Laparoscopic repair of a peritoneopericardial diaphragmatic hernia after a convergent procedure for the treatment of atrial fibrillation
Introduction
Peritoneopericardial diaphragmatic hernia was first described in the literature by French surgeons in 1903 (1). Since then, over 80 cases have been reported in the English literature. Diaphragmatic hernia has two primary etiologies: congenital and traumatic (2). The minority of cases are due to congenital etiology (3,4).
In congenital diaphragmatic hernia, the theorized dysfunction results from developmental failure of the pleuroperitoneal canals to close during the 8th and 10th week of gestation (4). The embryologic dysfunction is theorized to be due to irregular development of the ventral mesoderm, which develops into the lower sternum, antero-medial portion of the diaphragm, and diaphragmatic portion of the pericardium. Most patients with congenital diaphragmatic hernia present early in life due to pulmonary hypoplasia as a secondary process to the hernia (5).
Most peritoneopericardial diaphragmatic hernias are due to high velocity blunt trauma to the abdomen or the chest with motor vehicle accidents being the most common mechanism of injury. Diaphragmatic hernia secondary to blunt trauma could present early in the course of the injury or have delayed presentation. Peritoneopericardial diaphragmatic hernia arising from penetrating injury has also been described, but is less common (2).
Iatrogenic causes of peritoneopericardial diaphragmatic hernia have been described following various surgical procedures within both the thoracic and abdominal cavity (3). One well documented example is due to placement of a mediastinal drain through the peritoneum following a coronary artery bypass grafting (CABG) procedure (6,7). Other examples include hernia following laparoscopic procedures such as liver transplant, cholecystectomy, hepatectomy, splenectomy, and gastrectomy (3).
In our case, peritoneopericardial diaphragmatic hernia was a complication of a convergent procedure for the treatment of atrial fibrillation. The convergent procedure is a hybrid surgical and electrophysiological intervention for atrial fibrillation where epicardial and endocardial ablation is performed concurrently (8). The surgical approach utilizes a 10–15 mm cannula via a 3 cm subxiphoid incision to access the pericardium. The abdomen is first entered and inflated with CO2, and then an incision is created through the central tendon of the diaphragm, above the left lobe of the liver to gain access for ablation. A probe is then inserted through the diaphragmatic pericardial defect. Using radio frequency, the surface accessory conduction pathways are ablated. Following completion of the transabdominal component, the probe is removed and the abdomen is desufflated without primary closure of the diaphragmatic defect (8). To date, this is the first case of peritoneopericardial diaphragmatic hernia following a convergent procedure.
Case presentation
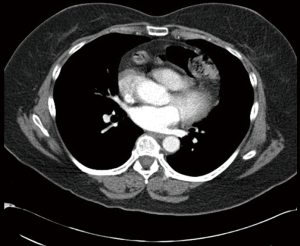
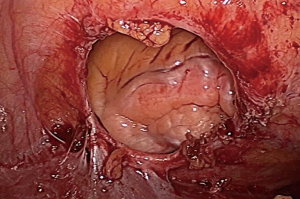
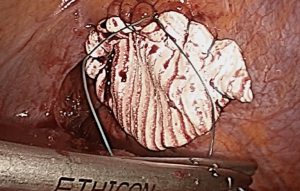
We report on a case of a 56-year-old female with significant surgical history of convergent procedure for treatment of atrial fibrillation 9 months prior, who presented to the emergency room with shortness of breath. The chest computed tomography scan showed the greater omentum and portions of the transverse colon extending from the abdomen into the pericardium through a peritoneopericardial diaphragmatic hernia (Figure 1). Elective laparoscopic repair of the hernia was performed. The hernia contents were reduced after minimal lysis of adhesions. A very well circumscribed 3 cm × 3 cm diaphragmatic defect was identified (Figure 2). The defect was repaired using a 7 cm × 7 cm GORE DUALMESH (WL Gore & Assoc, Flagstaff, AZ). An Endo Stitch (Covidien, New Haven, CT) was used to run a 0 ETHIBOND (Ethicon, Somerville, NJ) suture circumferentially around the defect (Figure 3). The Mesh was then fenestrated to avoid a postoperative pericardial effusion. The total operative time was 78 minutes. The patient was discharged uneventfully on postoperative day 2. At 2-week and 6-month follow up, the patient remained asymptomatic.
Discussion
Peritoneopericardial diaphragmatic hernia is a rare hernia seen most commonly secondary to blunt trauma to the abdomen or the chest (2). The etiology of our patient’s hernia was due to the insertion of a 15 mm cannula in the pericardial portion of the diaphragm for cardiac ablation in the treatment of atrial fibrillation.
The typical presenting symptoms in patients with peritoneopericardial diaphragmatic hernia include chest or abdominal pain, obstructive symptoms due to bowel herniation and incarceration, cardiac tamponade, or fatigue (3). Our patient presented with shortness of breath secondary to mass effect on the heart and lungs produced by the abdominal contents within the thoracic cavity.
Diagnosis of peritoneopericardial diaphragmatic hernia can often be difficult. In a review of 82 cases of peritoneopericardial diaphragmatic hernia due to trauma, 37 patients (48%) were diagnosed immediately during the acute phase, and 37 patients (48%) had delayed diagnosis with the interval being 23 days to 23 years after trauma (2). This illustrates the importance of close observation in a patient status post blunt abdominal trauma. In contrast to trauma, the presentation of congenital diaphragmatic hernia is usually soon after birth due to the sequelae of pulmonary hypoplasia in utero (4).
