Airway stenting in patients requiring intubation due to malignant airway stenosis: a 10-year experience
Introduction
Malignant airway stenosis is often life-threatening. Emergency intubation and mechanical ventilation are frequently required, especially in critically ill patients with severe acute respiratory failure. Rigid bronchoscopic treatment, including airway stenting, has been widely used as palliative therapy (1-3) or bridging therapy (4-6) for malignant airway stenosis. However, only a few small studies and case reports have reported its usefulness for patients with severe acute respiratory failure requiring intubation due to malignant central airway obstruction (7-9). Therefore, its clinical role remains unclear. The aim of this study was to determine the efficacy and outcomes of airway stenting in patients with malignant airway stenosis requiring emergency intubation.
Methods
Patients
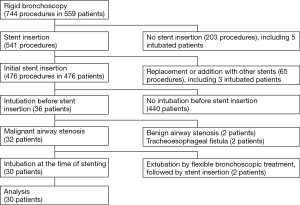
We performed 744 rigid bronchoscopic interventions for 559 patients during a 10-year period (from September 2005 to September 2015) at Nagoya Medical Center. Among the patients, 44 had airway stenosis that required intubation prior to rigid bronchoscopy. The following patients were excluded: five patients who did not undergo stenting, three with a history of prior stenting, two with benign airway stenosis, two with a tracheoesophageal fistula without airway stenosis, and two who could be extubated with bedside flexible bronchoscopic treatment followed by stenting. Thus, the medical records of the remaining 30 patients with malignant airway obstruction requiring emergency intubation followed by stenting were retrospectively reviewed. The patient flow is shown in Figure 1. Successful stenting was defined as no requirement for re-intubation within 48 hours after extubation (8). Prior to stent placement, written informed consent for the procedure was obtained from the patients’ families. The institutional review board of Nagoya Medical Center approved this study.
Procedures
Tracheal intubation was performed for patients with ventilation or oxygenation failure who could not wait until the start of the stenting procedures as determined by the primary physician. At our institution, we performed all stenting procedures using both rigid and flexible bronchoscopes under general anesthesia in the operating room. For airway stenosis, stenting was performed using a silicone straight stent (DUMON; Novatech, La Ciotat, France), silicone bifurcated stent (DUMON or OKI; Novatech), or self-expandable metal stent (Ultraflex, covered type; Boston Scientific, Natick, MA, USA) after bronchoscopic airway reestablishment using argon plasma coagulation, electrocautery, a CryoProbe, a high-pressure balloon, or the bevel of a rigid bronchoscope as previously described (10-12). After the stent insertion, acetylcysteine nebulization was performed three times daily. Stent removal under general anesthesia was performed whenever the primary physician considered it necessary; for example, when the tumor-specific therapy was successful or complications developed.
Statistical analysis
Continuous variables were analyzed using the Mann-Whitney U test, and dichotomous variables were analyzed using Fisher’s exact test. Multivariate analysis was performed using logistic regression analysis. Survival curves were calculated by the Kaplan-Meier method and compared using the log-rank test. The results were considered statistically significant at a two-tailed P value of ≤0.05. Statistical analyses were performed using a statistical software program (PASW Statistics 18; SPSS Inc., Chicago, IL, USA).
Results
The baseline characteristics of the 30 patients with malignant airway stenosis requiring emergency intubation prior to stenting procedures are shown in Table 1. The most frequent primary disease was lung cancer (17 of 30 patients, 57%), and the second most frequent was esophageal cancer (6 of 30 patients, 20%). Twenty-two patients (73%) had tracheal stenosis, and eight (26%) had bronchial but not tracheal stenosis. Of the eight patients with only bronchial stenosis, five had unilateral bronchial stenosis and three had bilateral main-stem bronchial stenosis. Twenty-one (70%) were chemoradiotherapy-naïve patients.
