The Society for Translational Medicine: clinical practice guidelines for mechanical ventilation management for patients undergoing lobectomy
Introduction
Anesthesia for lobectomy in thoracic surgery is a great challenge because it requires single contralateral lung ventilation with collapse of the ipsilateral lung. Collapse of the operated lung and ventilation of the other lung may induce an inflammatory response (1). The ventilated lung is hyperperfused, receiving most of the cardiac output and may be damaged by mechanical ventilation. The collapsed lung is exposed to ischemia, reperfusion injury and shear stress on reexpansion and postresection ventilation. As a result, patients who undergo lobectomy postoperatively may develop compromised lung function. Acute lung injury, reduced lung compliance and hypoxemia and an increase in pro-inflammatory cytokines, all are reported (2-6). The aim of mechanical ventilation during one-lung ventilation is (I) to facilitate carbon dioxide elimination; (II) to maintain oxygenation; and (III) to minimize postoperative lung dysfunction. There have been numerous investigations performed to determine the most appropriate means of mechanical ventilation. In this study we systematically searched the literature and the evidence for each graded recommendation.
Materials and methods
Literature review
Systematic search was performed to identify articles related to mechanical ventilation settings in patients undergoing lobectomy (((((((“2000/01/01”[Date - Publication]: “3000”[Date - Publication]) AND Clinical Trial[ptyp])) AND (anesthesia AND Clinical Trial[ptyp])) AND (((ventilation) OR ventilator) OR tidal volume)) AND ((surgery) OR resection OR operation OR lobectomy)) AND ((pulmonary) OR lung)). Studies were considered to be eligible if they fulfill the following criteria: (I) the study population involved patients who underwent lobectomy; (II) the primary intervention involved mechanical ventilation strategy; (III) articles were published after January 1st, 2000.
Classification and levels of evidence were graded according to American College of Cardiology/American Heart Association (ACC/AHA) rules (Available at: http://assets.cardiosource.com/Methodology_Manual_for_ACC_AHA_Writing_Committees.pdf).
Results
Evidence synthesis
Our initial search identified 461 citations. Four hundred and ten were excluded because in 176 studies the investigated patients underwent operations other than lobectomy, 84 studies did not investigate mechanical ventilation and 100 were unrelated studies. The remaining 51 citations were considered to be eligible for the present review.
Therapeutic hypercapnia
One-lung ventilation has long been associated with inflammatory response manifested as imbalance between pro-inflammatory and anti-inflammatory cytokines (7,8). Such systemic inflammatory response may cause complications such as acute lung injury and therefore, therapeutic strategy to prevent the inflammatory response may be potentially beneficial to patients.
Hypercapnia, secondary to reduced alveolar ventilation has been noted as a component of protective lung ventilation in clinical practice (9). It has been shown in both clinical and experimental studies that therapeutic hypercapnia can ameliorate severity of sepsis, injury induced by mechanical ventilation, and acute respiratory distress syndrome (10-13). In patients undergoing lobectomy with one-lung ventilation, hypercapnia facilitates inhibition of local and systemic inflammatory responses (REF?). Postoperative respiratory function, assessed by peak plateau pressure and dynamic compliance, was improved by hypercapnia induced by inhaled CO2 (14). Hypercapnia has been shown to reduce systemic vascular resistance, increase cardiac index and pulmonary vascular resistance (15). Although these pilot studies are randomized controlled trials, they are small in sample size and will require more study in larger cohorts before stronger recommendations can be made. However, we can assume that hypercarbia is not harmful, except in the face of pulmonary hypertension, possibly cardiac arrhythmia and high intracranial pressure.
Recommendation
Permissive/therapeutic hypercapnia, to maintain a partial pressure of carbon dioxide of 50-70 mmHg potentially may be beneficial in patients undergoing single lung ventilation during pulmonary lobectomy operations (class IIa, level B).
Protective mechanical ventilation
Although low mechanical ventilation rate, higher levels of positive end-expiratory pressure (PEEP) and low inspired oxygen levels are considered to be “protective”, the primary components of protective ventilation (PV) include low tidal volume (LTV, tidal volume 6–8 mL/kg) and limited peak airway pressure, with or without PEEP. The landmark study by Amato and coworkers found that low tidal volume ventilation can effectively reduce mortality in patients with acute respiratory distress syndrome (ARDS) (16). Recent evidence also suggests potential beneficial effect of low tidal volume ventilation during general anesthesia for patients undergoing non-thoracic operative procedures (17-20).
