Cystic tumor of the atrioventricular node: a review of the literature
Introduction
Primary cardiac tumors are uncommon clinical entities with an incidence of 0.0017% to 0.03% of all autopsies where benign cardiac tumors more common than those that are malignant (1,2). Cystic tumor of the atrioventricular (AV) node, also known as mesothelioma of the AV node, is a benign congenital tumor that is located in the triangle of Koch in the AV nodal region of the atrial septum of the heart. As the AV node is an important component of the electrical conduction system of the heart allowing electrical signals initiated in the sinoatrial node to be distributed to the heart’s ventricles for contraction, any disruption to the AV node may result in sudden death. Cystic tumor of the AV node comprises of 2.7% of cardiac tumors and is the most common primary cardiac tumor causing sudden death (1,3). We herein review the etiology, presentation, differential diagnosis, diagnosis, management, surgical approaches and outcomes of this rare tumor.
Etiology
Despite its name, the cystic tumor of the AV node (or AV node mesothelioma) does not appear to have a mesothelial origin (1,4). The name is a misnomer as the lesion was named based on historical observations on its similarity with mesothelial cells and that of an adenomatoid tumor (5,6). The histogenesis is still an area of controversy. It is believed that the cystic tumor of the AV node originates during embryogenesis of the heart and is derived from congenital rests of endodermal origin (5-7) or ultimobranchial heterotopic elements similar to solid cell nests of the thyroid (8). The AV nodal region is an area of embryonic fusion in which these tissues may become trapped leading to formation of this tumor (7). Studies have indicated that 10% of individuals with cystic tumor of the AV node also have midline developmental defects along the central vertical body axis (1,9), suggestive of a genetic defect involving migration of embryological tissues (8) with possible familial occurrence (6). It has been suggested that in contrast to a true neoplasm, it is likely a result of dilatation of cystic spaces rather than cellular replication given an absence of mitoses in this tumor (10,11).
Presentation
Cystic tumor of the AV node is a tumor of congenital origin (1), first reported in 1911 (12). It has been diagnosed from between birth to 89 years of age with a mean age of diagnosis of 38 years and occurs primarily in women (female-male ratio of 3:1) (13). No racial or ethnic preference of the tumor has been noted. Tumors of the AV node have been associated with congenital abnormalities including complex congenital heart disease, thyroglossal duct cysts, cysts in the ovaries, breasts, ventricular septal defect, encephalocele (1) and has also been reported in association with Emery-Dreifuss muscular dystrophy, an X-linked recessive disease (14).
This lesion is often diagnosed post-mortem in nearly all published cases (15). As the tumor is believed to interfere with the heart’s electrical conduction system, it can lead to conduction defects resulting in complete heart block in over 65% of patients, and partial AV block in 15% of patients (4). Other conduction abnormalities that can cause arrhythmias include intra-atrial conduction defect, paroxysmal atrial arrhythmia and spontaneous intermittent pre-excitation through multiple left-sided accessory pathways or channelopathies (3,5,8,16). These arrhythmias can manifest with symptoms of palpitations, chest pain, shortness of breath, dizziness and syncope. Complications include associated heart attack, stroke and sudden cardiac death (1).
Differential diagnosis
The differential diagnosis includes bronchogenic cyst, mesothelial cyst and teratomas as well as histiocytoid cardiomyopathy, especially in the pediatric population, since the majority of infants present with a spectrum of arrhythmias (15,17). These can be differentiated from cystic tumor of the AV node by the appearance and number of germ cell layers. Bronchogenic cysts develop on the epicardial surface of the heart and are composed of mesoderm and endoderm (5). Mesothelial cysts are larger than cystic tumor of the AV node, develop on the surface of the heart and similar to bronchogenic cysts, they are composed of mesoderm and endoderm (5). Teratomas are composed of all three germ cell layers including the endoderm, mesoderm and ectoderm (18).
