The new transbronchial diagnostic approach for the metastatic lung tumor from renal cell carcinoma—a case report
Introduction
Endobronchial ultrasound-guided needle aspiration (EBUS-TBNA) is a well-established procedure with high diagnostic yield and safety (1-3). Even though the complication rate is quite low, the standard 22 gauge needles sometimes cause major bleeding, particularly in hypervascular tumors (4). Renal cell carcinoma (RCC) is one of the well-known hypervascular tumors (5), and the metastatic lung tumor from RCC often represents hypervascularity as well. Therefore, several reports have warned against the high risk of hemorrhage in bronchoscopy when the target lesion has the potential for the metastasis from RCC (4,6-9).
Recently, the new 25 gauge needles have been used to perform diagnostic EBUS-TBNA. These kinds of thinner needles are already available in endoscopic ultrasound-guided fine needle aspiration (EUS-FNA), and are reported as effective with comparable diagnostic accuracy to standard 22 gauge needles (10). Besides, 25 gauge needles were reported to be superior to 22 gauge needles in terms of manipulability (11,12) and safety (12). Here we present a case of metastatic RCC, diagnosed successfully using the new 25 gauge needle by EBUS-TBNA without any major complications.
Case presentation
A 63-year-old ex-smoking male, who had undergone left nephrectomy 15 years ago for RCC, and a segmental pancreatectomy following this, 8 years ago for metastasis, was found to have a solitary pulmonary nodule at his routine check-up computed tomography (CT). The chest CT revealed a well defined round nodule 13 mm in size with high contrast uptake in his right lower lobe (Figure 1A-C). Subsequent positron emission tomography (PET)-CT showed non-specific 18F-fluorodeoxyglucose uptake (maximum standardized uptake value was 1.34) at the nodule (Figure 1D), and there was no other abnormality detected in his whole body. Though a high clinical suspicion was present for metastatic RCC, a tissue diagnosis was necessary for further treatment in the form of lobectomy, as the lesion was central in location. CT-guided or surgical biopsy of the lesion was not a feasible option due to its location. Thus, he was referred to our department for histopathologic diagnosis of the lesion by EBUS-TBNA.
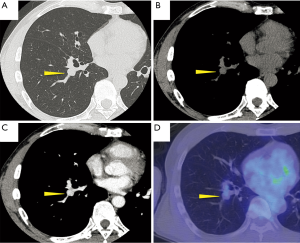
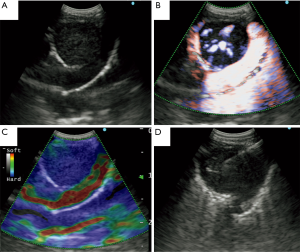
The lesion was present adjacent to right B9+10 (Figure 1A), and planned to be approached by EBUS-TBNA. Since there was a high risk of bleeding, considering the suspicion to be metastatic RCC (4), a choice was made to use the new 25 gauge needle (ExpectTM Pulmonary, Boston Scientific, USA) in place of the 22 gauge needle. The EBUS B-mode showed round shaped heterogeneous nodule (Figure 2A). Besides, while High Resolution Flow mode showed rich aberrant vessels inside the nodule, Elastography showed blue-dominant: it means hard nodule (Figure 2B,C). We punctured the nodule 3 times carefully using the 25 gauge needle taking care not to touch the blood vessel nearby (Figure 2D). During and after the procedure there was no major intrabronchial bleeding.
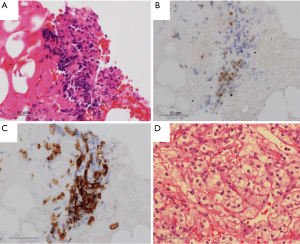
The obtained core tissue revealed a small cluster of atypical epithelial cells (Figure 3A) showing positivity for both PAX8 and CD10 in immunohistochemistry (Figure 3B,C). In view of these findings, the histopathological diagnosis of “suspicious tumor cells, compatible with metastatic RCC” was made. Following this, he underwent right lower lobectomy, and the pathological diagnosis of metastatic RCC was made (Figure 3D) that had the features similar to both the preoperative study (Figure 3A-C) and the primary tumor. His postoperative course was uneventful, and he was discharged on postoperative day 3 without any complications.
Discussion
In the present case, we were able to obtain a definitive diagnosis of the metastatic lung tumor from RCC by EBUS-TBNA using the new 25 gauge needle without any major complications.
Twenty-five gauge needles are already introduced to EUS-FNA, and are considered as one of the standard devices. In contrast to the existing concern that the 25 gauge needles extract less tissue, recent studies have proven that they have similar diagnostic outcome to the 22 gauge needles (13), and are also reported to have as comparable diagnostic outcome as per meta-analysis (10). To add to this, due to its thinner size, 25 gauge needles were described to have lower complication rate (12) and the better manipulability (11,12). Thus, this thinner needle enabled us to perform EBUS-TBNA without any major complications for the hypervascular metastatic RCC.
Similar to EUS-FNA, EBUS-TBNA is a well-established procedure with high diagnostic yield and safety: the cumulative sensitivity, specificity, and complication rate are 90–93%, 99–100%, and 1.23% respectively (1-3,14). Particularly in primary lung cancer, EBUS-TBNA is performed not only for initial diagnosis, but also for nodal staging (14) and re-biopsy for mutational analysis (15). As mentioned above, metastatic RCC is one of the most hemorrhagic tumors (5-9), together with some other hypervascular tumors: e.g., carcinoid and papilloma. Most bronchoscopic procedure performed on these hypervascular tumors have to be terminated prematurely due to uncontrollable bleeding (4). In these situations, the specimens also represent non-diagnostic sample with a lot of blood cells usually.