During operative lobectomy with one-lung ventilation, results of PV in improving patients’ outcomes are confusing (Table 1) (21,22). Several studies failed to identify beneficial effects with PV strategy (21,23,24). Another randomized controlled trial favored the use of high tidal volume (HTV; 10 mL/kg) ventilation, as it resulted in less hypercarbia, less dead space, better dynamic compliance, and less postoperative atelectasis (25). However, in this small study (n=34 patients) there was no difference in postoperative morbidity, or length of stay with LTV or HTV. In another study, LTV was found to be associated with increased risk of arterial hypoxemia (26).
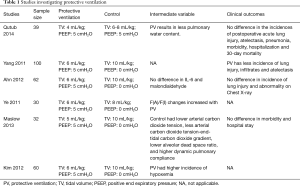
Full table
Arterial hypoxemia in the presence of an elevated inspired oxygen concentration (FIO2) is caused by right-to-left intrapulmonary shunting of blood, likely secondary to atelectasis. Low tidal volume ventilation has long been known to result in atelectasis, especially when FIO2 is high, as it usually is during one-lung ventilation. Therefore, when LTV is applied, basic physiologic principles and some reports support application of a recruitment maneuver, followed by application of PEEP and lower FIO2 (27,28).
This paragraph is out of place. There is no mention of FIO2 in the recommendation. Further, “protective ventilation” advocates do not mention FIO2 except as a mechanism to maintain PaO2 in the face of low PEEP. I recommend this be a part of the “open lung” discussion.
Recommendation
PV with tidal volume of 6–8 mL/kg and a PEEP of 5 cmH2O is reasonable based on current evidence (class IIa, level B).
Alveolar recruitment (open lung)
Alveolar recruitment is traditionally used to open collapsed lungs, which typically occur in acute respiratory distress syndrome, but there is scarce evidence to support the use of alveolar recruitment in patients undergoing lobectomy with one-lung ventilation. In a feasibility study, Downs and colleagues reported that open lung ventilation (another term used for alveolar recruitment), which is performed by initially setting the PEEP to 30 cmH2O, then adjusting the amount needed to maximize compliance, is safe and effective. A novel form of ventilation was applied to maintain the lung “open”. Apneustic anesthesia ventilation (AAV), similar to airway pressure release ventilation (APRV), utilized a continuous positive airway pressure (CPAP) of 15–30 cmH2O. Ventilation was accomplished by decreasing airway pressure for 1–2 s to allow exhalation of a tidal volume of 6 mL/kg, but not long enough to permit lung collapse. Further, patients did not receive supplemental O2, even on induction of general anesthesia, prior to extubation, or in the recovery room. Use of LTV, CPAP titrated to maximize lung-thorax compliance, FIO2 =0.21, low ventilator rate (6–8 BPM) and mild hypercarbia (48–52 mmHg) were associated with no PPC. In this cohort of 12 patients, there was no atelectasis or infiltrates, and there was no complication or mortality (29).
Arterial hypoxemia in the presence of an elevated inspired oxygen concentration (FIO2) is caused by right-to-left intrapulmonary shunting of blood, likely secondary to atelectasis. Low tidal volume ventilation has long been known to result in atelectasis, especially when FIO2 is high, as it usually is during one-lung ventilation. Therefore, when LTV is applied, basic physiologic principles and some reports support application of a recruitment maneuver, followed by application of PEEP and lower FIO2 (27,28).
Recommendation
Alveolar recruitment (open lung ventilation) may be potentially beneficial in patients undergoing lobectomy with one-lung ventilation (class IIb, level C). Low FIO2 may prevent absorption atelectasis.
Mode of mechanical ventilation
Different mode of mechanical ventilation may produce different pulmonary mechanics for patients during surgical procedures. For instance, volume controlled ventilation (VCV) guarantees the tidal volume of inspired gas, whereas pressure controlled ventilation (PCV) provides a preset pressure to the airway. In a crossover study, involving patients undergoing open thoracotomy with one lung ventilation, PCV offered improved right ventricle (RV) function compared with the use of VCV. No other clinical outcomes were reported in this study (30). In other studies, PCV did not provide any beneficial effect, except for reduced peak airway pressure during ventilation (31-33). In a small pilot study involving 30 patients, the pressure-controlled volume-guaranteed (PCV-VG) mode appeared to offer clinical benefits in terms of lung mechanics and pro-inflammatory cytokines (34). However, other long-term outcomes were not investigated in these studies. In elderly patients with compromised pulmonary function, PCV and PCV-VG were found to have significant beneficial effects on intraoperative oxygenation and airway pressure (35-37).
