and the mainstem bronchus (2,6). Lymph nodes at stations 10 through 14 are categorized as N1 nodes. The pulmonary ligament lymph nodes (station 9) lie within the pulmonary ligament, with the inferior pulmonary vein and diaphragm marking their upper and lower border, respectively. Positioned to the right or left of the midline esophagus, the paraesophageal nodes (station 8) lie dorsal to the posterior wall of the trachea (2). Station 8 nodes extend from the upper border of the lower lobe bronchus on the left and the lower border of the bronchus intermedius on the right to the diaphragm (6). The subcarinal nodes (station 7) are positioned just inferior to the carina and extend inferiorly to the level of the upper border of the lower lobe bronchus (left) and the lower border of the bronchus intermedius (right). As mentioned previously, care must be taken during mobilization of the subcarinal nodes due to their close proximity to the bifurcation of the pulmonary trunk. Lymph nodes at stations 7, 8 and 9 are considered inferior mediastinal nodes. The subaortic lymph nodes (station 5) and para-aortic nodes (station 6) are categorized as aortic nodes. The subaortic lymph nodes lie lateral to the ligamentum arteriosum, with the aortic arch at the upper border and the left main pulmonary artery at the lower border. The para-aortic nodes are located anterior and lateral to the ascending aorta and aortic arch (6). The superior mediastinal nodes include stations 2,3, and 4. The right lower paratracheal nodes (station 4R) are anterolateral to the trachea, extending from the intersection of the innominate vein with the trachea to the lower border of the azygos vein (6). The left lower paratracheal nodes (station 4L) are found on the left, lateral border of the trachea, from the upper margins of the aortic arch to the left main pulmonary artery, just medial to the ligamentum arteriosum (6). Located posterior to the trachea, the retrotracheal nodes (station 3P) extend from the apex of the chest to the carina. The prevascular nodes (station 3A) are bordered, anteriorly, by the posterior aspect of the sternum and posteriorly, by the anterior border of the SVC (right) and the left carotid artery (left). Like the retrotracheal nodes, the prevascular nodes are positioned between the apex of the chest and the carina. The right (station 2R) and left (station 2L) upper paratracheal nodes are bordered superiorly by the apex of their respective lungs and the upper border of the manubrium. The lower border of the right upper paratracheal nodes is the intersection of the innominate vein with the trachea, whereas the left paratracheal nodes extend to the superior border of the aortic arch (6). The supraclavicular nodes include the low cervical, supraclavicular and sternal notch nodes. These lymph nodes extend from the cricoid cartilage to the clavicles and upper border of the manubrium, with the midline of the trachea serving as a border between stations 1R and 1L (6). A diagrammatic representation of the lymph node stations is depicted in Figure 1.
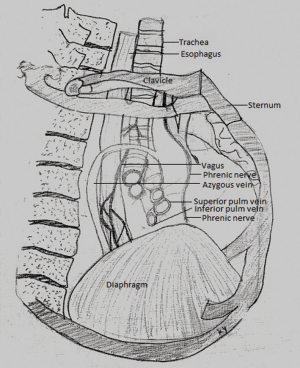
Anatomy of the right chest space
The medial border of the right chest space is formed by the thoracic vertebral bodies, posteriorly and the mediastinum including the pericardium, anteriorly (Figure 2). The thoracic cage forms the posterior, lateral and anterior walls. The right lung is divided into the upper, middle and lower lobes. The two fissures that divide the right lung are the right oblique and the horizontal. Variants in anatomy include an incomplete or a completely absent fissure. The structures of the hilum are enclosed by a pleural sleeve that is continuous with the pulmonary ligament. In the right hilum, the right main-stem bronchus is the most superior and posterior structure, with the pulmonary artery slightly anterior and inferior to it (2). The superior pulmonary vein is the most anterior of the right hilar structures. The superior and inferior pulmonary veins are situated inferior and anterior to the pulmonary artery and bronchus (5). The azygos vein can be identified on the right lateral surface of the thoracic vertebral bodies. It arches over the root of the right lung at the hilum and empties into the superior vena cava (7). The right phrenic nerve can be identified as it travels inferiorly along the superior vena cava and passes onto the pericardium, toward the diaphragm. The thoracic portion of the right sympathetic chain courses vertically, along the heads of the ribs (2,7). As mentioned previously, the proximal esophagus lies at the left, posterior border of the trachea beginning at the level of the cricoid cartilage to the bifurcation at the carina. After passing the aortic arch, the esophagus inclines forward and passes in front of the descending aorta, maintaining this position left of midline through the esophageal hiatus (2).