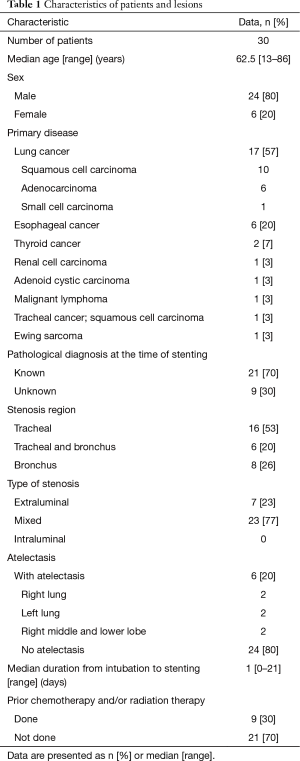
Full table
Details of the procedures are summarized in Table 2. Twenty-three patients (77%) underwent silicone stenting and seven (23%) underwent metallic stenting. Fourteen patients (47%) underwent airway reestablishment with mechanical coring, argon plasma coagulation, electrocautery, or cryorecanalization during the stenting procedures, and the remaining 16 patients (53%) underwent stent placement without airway reestablishment.
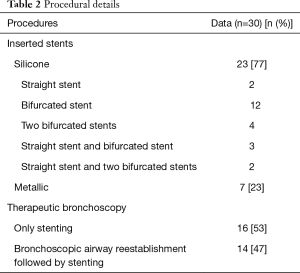
Full table
The clinical outcomes after stent placement are shown in Table 3. Extubation within 48 hours after stenting could be performed in 28 of 30 patients (93%). The two patients who could not be extubated had undergone tracheostomy. Although their tracheostomy tubes could not be removed, they were successfully removed from mechanical ventilation and supplemental oxygen. Twenty-eight patients (93%) could be removed from supplemental oxygen. A total of 21 patients (70%) underwent additional tumor-specific therapy, including chemotherapy and/or radiation therapy. Only 3 of 8 patients (38%) who had undergone prior chemoradiotherapy received additional tumor-specific therapy, while 18 of 21 chemoradiotherapy-naïve patients (86%) could receive additional therapy (P=0.019). Stents could be removed in four patients (13%) with a tumor response to chemotherapy and/or radiation therapy.
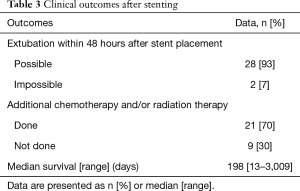
Full table
No significant complications occurred during the stenting procedures. Four patients underwent tracheostomy after stent placement. Of these four, two who could not be extubated had undergone tracheostomy because of difficulty coughing out sputum. One patient, who was able to be extubated once, underwent stent removal and tracheostomy due to retention of secretions 2 weeks after stent placement. The remaining patient, who was also successfully extubated once, developed convulsions of unknown origin accompanied by impaired consciousness and underwent tracheostomy to prevent retention of secretions 4 days after stent placement. In addition, granulation tissue formation requiring bronchoscopic resection 70 days after stent placement occurred in one patient, and pneumonia immediately after stenting occurred in another patient.
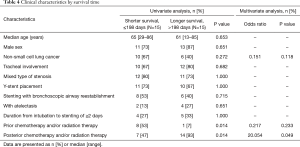
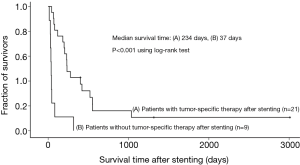
The median survival duration after stenting at the time of analysis was 198 days (range, 13–3,009 days). When patients were categorized into shorter and longer survival groups, the absence of prior chemotherapy and/or radiotherapy and the performance of posterior chemotherapy and/or radiotherapy were associated with the survival time in the univariate analysis; only the latter was associated with the survival time in the multivariate analysis (Table 4). The Kaplan-Meier method showed that the survival time was significantly longer in patients who received chemotherapy and/or radiation therapy after the procedure (234 vs. 37 days, respectively; P<0.001 using log-rank test) (Figure 2) and in chemoradiotherapy-naive patients (234 vs. 40 days, respectively; P<0.001 using log-rank test).
Full table
Discussion
To the best of our knowledge, this is the largest study on the utility of airway stenting for patients with malignant central airway stenosis requiring emergency endotracheal intubation. This study demonstrated the usefulness of airway stenting as a bridge as well as a palliation therapy for such patients. A total of 93% of patients could be extubated within 48 hours after stenting, and 86% of chemoradiotherapy-naive patients could receive chemotherapy and/or radiation therapy (which are associated with longer survival times) after the stenting procedures.