Alternative procedures for obtaining tissue for diagnosis of thoracic tumors include CT-guided percutaneous needle biopsy or aspiration, and surgical biopsy. CT-guided percutaneous needle biopsy or aspiration were thought unsuitable for this nodule because the nodule was located in the central area and surrounded with many blood vessels and bronchi (Figure 2). Surgical biopsy is also a good option for tissue sampling (16), but it needs general anesthesia, and adds to morbidity of the patient. In this case, less invasive surgery such as wedge resection was technically impossible because of the location of the nodule, while major lobectomy as a diagnostic procedure would not be appropriate given the aggressiveness of the surgery.
Therefore, we selected EBUS-TBNA using the new 25 gauge needle for this lesion. Although there was no previous report, it might be a preferable option for the diagnosis of hemorrhagic tumors like a metastatic lung tumor from RCC.
Conclusions
In the present case, we were able to obtain a definitive diagnosis of the metastatic lung tumor from RCC by EBUS-TBNA using the 25 gauge needle without any major complications. This new thin 25 gauge needle might be a useful option for the diagnosis of tumor that is suspected to be hypervascular.
Acknowledgements
Funding: This work was supported by the National Cancer Center Research and Development Fund (29-A-13).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
References
- Yasufuku K, Chiyo M, Koh E, et al. Endobronchial ultrasound guided transbronchial needle aspiration for staging of lung cancer. Lung Cancer 2005;50:347-54. [Crossref] [PubMed]
- Asano F, Aoe M, Ohsaki Y, et al. Complications associated with endobronchial ultrasound-guided transbronchial needle aspiration: a nationwide survey by the Japan Society for Respiratory Endoscopy. Respir Res 2013;14:50. [Crossref] [PubMed]
- Gu P, Zhao YZ, Jiang LY, et al. Endobronchial ultrasound-guided transbronchial needle aspiration for staging of lung cancer: a systematic review and meta-analysis. Eur J Cancer 2009;45:1389-96. [Crossref] [PubMed]
- Evison M, Crosbie PA, Booton R. Thoracic metastasis from renal cell carcinoma: bronchoscopic and EBUS images. J Bronchology Interv Pulmonol 2015;22:55-7. [Crossref] [PubMed]
- Heidenreich A, Ravery V. Preoperative imaging in renal cell cancer. World J Urol 2004;22:307-15. [Crossref] [PubMed]
- Dobbertin I, Dierkesmann R, Kwiatkowski J, et al. Bronchoscopic aspects of renal cell carcinoma (RCC). Anticancer Res 1999;19:1567-72. [PubMed]
- Sakumoto N, Inafuku S, Shimoji H, et al. Endobronchial metastasis from renal cell carcinoma: report of a case. Surg Today 2000;30:744-6. [Crossref] [PubMed]
- Reddy C, Michaud G, Majid A, et al. Photodynamic therapy in the management of endobronchial metastatic lesions from renal cell carcinoma. J Bronchology Interv Pulmonol 2009;16:245-9. [Crossref] [PubMed]
- Suyama H, Igishi T, Makino H, et al. Bronchial artery embolization before interventional bronchoscopy to avoid uncontrollable bleeding: a case report of endobronchial metastasis of renal cell carcinoma. Intern Med 2011;50:135-9. [Crossref] [PubMed]
- Affolter KE, Schmidt RL, Matynia AP, et al. Needle size has only a limited effect on outcomes in EUS-guided fine needle aspiration: a systematic review and meta-analysis. Dig Dis Sci 2013;58:1026-34. [Crossref] [PubMed]
- Camellini L, Carlinfante G, Azzolini F, et al. A randomized clinical trial comparing 22G and 25G needles in endoscopic ultrasound-guided fine-needle aspiration of solid lesions. Endoscopy 2011;43:709-15. [Crossref] [PubMed]
- Lee JK, Lee KT, Choi ER, et al. A prospective, randomized trial comparing 25-gauge and 22-gauge needles for endoscopic ultrasound-guided fine needle aspiration of pancreatic masses. Scand J Gastroenterol 2013;48:752-7. [Crossref] [PubMed]
- Micames CG, McCrory DC, Pavey DA, et al. Endoscopic ultrasound-guided fine-needle aspiration for non-small cell lung cancer staging: A systematic review and metaanalysis. Chest 2007;131:539-48. [Crossref] [PubMed]
- Dong X, Qiu X, Liu Q, et al. Endobronchial ultrasound-guided transbronchial needle aspiration in the mediastinal staging of non-small cell lung cancer: a meta-analysis. Ann Thorac Surg 2013;96:1502-7. [Crossref] [PubMed]
- Kirita K, Izumo T, Matsumoto Y, et al. Bronchoscopic Re-biopsy for Mutational Analysis of Non-small Cell Lung Cancer. Lung 2016;194:371-8. [Crossref] [PubMed]
- Amos AM, Kim FH, McRoberts JW. The utility of video-assisted thoracic surgery in the diagnosis of pulmonary metastases from renal cell carcinoma. Urology 1997;49:123-7. [Crossref] [PubMed]