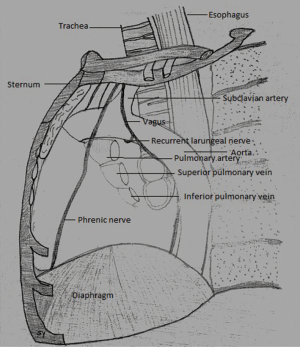
Anatomy of the left chest space
As with the right chest space, the medial wall of the left chest space is formed by thoracic vertebral bodies, posteriorly and the mediastinum containing the pericardium and heart, anteriorly (7) (Figure 3). The left lung is divided into the upper and lower lobes by the left oblique fissure. The structures of the hilum are enclosed by the pleural sleeve and include the left main-stem bronchus, left pulmonary artery and left pulmonary veins. Different from the right hilum, the pulmonary artery lies anterior and superior to the bronchus with the left pulmonary veins situated posterior and inferior (7). At the level of the hilum, the aorta arches over the hilar structures and descends posteriorly, anterior to the thoracic vertebral bodies. The ligamentum arteriosum can be found between the left pulmonary artery and the aortic arch. Similar to the right side, the left phrenic nerve travels inferiorly, first crossing anteromedial to the aortic arch before passing onto the pericardium and through the muscular part of the diaphragm (2,7). As discussed previously, the left recurrent laryngeal nerve originates from the vagus nerve at the level of the aortic arch and passes beneath the arch before it ascends laterally in the tracheoesophageal groove. The left vagus nerve, after giving off the left recurrent laryngeal branch, descends behind the left pulmonary hilum. The thoracic portion of the sympathetic chain can be found coursing along the heads of the ribs, similar to the right side. As noted above, the esophagus assumes a position anterior to the thoracic aorta once passing the aortic arch. As a result, access to the proximal esophagus is difficult from the left hemothorax due to the overlying aortic arch (2).
Summary
Bronchoscopy is a minimally invasive procedure that allows both diagnostic and therapeutic intervention in diseases of the airways. A thorough understanding of tracheal and bronchial anatomy, including the relationships to adjacent structures, is integral to the performance of safe and effective endoscopic procedures.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Minnich DJ, Mathisen DJ. Anatomy of the trachea, carina, and bronchi. Thorac Surg Clin 2007;17:571-85. [Crossref] [PubMed]
- Sellke F, del Nido PJ, Swanson SJ. Sabiston and Spencer Surgery of the Chest. 9th Edition. Philadelphia, PA: Elsevier, 2015:12-65.
- Campos JH. Update on tracheobronchial anatomy and flexible fiberoptic bronchoscopy in thoracic anesthesia. Curr Opin Anaesthesiol 2009;22:4-10. [Crossref] [PubMed]
- Al-Qadi MO, Artenstein AW, Braman SS. The "forgotten zone": acquired disorders of the trachea in adults. Respir Med 2013;107:1301-13. [Crossref] [PubMed]
- Moore KL, Dalley AF, Agur AM. Clinically Oriented Anatomy. 7th edition. Philadelphia: Lippincott Williams & Wilkins, 2013:114-24.
- Harisinghani MG. Atlas of Lymph Node Anatomy. New York, NY: Springer, 2013:31-57.
- Kaminsky D. The Netter Collection of Medical Illustrations: Respiratory System. 2nd edition. Elsevier Health Sciences, 2011.