Diagnosis
Approach
An approach to the diagnosis of a cystic tumor of the AV node should begin with a complete evaluation of the patient’s medical and family history along with a thorough physical examination of the heart for abnormal heart sounds. Should there be clinical suspicion of underlying pathology, these patients should be followed up with an echocardiography (Echo), electrocardiogram, electrophysiological studies, magnetic resonance imaging (MRI) or computed tomography (CT) of the heart where the lesion may be high or low attenuating as deemed fit by a clinician (19,20). Concurrently, laboratory workup with extended electrolytes, complete blood count, thyroid hormone levels and levels of certain medications or drugs can be done to search for any trigger factors for arrhythmias. Given that the AV nodal artery mostly arises from the right coronary artery, selective angiogram may demonstrate a “tumor flush” or an abnormality of the course of this artery, suggestive of a cystic tumor of the AV node (21). If warranted, a tissue biopsy of the tumor including standard tissue blocks around the AV node, sinoatrial node, bundle of His, and regional samples from both ventricles (22) can be obtained for final diagnosis of cystic tumor of the AV node.
Pathology
Macroscopic findings of an cystic tumor of the AV node may reveal a small multicystic tumor with sizes ranging from 2 mm to 2 cm (1) and appear as a thickening of the atrial septum or as a slightly elevated lesion (23). The mass is located where the AV node is normally located, at the base of the atrial septum in Koch’s triangle. It often spans between the ostium of the coronary sinus in the right atrium to the membranous septum, along the top of the tricuspid valve septal leaflet (24). The lesion may not be prominent and can be easily missed. It has also been reported to exist in the thymus gland in one case (25), though nearly always exist inside the region of the AV junction. It has been recommended to take a routine section of the conducting system, including the AV node, in all cases of sudden death.
Microscopically, the lesion appears to be composed of cysts, ducts and solid nests of cells. The cystic areas are lined by nonciliated, epithelial-appearing flat or cuboidal benign cells that may be single or multilayered (main cells) mixed with occasional clear cells (neuroendocrine or C cells) (17). The nuclei are bland. The cell nests may resemble squamous or transitional epithelium and are embedded in a dense fibrous stroma that contains collagen and elastin fibers (6). There may also be squamous differentiation and calcification of luminal debris. Remnants of AV node are rarely identifiable. There may also be inflammatory cells and fibrosis. No smooth muscle, mitotic figures or atypia which would be suggestive of malignancy have been reported (13).
Immunohistochemically, the cells of the cystic tumor of the AV node stain with alcian blue and PAS, exhibiting resistance to both hyaluronidase and diastase digestion, respectively (23). The main cells of the lesion stain positive for cytokeratin CAM5.2, cytokeratin AE1/AE3, cytokeratin 34βE12, cytokeratin 5/6 (CK5/6), cytokeratin 7 (CK7), epithelial membrane antigen (EMA), carcinoembryonic antigen (CEA), carbohydrate antigen (CA)19.9, p63, bcl2, galectin 3 (13,26). The neuroendocrine cells of the lesion stain positive for CAM5.2, pan-keratin (AE1/AE3), CEA, calcitonin, chromogranin, synaptophysin and thyroid transcription factor 1 (TTF1) (13,16,17,26). The lesion overall stains negative for keratin 20 (CK20), p53, Bcl-2, cyclin D1, cytokeratin 20 (CK20), vimentin, CD31, factor VIII related antigen, estrogen receptor, progesterone receptor, thrombomodulin, Wilm’s tumor 1 and calretinin (13,16,17,26). This is in contrast to true mesothelium which stains positive for thrombomodulin, Wilm’s tumor 1, calretinin and negative for PAS (23). Ki-67 staining shows minimal proliferation (2%) (16). The immunohistochemistry profile for the cystic tumor of the AV node supports epithelial differentiation and a designation of this tumor as a form of endodermal heterotopia (16). This most likely reflects embryonic developmental factors with differentiation towards an upper foregut phenotype for the lesion rather than being mesothelial in origin (7,16).
On electron microscopy, the lesion appears as cells that form solid nests with a well formed basement membranes, cytoplasmic tonofilaments and desmosomes or glandular structures with desmosomes, electron-dense material and short microvilli (13).