In respect to diagnosis, chest radiographic imaging may show an air fluid level in the anterior mediastinum. The gold standard in diagnosis is computerized tomography of the chest, which will reveal herniation of intra-abdominal structures into the pericardial space. Echocardiography allows further visualization of herniated viscera in the pericardium, as well as functional imagining of the heart. However, most peritoneopericardial diaphragmatic hernias were diagnosed intraoperatively during lifesaving surgery in treatment of blunt trauma (2).
The repairs of peritoneopericardial diaphragmatic hernia were traditionally preformed with an open surgical technique, but there are reports of four cases of laparoscopic repair. The hernias in these reports were secondary to blunt trauma, penetrating trauma, and congenital etiology. In all cases but one, the presentation was late onset with interval of 2 months to 36 years (9-12). Our case is the first documented laparoscopic repair of a peritoneopericardial diaphragmatic hernia secondary to a convergent procedure.
Primary repair with nonabsorbable sutures or mesh repair with nonabsorbable sutures have been successfully performed without any complications in our literature review in all cases with follow up between 2 to 11 months (9-12). In our case, the 3 cm × 3 cm diaphragmatic defect would not be approximated primarily due to high tension. We therefore decided to place a 7 cm by 7 cm synthetic mesh to bridge the defect.
Multiple fenestrations were created to prevent accumulation of pericardial effusion and cardiac tamponade, which has been observed in 3 of the 82 cases (3.6%) of surgical repair in peritoneopericardial diaphragmatic hernia (2). Sugarbaker et al. observed 328 patients undergoing extra pleural pneumonectomies for mesothelioma. Twelve of the 328 patients (3.6%) developed pericardial tamponade after reconstruction of the pericardium leading them to advocate for routine fenestrations for all pericardial reconstructions (13). Fenestrations are likely to be sufficient for drainage of pericardial fluid into the peritoneum without placement of a pericardial drain. Pericardial drains were not placed in any of the laparoscopic repairs, which led us to believe that it was not necessary in our procedure (9-12). Based on our experience and the few other reports in the literature; laparoscopic repair of peritoneopericardial diaphragmatic hernia is both safe and effective. In the future, surgeons should consider primary closure of the diaphragmatic defect during completion of the convergent procedure to avoid the potential complication we treated in our case report.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- DeCardinal. Grenier, Bourderou. Hernie diaphragmatique du colon transverse dans le pericarde chez un adulte. J Med Bourdeaux 1903;23:22.
- Reina A, Vidaña E, Soriano P, et al. Traumatic intrapericardial diaphragmatic hernia: case report and literature review. Injury 2001;32:153-6. [Crossref] [PubMed]
- Soufi M, Meillat H, Le Treut YP. Right diaphragmatic iatrogenic hernia after laparoscopic fenestration of a liver cyst: report of a case and review of the literature. World J Emerg Surg 2013;8:2. [Crossref] [PubMed]
- Zhang G, Liu D, Wang G, et al. Congenital intrapericardial diaphragmatic hernia with omphalocele. Hernia 2014;18:423-5. [Crossref] [PubMed]
- Kluth D, Tenbrinck R, von Ekesparre M, et al. The natural history of congenital diaphragmatic hernia and pulmonary hypoplasia in the embryo. J Pediatr Surg 1993;28:456-62; discussion 462-3. [Crossref] [PubMed]
- Waller DA, Satur CM, Mitchell IM, et al. Iatrogenic peritoneopericardial hernia following coronary artery bypass surgery. Eur J Cardiothorac Surg 1992;6:156-7. [Crossref] [PubMed]
- Takiuchi H, Totsugawa T, Tamaki T, et al. Intrapericardial diaphragmatic hernia after coronary artery bypass grafting using the right gastroepiploic artery graft: report of a case. Ann Thorac Cardiovasc Surg 2011;17:624-7. [Crossref] [PubMed]
- Zembala MO, Suwalski P. Minimally invasive surgery for atrial fibrillation. J Thorac Dis 2013;5 Suppl 6:S704-12. [PubMed]
- Al-Ghnaniem R, Ahmed I, Bosanac Z, et al. Successful laparoscopic repair of acute intrapericardial diaphragmatic hernia secondary to penetrating trauma. J Trauma 2009;67:E181-2. [Crossref] [PubMed]
- McCutcheon BL, Chin UY, Hogan GJ, et al. Laparoscopic repair of traumatic intrapericardial diaphragmatic hernia. Hernia 2010;14:647-9. [Crossref] [PubMed]
- Kuy S, Juern J, Weigelt J. Laparoscopic repair of a traumatic intrapericardial diaphragmatic hernia. JSLS 2014;18:333-7. [Crossref] [PubMed]
- Tyagi S, Steele J, Patton B, et al. Laparoscopic repair of an intrapericardial diaphragmatic hernia. Ann Thorac Surg 2014;97:332-3. [Crossref] [PubMed]
- Sugarbaker DJ, Jaklitsch MT, Bueno R, et al. Prevention, early detection, and management of complications after 328 consecutive extrapleural pneumonectomies. J Thorac Cardiovasc Surg 2004;128:138-46. [Crossref] [PubMed]