Endotracheal intubation is a recommended procedure for the treatment of life-threatening malignant central airway obstruction (2). However, its role is often temporary, and further interventions are necessary for more permanent relief of symptoms. External beam radiotherapy has been widely used for palliation of malignant airway obstruction (2,3); however, its role seems to be quite limited for intubated patients. Louie et al. (13) retrospectively evaluated the efficacy of external beam radiotherapy for 26 intubated patients with malignant airway obstruction. The median overall survival duration was only 0.36 months, and the extubation success rate was only 27%; extubation occurred a median of 8 days between initiating radiation therapy and extubation. Chemotherapy might be another choice for patients with chemosensitive tumors such as hematological malignancies (14,15) and small cell lung cancer (16). Song et al. (15) retrospectively investigated the outcomes and prognostic factors in critically ill cancer patients who were receiving chemotherapy in the intensive care unit. Of 38 mechanically ventilated patients with malignancies (most of which were hematologic malignancies) who received chemotherapy in the intensive care unit, 22 (58%) died in the intensive care unit. The authors found that respiratory failure requiring mechanical ventilation was an independent prognostic factor associated with intensive care unit mortality. The poor prognoses and the low success rates of extubation suggest that urgent intervention other than tumor-specific therapy is indispensable for the survival of intubated patients.
Bronchoscopic intervention, including stent placement, reportedly provides rapid relief from symptoms of malignant airway obstruction. To date, only a few small studies have been published on the usefulness of stenting for patients who have been intubated due to malignant central airway obstruction (7-9). Lin et al. (8) retrospectively investigated 26 mechanically ventilated patients (21 with malignant and 5 with benign central airway obstruction) who underwent metallic stent placement with a flexible bronchoscope in the intensive care unit. Fourteen (54%) could be removed from mechanical ventilation after the procedures. Murgu et al. (9) performed a retrospective study on the usefulness of bronchoscopic intervention in 12 consecutively intubated and mechanically ventilated patients with central airway obstruction due to non-small cell lung cancer. Eleven (92%) were successfully weaned, nine of whom could be extubated within 24 hours after therapeutic bronchoscopy. Boyd et al. (17) reviewed 12 studies on the utility of bronchoscopic interventions such as ablative therapies and stenting for patients with mechanical ventilation and found that the rate of removal from mechanical ventilation was 63% (range, 43–100%). The high success rates of extubation, including that in the present study, indicate that bronchoscopic intervention with airway stenting is a rapid and useful palliative therapy for intubated patients with malignant central airway stenosis. It is well known that airway stenting sometimes causes complications, such as retained secretions, granulation tissue formation, and stent migration (18). Although reported complication rates vary widely among studies, serious complications rarely occur (18,19). The complications in the current study were managed easily and seem to be acceptable.
Another role of airway stenting other than palliation in patients with malignant central airway obstruction is a bridge to additional tumor-specific therapies. This role of airway stenting has been reported to be associated with longer survival (20,21), which was again confirmed by the present study. Several investigators (4-6) have stated that temporary stenting, which has been characterized as a bridge to other therapies, is a useful therapeutic strategy for patients with malignant airway stenosis. In a prospective study by Witt et al. (4), 22 patients with severe malignant strictures underwent stent placement for primary palliation of dyspnea followed by tumor-specific therapy with the aim of stent removal. In 11 of the 22 patients, the stents could be removed after successful tumor-specific therapy. We also previously reported that temporary stenting was useful as a bridging therapy for patients with central airway stenosis caused by malignant lymphoma (6). The prognosis of inoperable malignant diseases other than malignant lymphoma is poor; thus, the stents could be removed in only four patients in the present study. However, airway stenting procedures enabled chemotherapy and/or radiation therapy in 86% of chemoradiotherapy-naive patients and seem to play an important role as bridging therapy.
The main limitation of the present study is its retrospective nature. Our institution plays a specialized role in bronchoscopic interventions in our region, and many patients have thus been referred for bronchoscopic treatment. In fact, 23 of the 30 patients were referred for bronchoscopic treatment from neighboring general or university hospitals. Some patients who could not be transferred to our institution or who the attending physician determined had no indications for stenting might have been excluded; this selection bias may have influenced our results. The efficacy of stenting is doubtless due to the high success rate of removing patients from mechanical ventilation in the present study, but large multicenter prospective studies are required to elucidate other details, including the indications for the procedure.
Conclusions
Airway stenting facilitates extubation in critically ill patients with malignant central airway stenosis. It is also useful as a bridge to additional therapies, especially for chemoradiotherapy-naïve patients.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This study was approved by the Institutional Review Board of Nagoya Medical Center (identifier: 2014-803).