Management
As pacemaker implantation does not prevent sudden death in patients with this tumor (27,28), surgical intervention should always be indicated upon diagnosis (17,29,30). There are various methods of excising the lesion. However, because of the rarity of the cystic tumor of the AV node coupled with an antemortem diagnosis of the lesion, methods of surgical resection and therapeutic concepts have not been standardized. Whether the lesion should be completely or partially resected from the intra-atrial septum base remains controversial. Presentation, methods of diagnosis, tumor size and location of previously described cases that were surgically managed are described in Table 1. Surgical approaches and outcomes of these cases are described in Table 2.
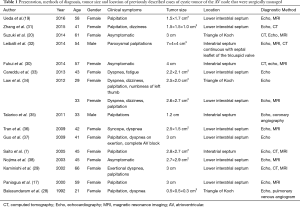
Full table
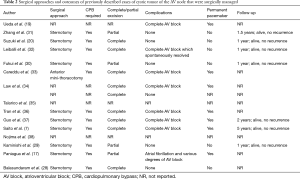
Full table
Complete excision
As cystic tumor of the AV node can result in sudden death due to ventricular tachycardia or fibrillation, complete resection is often done regardless if a pacemaker is required following resection (8,20,28,31-35). It can be accomplished using sternotomy, on cardiopulmonary bypass (CPB) with ascending aortic and direct bicaval cannulation (35). Following clamping of the ascending aorta, a right atriotomy (35) or biatrial transseptal incision (32) can be performed with the patient in cardioplegic arrest. The tumor is located in the right atrium and often widely attached to the atrial septum. The tumor can be opened; the fluid filled cavity suctioned and sent for rapid cytodiagnosis for malignant cells or bacteria in the fluid, then washed. The mass is then removed together with the part of the interatrial septum it is adherent to and sent to pathology (8,20,28,32-35). Temporary detachment of the tricuspid and mitral valves from their respective annulae may be required for mass excision (31). Following leaflet reattachment, atrium septoplasty is then performed with a polytetrafluroethylene (35) or pericardial patch (33).
Partial excision
As there are no reports on recurrence of the cystic tumor of the AV node following resection (30), some groups have attempted a partial excision to avoid injury to the conduction system and lessen the likelihood of heart block requiring pacemaker implantation (17,29,30,36). Partial excision of the cystic tumor of the AV node is similar in technique to the complete excision with the exception of the step of removing the mass. Careful estimation of the border between the atrial and cyst walls is required by examining the cyst from both inside and outside following drainage of cystic fluid. Only the cyst wall projecting into the right atrium is then resected by deroofing from the atrial surface (17,29,30,36).
Excision of the cystic tumor of the AV node by a minimally invasive approach has also been described via a 6-cm anterior minithoracotomy on peripheral CPB (34). After resection, close follow-up is needed to detect subsequent AV node dysfunction. Anti-arrhythmic medications and pacemaker implantation following excision may be necessary to manage any post excision AV block.
Prognosis
The prognosis of cystic tumor of the AV node is good with early diagnosis followed by prompt and complete surgical excision of the tumor. Cases of sudden cardiac death have shown that this tumor is associated with fatal cardiac dysrhythmia with partial-to-complete heart block (17,22). Thus even though the tumor is benign, the majority of individuals are diagnosed on post-mortem examination. Patients with a more atrial based site appear to have a better presentation with partial heart block (17,37). Tumor size does not appear to be associated with symptoms, lethal arrhythmia or sudden death (30).