Recommendation
PC or PCV-PG is recommended over VCV and can be used in patients undergoing lung resection with single-lung ventilation (class IIa, level B).
Pre-and post-operative noninvasive ventilation
CPAP is commonly used for patients with respiratory failure. Patients undergoing lung resection are at increased risk of postoperative acute lung injury. In a recent randomized controlled trial, CPAP applied for 6 h after operation was able to improve the oxygenation index at 24 h as compared to supplemental oxygen through a Venturi mask. Other clinical outcomes such as postoperative pulmonary complications and duration of stay in the post-anesthesia care unit (PACU) and hospital were not different between groups (38). Similar results are found in another study with smaller sample size (39). CPAP can be delivered via Boussignac CPAP system and helmet. In patients with a preoperative FEV1 <70%, pre- and post-operative use of pressure support ventilation significantly reduced pulmonary dysfunction following lobectomy (40).
Recommendation
CPAP can be used in patients undergoing lobectomy and one lung ventilation, and is beneficial in improving short-term oxygenation (class IIa, level A).
Non-intubated thoracoscopic lobectomy
In recent years, some authors have reported the use of thoracoscopic lobectomy performed under epidural anesthesia, intrathoracic vagal blockade, sedation and spontaneous breathing, without tracheal intubation. Non-intubated patients had significantly shorter duration of anesthesia and other clinical outcomes were comparable (41). Occasionally, conversion to conventional one-lung ventilation is necessary (42). One retrospective study reported a conversion rate of 5.5% (13/238) (43). The technique is feasible, and there were no severe complications reported. Safety and efficacy need to be investigated in larger trials (44,45). To date, no randomized controlled trial investigating the efficacy and safety of this technique has been published. The technique is feasible, and there were no severe complications reported. Safety and efficacy need to be investigated in larger trials (44,45).
Recommendation
Thoracoscopic lobectomy without tracheal intubation may be an alternative to conventional one-lung ventilation, in selected patients (class II, level C).
Inspiratory to expiratory ratio (I:E)
The setting of I:E ratio in controlled mechanical ventilation has been shown to have clinical important clinical impact on patients undergoing lobectomy with one-lung ventilation. A study involving 56 patients showed that setting I:E ratio to 1:1 as compared to 1:2 can reduce airway pressures and improve pulmonary compliance, but cannot significantly improve arterial oxygenation (46). Similar findings were reported in patients with low diffusion capacity of lung for carbon monoxide (47). AAV reported by Bratzke and Downs utilized an I:E of 2:1 to 4:1, as discussed earlier, with no PPC (48).
Recommendation
Controlled mechanical ventilation with I:E ratio of 1:1, or greater, is reasonable in patients undergoing one-lung ventilation (class IIa, level B).
Low inspired oxygen concentration
There is a pervasive, but scientifically unsupported assumption that higher inspired oxygen concentrations yield a protective and beneficial effect during thoracic surgical procedures. However, absorption atelectasis rapidly occurs within minutes of induction of general anesthesia with high FIO2 and detection of deterioration in lung function may be delayed significantly (27).
Few clinical trials have even mentioned FIO2, a variable that likely has a profound influence on atelectasis, postoperative work of breathing, and, possibly, PPCs (49,50).
Recommendation
Application of the lowest FIO2 necessary to maintain satisfactory arterial oxygen saturation is reasonable (REF Downs).
Adjuvant drug use
Preoperative nebulized budesonide was found to be effective in reducing peak and plateau pressure during mechanical ventilation. The effects of the drug lasted to the postoperative period where lung compliance was improved and pro-inflammatory cytokines were reduced after lung re-expansion (51). The use of intravenous sivelestat, a selective neutrophil elastase inhibitor, was effective in limiting inflammatory response and improving oxygenation (52,53). In a single RCT it was reported that preoperative injection of ulinastatin at 5,000 U/kg could attenuate local pulmonary inflammatory response in one-lung ventilation (54).