References
- Morris CD, Budde JM, Godette KD, et al. Palliative management of malignant airway obstruction. Ann Thorac Surg 2002;74:1928-32; discussion 1932-3.
- Kvale PA, Selecky PA, Prakash UB, et al. Palliative care in lung cancer: ACCP evidence-based clinical practice guidelines (2nd edition). Chest 2007;132:368S-403S.
- Simoff MJ, Lally B, Slade MG, et al. Symptom management in patients with lung cancer: Diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 2013;143:e455S-e497S.
- Witt C, Dinges S, Schmidt B, et al. Temporary tracheobronchial stenting in malignant stenoses. Eur J Cancer 1997;33:204-8. [Crossref] [PubMed]
- Kim JH, Shin JH, Song HY, et al. Palliative treatment of inoperable malignant tracheobronchial obstruction: temporary stenting combined with radiation therapy and/or chemotherapy. AJR Am J Roentgenol 2009;193:W38-42. [Crossref] [PubMed]
- Oki M, Saka H. Temporary use of silicone stents for severe airway stenosis in untreated malignant lymphoma. J Bronchology Interv Pulmonol 2013;20:21-7. [Crossref] [PubMed]
- Colt HG, Harrell JH. Therapeutic rigid bronchoscopy allows level of care changes in patients with acute respiratory failure from central airways obstruction. Chest 1997;112:202-6. [Crossref] [PubMed]
- Lin SM, Lin TY, Chou CL, et al. Metallic stent and flexible bronchoscopy without fluoroscopy for acute respiratory failure. Eur Respir J 2008;31:1019-23. [Crossref] [PubMed]
- Murgu S, Langer S, Colt H. Bronchoscopic intervention obviates the need for continued mechanical ventilation in patients with airway obstruction and respiratory failure from inoperable non-small-cell lung cancer. Respiration 2012;84:55-61. [Crossref] [PubMed]
- Oki M, Saka H. Double Y-stenting for tracheobronchial stenosis. Eur Respir J 2012;40:1483-8. [Crossref] [PubMed]
- Oki M, Saka H. New dedicated bifurcated silicone stent placement for stenosis around the primary right carina. Chest 2013;144:450-5. [Crossref] [PubMed]
- Oki M, Saka H. Silicone Y-Stent Placement on the Secondary Left Carina. Respiration 2015;90:493-8. [Crossref] [PubMed]
- Louie AV, Lane S, Palma DA, et al. Radiotherapy for intubated patients with malignant airway obstruction: futile or facilitating extubation? J Thorac Oncol 2013;8:1365-70. [Crossref] [PubMed]
- Darmon M, Thiery G, Ciroldi M, et al. Intensive care in patients with newly diagnosed malignancies and a need for cancer chemotherapy. Crit Care Med 2005;33:2488-93. [Crossref] [PubMed]
- Song JU, Suh GY, Chung MP, et al. Risk factors to predict outcome in critically ill cancer patients receiving chemotherapy in the intensive care unit. Support Care Cancer 2011;19:491-5. [Crossref] [PubMed]
- Jennens RR, Rosenthal MA, Mitchell P, et al. Outcome of patients admitted to the intensive care unit with newly diagnosed small cell lung cancer. Lung Cancer 2002;38:291-6. [Crossref] [PubMed]
- Boyd M, Rubio E. The utility of interventional pulmonary procedures in liberating patients with malignancy-associated central airway obstruction from mechanical ventilation. Lung 2012;190:471-6. [Crossref] [PubMed]
- Miyazawa T, Miyazu Y, Iwamoto Y, et al. Stenting at the flow-limiting segment in tracheobronchial stenosis due to lung cancer. Am J Respir Crit Care Med 2004;169:1096-102. [Crossref] [PubMed]
- Ost DE, Ernst A, Grosu HB, et al. Complications Following Therapeutic Bronchoscopy for Malignant Central Airway Obstruction: Results of the AQuIRE Registry. Chest 2015;148:450-71. [Crossref] [PubMed]
- Jeon K, Kim H, Yu CM, et al. Rigid bronchoscopic intervention in patients with respiratory failure caused by malignant central airway obstruction. J Thorac Oncol 2006;1:319-23. [Crossref] [PubMed]
- Furukawa K, Ishida J, Yamaguchi G, et al. The role of airway stent placement in the management of tracheobronchial stenosis caused by inoperable advanced lung cancer. Surg Today 2010;40:315-20. [Crossref] [PubMed]