Conclusions
Cystic tumor of the AV node is the most common primary cardiac tumor causing sudden cardiac death. Sudden cardiac death accounts for 50% of cardiovascular mortality (39). Given the lack of macroscopic clues to its presence, awareness of the possibility of the development of this tumor in a patient with heart block limited to the AV node or sudden cardiac death, both in children and young adults and particularly in women, warrants a detailed examination of the cardiac conduction system with sampling of cardiac tissue for final diagnosis (22). Decreased threshold for suspicion with prompt diagnosis and surgical excision may help prevent the fatal complications of this tumor.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Burke A, Tavora F. The 2015 WHO Classification of Tumors of the Heart and Pericardium. J Thorac Oncol 2016;11:441-52. [Crossref] [PubMed]
- Miller DV. Cardiac Tumors. Surg Pathol Clin 2012;5:453-83. [Crossref] [PubMed]
- Wolf PL, Bing R. The smallest tumor which causes sudden death. JAMA 1965;194:674-5. [Crossref] [PubMed]
- Cavanaugh J, Prahlow JA. Sudden cardiac death due to arrhythmogenic right ventricular cardiomyopathy and cystic tumor of the AV node. Forensic Sci Med Pathol 2013;9:407-12. [Crossref] [PubMed]
- Burke AP, Anderson PG, Virmani R, et al. Tumor of the atrioventricular nodal region. A clinical and immunohistochemical study. Arch Pathol Lab Med 1990;114:1057-62. [PubMed]
- Cameselle-Teijeiro J, Santías RR, Nallib IA, et al. Cystic tumor of the atrioventricular node: a rare cardiac pseudoneoplastic lesion. Arch Pathol Lab Med 2010;134:1584-6. [PubMed]
- Saito S, Kobayashi J, Tagusari O, et al. Successful excision of a cystic tumor of the atrioventricular nodal region. Circ J 2005;69:1293-4. [Crossref] [PubMed]
- Cameselle-Teijeiro J, Abdulkader I, Soares P, et al. Cystic tumor of the atrioventricular node of the heart appears to be the heart equivalent of the solid cell nests (ultimobranchial rests) of the thyroid. Am J Clin Pathol 2005;123:369-75. [Crossref] [PubMed]
- Wong J, Ball RY. Endodermal heterotopia of the atrioventricular node associated with transposition of the great arteries. Cardiovasc Pathol 2003;12:159-62. [Crossref] [PubMed]
- Ford SE. Congenital cystic tumors of the atrio-ventricular node: successful demonstration by an abbreviated dissection of the conduction system. Cardiovasc Pathol 1999;8:233-7. [Crossref] [PubMed]
- Thorgeirsson G, Liebman J. Mesothelioma of the AV node. Pediatr Cardiol 1983;4:219-23. [Crossref] [PubMed]
- Sharma G, Linden MD, Schultz DS, et al. Cystic tumor of the atrioventricular node: an unexpected finding in an explanted heart. Cardiovasc Pathol 2010;19:e75-8. [Crossref] [PubMed]
- Jones JSP, Lund C, Planteydt HT. Colour Atlas of Mesothelioma. 1st ed. Netherlands: Springer Verlag Gmbh; 2012.
- Strøm EH, Skjørten F, Stokke ES. Polycystic tumor of the atrioventricular nodal region in a man with Emery-Dreifuss muscular dystrophy. Pathol Res Pract 1993;189:960-4; discussion 965-7. [Crossref] [PubMed]
- Pan Y, Chen JL, Li ZJ, et al. Cystic tumour of the atrioventricular node: a case report and review of the literature. Chin Med J (Engl) 2012;125:4514-6. [PubMed]
- Evans CA, Suvarna SK. Cystic atrioventricular node tumour: not a mesothelioma. J Clin Pathol 2005;58:1232. [PubMed]
- Paniagua JR, Sadaba JR, Davidson LA, et al. Cystic tumour of the atrioventricular nodal region: report of a case successfully treated with surgery. Heart 2000;83:E6. [Crossref] [PubMed]
- Ali SZ, Susin M, Kahn E, et al. Intracardiac teratoma in a child simulating an atrioventricular nodal tumor. Pediatr Pathol 1994;14:913-7. [Crossref] [PubMed]
- Ueda K, Tagusari O, Kasao M. Cystic tumour of the atrioventricular node: can an electrophysiological study predict sudden death? Europace 2016;18:1334. [Crossref] [PubMed]
- Suzuki K, Matsushita S, Suzuki H, et al. Cystic Tumor of the Atrioventricular Node. J Thorac Imaging 2014;29:W97-9. [Crossref] [PubMed]
- Bharati S, Bicoff JP, Fridman JL, et al. Sudden death caused by benign tumor of the atrioventricular node. Arch Intern Med 1976;136:224-8. [Crossref] [PubMed]
- Davies MJ. The investigation of sudden cardiac death. Histopathology 1999;34:93-8. [Crossref] [PubMed]
- Fletcher CDM. Diagnostic Histopathology of Tumors. 4th edition. Elsevier Health Sciences 2013.