Recommendation
Adjuvant drugs such as nebulized budesonide, intravenous sivelestat and ulinastatin may have beneficial effect in attenuating inflammatory response following one-lung ventilation (class IIa, level B).
Acknowledgements
The authors would like to thank the secretaries Grace S. Li (Science Editor, The Society for Translational Medicine. Email: lsl@amegroups.com) and Maxine Y. Feng (Science Editor, The Society for Translational Medicine. Email: fengyp@amegroups.com) for their help and comments on this guideline.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Della Rocca G, Coccia C. Acute lung injury in thoracic surgery. Curr Opin Anaesthesiol 2013;26:40-6. [Crossref] [PubMed]
- Ng CSH, Wan S, Yim APC, Arifi AA. Pulmonary dysfunction after cardiac surgery. Chest 2002;121:1269-77. [Crossref] [PubMed]
- Ng CS, Wan S, Yim AP. Pulmonary ischaemia-reperfusion injury: role of apoptosis. Eur Respir J 2005;25:356-63. [Crossref] [PubMed]
- Ng CS, Wan S, Arifi AA, et al. Inflammatory response to pulmonary ischemia-reperfusion injury. Surg Today 2006;36:205-14. [Crossref] [PubMed]
- Ng CS, Arifi AA, Wan S, et al. Ventilation during cardiopulmonary bypass: impact on cytokine response and cardiopulmonary function. Ann Thorac Surg 2008;85:154-62. [Crossref] [PubMed]
- Ng CS, Wan S, Ho AM, et al. Gene expression changes with a “non-injurious” ventilation strategy. Crit Care 2009;13:403. [Crossref] [PubMed]
- Sugasawa Y, Yamaguchi K, Kumakura S, et al. The effect of one-lung ventilation upon pulmonary inflammatory responses during lung resection. J Anesth 2011;25:170-7. [Crossref] [PubMed]
- Lohser J, Slinger P. Lung Injury After One-Lung Ventilation: A Review of the Pathophysiologic Mechanisms Affecting the Ventilated and the Collapsed Lung. Anesth Analg 2015;121:302-18. [Crossref] [PubMed]
- Fuchs H, Mendler MR, Scharnbeck D, et al. Very low tidal volume ventilation with associated hypercapnia--effects on lung injury in a model for acute respiratory distress syndrome. PLoS One 2011;6:e23816. [Crossref] [PubMed]
- Nichol AD, O'Cronin DF, Naughton F, et al. Hypercapnic acidosis reduces oxidative reactions in endotoxin-induced lung injury. Anesthesiology 2010;113:116-25. [Crossref] [PubMed]
- Laffey JG, Tanaka M, Engelberts D, et al. Therapeutic hypercapnia reduces pulmonary and systemic injury following in vivo lung reperfusion. Am J Respir Crit Care Med 2000;162:2287-94. [Crossref] [PubMed]
- Citerio G, Bakker J, Bassetti M, et al. Year in review in Intensive Care Medicine 2013: I. Acute kidney injury, ultrasound, hemodynamics, cardiac arrest, transfusion, neurocritical care, and nutrition. Intensive Care Med 2014;40:147-59. [Crossref] [PubMed]
- Hickling KG, Walsh J, Henderson S, et al. Low mortality rate in adult respiratory distress syndrome using low-volume, pressure-limited ventilation with permissive hypercapnia: a prospective study. Crit Care Med 1994;22:1568-78. [Crossref] [PubMed]
- Gao W, Liu DD, Li D, et al. Effect of Therapeutic Hypercapnia on Inflammatory Responses to One-lung Ventilation in Lobectomy Patients. Anesthesiology 2015;122:1235-52. [Crossref] [PubMed]
- Sticher J, Müller M, Scholz S, et al. Controlled hypercapnia during one-lung ventilation in patients undergoing pulmonary resection. Acta Anaesthesiol Scand 2001;45:842-7. [Crossref] [PubMed]
- Amato MB, Barbas CS, Medeiros DM, et al. Effect of a protective-ventilation strategy on mortality in the acute respiratory distress syndrome. N Engl J Med 1998;338:347-54. [Crossref] [PubMed]
- Zhang Z, Hu X, Zhang X, et al. Lung protective ventilation in patients undergoing major surgery: a systematic review incorporating a Bayesian approach. BMJ Open 2015;5:e007473. [Crossref] [PubMed]
- Chaney MA, Nikolov MP, Blakeman BP, et al. Protective ventilation attenuates postoperative pulmonary dysfunction in patients undergoing cardiopulmonary bypass. J Cardiothorac Vasc Anesth 2000;14:514-8. [Crossref] [PubMed]
- Futier E, Constantin JM, Paugam-Burtz C, et al. A trial of intraoperative low-tidal-volume ventilation in abdominal surgery. N Engl J Med 2013;369:428-37. [Crossref] [PubMed]
- Choi G, Wolthuis EK, Bresser P, et al. Mechanical ventilation with lower tidal volumes and positive end-expiratory pressure prevents alveolar coagulation in patients without lung injury. Anesthesiology 2006;105:689-95. [Crossref] [PubMed]
- Qutub H, El-Tahan MR, Mowafi HA, et al. Effect of tidal volume on extravascular lung water content during one-lung ventilation for video-assisted thoracoscopic surgery: a randomised, controlled trial. Eur J Anaesthesiol 2014;31:466-73. [Crossref] [PubMed]
- Yang M, Ahn HJ, Kim K, et al. Does a protective ventilation strategy reduce the risk of pulmonary complications after lung cancer surgery?: a randomized controlled trial. Chest 2011;139:530-7. [Crossref] [PubMed]
- Ahn HJ, Kim JA, Yang M, et al. Comparison between conventional and protective one-lung ventilation for ventilator-assisted thoracic surgery. Anaesth Intensive Care 2012;40:780-8. [PubMed]
- Ye FF, Li LW. Effects of different ventilation modes for one-lung ventilation anesthesia on respiratory function and F(A)/F(I) changes during sevoflurane inhalation. Nan Fang Yi Ke Da Xue Xue Bao 2011;31:714-7. [PubMed]
- Maslow AD, Stafford TS, Davignon KR, et al. A randomized comparison of different ventilator strategies during thoracotomy for pulmonary resection. J Thorac Cardiovasc Surg 2013;146:38-44. [Crossref] [PubMed]
- Kim SH, Jung KT, An TH. Effects of tidal volume and PEEP on arterial blood gases and pulmonary mechanics during one-lung ventilation. J Anesth 2012;26:568-73. [Crossref] [PubMed]
- Downs JB, Smith RA. Increased inspired oxygen concentration may delay diagnosis and treatment of significant deterioration in pulmonary function. Crit Care Med 1999;27:2844-6. [Crossref] [PubMed]
- Downs JB. Is supplemental oxygen necessary? J Cardiothorac Vasc Anesth 2006;20:133-5. [Crossref] [PubMed]
- Downs JB, Robinson LA, Steighner ML, et al. Open lung ventilation optimizes pulmonary function during lung surgery J Surg Res 2014;192:242-9. [Crossref] [PubMed]
- Al Shehri AM, El-Tahan MR, Al Metwally R, et al. Right ventricular function during one-lung ventilation: effects of pressure-controlled and volume-controlled ventilation. J Cardiothorac Vasc Anesth 2014;28:880-4. [Crossref] [PubMed]
- Unzueta MC, Casas JI, Moral MV. Pressure-controlled versus volume-controlled ventilation during one-lung ventilation for thoracic surgery. Anesth Analg 2007;104:1029-33. tables of contents. [Crossref] [PubMed]
- Pardos PC, Garutti I, Piñeiro P, et al. Effects of ventilatory mode during one-lung ventilation on intraoperative and postoperative arterial oxygenation in thoracic surgery. J Cardiothorac Vasc Anesth 2009;23:770-4. [Crossref] [PubMed]
- Song SY, Jung JY, Cho MS, et al. Volume-controlled versus pressure-controlled ventilation-volume guaranteed mode during one-lung ventilation. Korean J Anesthesiol 2014;67:258-63. [Crossref] [PubMed]
- Hu X, Shen H, Li X, et al. Effects of volume-controlled ventilation and pressure-controlled volume- guaranteed mode during one-lung ventilation on circulation, pulmonary function and lung injury. Zhonghua Yi Xue Za Zhi 2014;94:1006-9. [PubMed]
- Lin F, Pan L, Qian W, et al. Comparison of three ventilatory modes during one-lung ventilation in elderly patients. Int J Clin Exp Med 2015;8:9955-60. [PubMed]