- Veinot JP. Cardiac tumors of adipocytes and cystic tumor of the atrioventricular node. Semin Diagn Pathol 2008;25:29-38. [Crossref] [PubMed]
- Duray PH, Mark EJ, Barwick KW, et al. Congenital polycystic tumor of the atrioventricular node. Autopsy study with immunohistochemical findings suggesting endodermal derivation. Arch Pathol Lab Med 1985;109:30-4. [PubMed]
- Arai T, Kurashima C, Wada S, et al. Histological evidence for cell proliferation activity in cystic tumor (endodermal heterotopia) of the atrioventricular node. Pathol Int 1998;48:917-23. [Crossref] [PubMed]
- Evans DW, Stovin PG. Fatal heart block due to mesothelioma of the atrioventricular node. Br Heart J 1986;56:572-4. [Crossref] [PubMed]
- Balasundaram S, Halees SA, Duran C. Mesothelioma of the atrioventricular node: first successful follow-up after excision. Eur Heart J 1992;13:718-9. [Crossref] [PubMed]
- Kaminishi Y, Watanabe Y, Nakata H, et al. Cystic tumor of the atrioventricular nodal region. Jpn J Thorac Cardiovasc Surg 2002;50:37-9. [Crossref] [PubMed]
- Fukui S, Mitsuno M, Yamamura M, et al. Partial resection of cystic tumor of atrioventricular node. Ann Thorac Surg 2014;98:2223-6. [Crossref] [PubMed]
- Zhang Y, Mei X, Zheng X. Surgical excision of a cystic tumor of the atrioventricular node complicating complete atrioventricular block. Zhonghua Xin Xue Guan Bing Za Zhi 2015;43:358-9. [PubMed]
- Leiballi E, Pecoraro R, Del Bianco F, et al. Incessant supraventricular tachycardia due to a cystic atrioventricular node tumor. Eur Heart J 2014;35:1209.
- Careddu L, Pantaleo A, Savini C, et al. Cystic atrioventricular node tumor excision by minimally invasive surgery. Ann Thorac Surg 2013;96:1873-5. [Crossref] [PubMed]
- Law KB, Feng T, Nair V, et al. Cystic tumor of the atrioventricular node: rare antemortem diagnosis. Cardiovasc Pathol 2012;21:120-7. [Crossref] [PubMed]
- Talarico F, Mirante Marini M, Gigliotti O, et al. Peculiar case of palpitations. Italian Journal of Medicine Conference: 16th Congresso Nazionale FADOIFirenze Italy 2011:106.
- Tran TT, Starnes V, Wang X, et al. Cardiovascular magnetic resonance diagnosis of cystic tumor of the atrioventricular node. J Cardiovasc Magn Reson 2009;11:13. [Crossref] [PubMed]
- Guo J, Zuo S, Lin C, et al. Surgical treatment of a giant cystic tumor of the atrioventricular nodal region. Interact Cardiovasc Thorac Surg 2009;8:592-3. [Crossref] [PubMed]
- Nojima Y, Ishibashi-Ueda H, Yamagishi M. Cystic tumour of the atrioventricular node. Heart 2003;89:122. [Crossref] [PubMed]
- Patel J, Patel S, Sheppard MN. Benign cardiac tumours associated with sudden death. Europace 2014;16:855-60. [Crossref] [PubMed]