- Lin F, Pan L, Huang B, et al. Pressure-controlled versus volume-controlled ventilation during one-lung ventilation in elderly patients with poor pulmonary function. Ann Thorac Med 2014;9:203-8. [Crossref] [PubMed]
- Pu J, Liu Z, Yang L, et al. Applications of pressure control ventilation volume guaranteed during one-lung ventilation in thoracic surgery. Int J Clin Exp Med 2014;7:1094-8. [PubMed]
- Garutti I, Puente-Maestu L, Laso J, et al. Comparison of gas exchange after lung resection with a Boussignac CPAP or Venturi mask. Br J Anaesth 2014;112:929-35. [Crossref] [PubMed]
- Barbagallo M, Ortu A, Spadini E, et al. Prophylactic use of helmet CPAP after pulmonary lobectomy: a prospective randomized controlled study. Respir Care 2012;57:1418-24. [PubMed]
- Perrin C, Jullien V, Vénissac N, et al. Prophylactic use of noninvasive ventilation in patients undergoing lung resectional surgery. Respir Med 2007;101:1572-8. [Crossref] [PubMed]
- Wu CY, Chen JS, Lin YS, et al. Feasibility and safety of nonintubated thoracoscopic lobectomy for geriatric lung cancer patients. Ann Thorac Surg 2013;95:405-11. [Crossref] [PubMed]
- Chen JS, Cheng YJ, Hung MH, et al. Nonintubated thoracoscopic lobectomy for lung cancer. Ann Surg 2011;254:1038-43. [Crossref] [PubMed]
- Hung MH, Chan KC, Liu YJ, et al. Nonintubated thoracoscopic lobectomy for lung cancer using epidural anesthesia and intercostal blockade: a retrospective cohort study of 238 cases. Medicine (Baltimore) 2015;94:e727. [Crossref] [PubMed]
- Hung MH, Hsu HH, Chen KC, et al. Nonintubated thoracoscopic anatomical segmentectomy for lung tumors. Ann Thorac Surg 2013;96:1209-15. [Crossref] [PubMed]
- Hung MH, Hsu HH, Cheng YJ, et al. Nonintubated thoracoscopic surgery: state of the art and future directions. J Thorac Dis 2014;6:2-9. [PubMed]
- Kim SH, Choi YS, Lee JG, et al. Effects of a 1:1 inspiratory to expiratory ratio on respiratory mechanics and oxygenation during one-lung ventilation in the lateral decubitus position. Anaesth Intensive Care 2012;40:1016-22. [PubMed]
- Lee K, Oh YJ, Choi YS, et al. Effects of a 1:1 inspiratory to expiratory ratio on respiratory mechanics and oxygenation during one-lung ventilation in patients with low diffusion capacity of lung for carbon monoxide: a crossover study. J Clin Anesth 2015;27:445-50. [Crossref] [PubMed]
- Bratzke E, Downs JB, Smith RA. Intermittent CPAP: a new mode of ventilation during general anesthesia. Anesthesiology 1998;89:334-40. [Crossref] [PubMed]
- Hedenstierna G. Small tidal volumes, positive end-expiratory pressure, and lung recruitment maneuvers during anesthesia: good or bad? Anesthesiology 2015;123:501-3. [Crossref] [PubMed]
- Hedenstierna G. Oxygen and anesthesia: what lung do we deliver to the post-operative ward? Acta Anaesthesiol Scand 2012;56:675-85. [Crossref] [PubMed]
- Ju NY, Gao H, Huang W, et al. Therapeutic effect of inhaled budesonide (Pulmicort® Turbuhaler) on the inflammatory response to one-lung ventilation. Anaesthesia 2014;69:14-23. [Crossref] [PubMed]
- Kawahara Y, Ninomiya I, Fujimura T, et al. Prospective randomized controlled study on the effects of perioperative administration of a neutrophil elastase inhibitor to patients undergoing video-assisted thoracoscopic surgery for thoracic esophageal cancer. Dis Esophagus 2010;23:329-39. [Crossref] [PubMed]
- Eguchi T, Yoshida K, Kondo R, et al. Sivelestat prevents cytoskeletal rearrangements in neutrophils resulting from lung re-expansion following one-lung ventilation during thoracic surgery. Inflammation 2013;36:1479-84. [Crossref] [PubMed]
- Li W, Wang J, Jiang YB, et al. Effects of ulinastatin on interleukin-8 during one-lung ventilation in surgery. Ai Zheng 2003;22:1074-6. [PubMed]


