SYNTAX score may predict the severity of atherosclerosis of the ascending aorta
Introduction
SYNTAX score was first introduced as an angiographic tool to objectively quantify the complexity of coronary artery disease (CAD) (1). SYNTAX score has since become an integral part of the decision-making process in patients undergoing intervention for three-vessel or left main CAD. In fact, in the latest US and European guidelines for myocardial revascularization, recommendations for the treatment strategies for these patients with complex coronary disease—either coronary artery bypass grafting (CABG) or percutaneous coronary intervention (PCI)—are based on the SYNTAX score (2,3). SYNTAX score has been identified as an independent predictor of mortality and major adverse cardiac or cerebrovascular events during follow-up especially in patients who undergo PCI (4,5). In patients who undergo CABG, the role of SYNTAX score as a prognostic indicator is not certain (4) and often times the score is considered irrelevant once surgery is indicated. However, it may be reasonable to assume that the complexity and degree of CAD represented by SYNTAX score is the surrogate of systemic atherosclerosis (6,7). This study was therefore designed to investigate the association of SYNTAX score with the severity of atherosclerosis mainly focusing on the ascending aorta, the most surgically relevant location in CABG.
Methods
Study population
We retrospectively analyzed 152 patients who underwent isolated CABG between October 2011 and December 2015 at the Mount Sinai Hospital. Patients were included in the study only when both SYNTAX score and grading of the severity of atherosclerosis in the ascending aorta were available. SYNTAX score was calculated preoperatively and prospectively on all patients undergoing coronary angiography in our catheterization laboratory. Patients who underwent concomitant valve operations and previous cardiac surgery were excluded. The study population was then stratified into three groups based on SYNTAX score with the cut-offs used in the current US/European guidelines [low score ≤22 (n=40), intermediate score 23–32 (n=44), and high score ≥33 (n=76)] (2,3). The study protocol was approved by the Icahn School of Medicine at Mount Sinai Institutional Review Board (IRB#: 15-01013).
Assessment of atherosclerosis in the ascending aorta
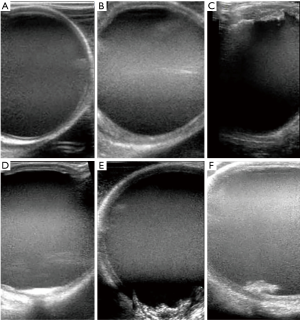
The severity of atherosclerosis in the ascending aorta was assessed by intraoperative epiaortic ultrasound imaging. During the study period, epiaortic imaging was routinely performed when aortic manipulation was required either for cross-clamping for cardiopulmonary bypass in the on-pump approach or side-clamping for proximal anastomosis to the ascending aorta in the off-pump approach. The severity of atherosclerosis was graded on a 5-point scale (Figure 1), compatible with the American Society of Echocardiography guideline (8). Grade III or greater atherosclerosis was considered to be severe.
Statistical analysis
Continuous variables are expressed as means with standard deviations. Categorical variables are expressed as proportions. Differences between groups were detected using the χ2-test for categorical variables, analysis of variance for normally distributed continuous variables, and the Kruskal-Wallis test for non-normally distributed continuous variables. Linear regression and logistic regression analysis were performed to test univariate and multivariate predictors of severe atherosclerosis (Grade III or greater). SYNTAX score was entered into the model as an independent variable in categorical and continuous format. In categorical format, SYNTAX score was categorized as low (≤22), intermediate [23–32], and high (≥33) score and the odds ratio (OR) for the SYNTAX score is shown with low scores as a reference. In continuous format, the OR is shown for each 10 score increment. For multivariate analyses, predefined regression models were used with covariates considered of potential predictors of severe atherosclerosis. The model fit and predictive power of logistic regression were validated with the Hosmer and Lemeshow goodness-of-fit test and c statistic, respectively. Correlation analysis between each variable was performed (Pearson or Spearman as appropriate) to ensure no violation of the assumption of multicollinearity (the cut-off correlation coefficient <0.7). Receiver operating characteristics (ROC) analysis was used to identify the level of SYNTAX score that best predicts severe atherosclerosis. The area under the ROC curve was used to assess the predictive ability. Results are demonstrated as beta in linear regression and OR and 95% confidence intervals (CI) in logistic regression. All tests were two tailed. A P value of <0.05 was considered to be statistically significant. The statistical analysis was performed using IBM SPSS Statistics for Windows, version 20.0 (SPSS, Inc., IBM Corporation, Armonk, NY, USA).
Results
Patient characteristics
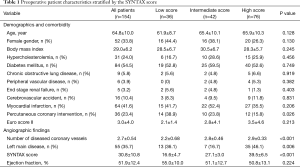
Baseline patient demographics and co-morbidity stratified by SYNTAX score are summarized in Table 1 and are comparable with the exceptions of less prevalence of prior PCI in higher SYNTAX groups (P=0.026). Age, left ventricular ejection fraction, and Euro SCORE II were not different in each group. The overall STNTAX score ranged from 2 to 62, with a mean of 31±11. Mean scores for each group were 17±5, 27±3, and 40±7, respectively (P<0.001). As expected, the number of diseased coronary vessels (2.9±0.3, P<0.001) and the prevalence of left main disease (46%, P=0.006) was highest in the high SYNTAX score group.
Full table
SYNTAX score and the severity of atherosclerosis
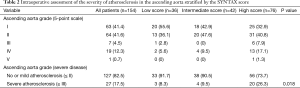
Intraoperative findings of severity of atherosclerosis in the ascending and descending aorta are summarized in Table 2. The overall prevalence of severe atherosclerosis of the ascending aorta and descending aorta were 17.5% and 62.2%. Patients with higher SYNTAX scores tended to have more severe atherosclerosis (8.3% vs. 9.5% vs. 26.3% in the ascending aorta, P=0.018; and 40.0% vs. 76.7% vs. 65.8% in the descending aorta, P=0.002).
Full table
Predictors of severe atherosclerosis in the ascending aorta
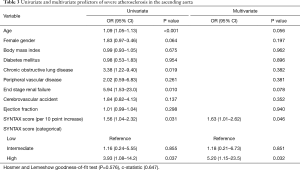
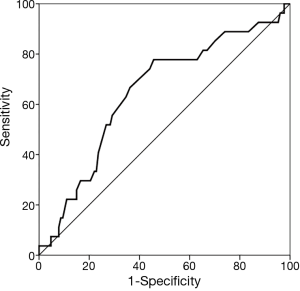
Logistic regression analysis was performed using the covariates listed in Table 3 to investigate the predictors of severe atherosclerosis in the ascending aorta. In univariate analysis, the following were found to be predictors: age (OR 1.1, 95% CI: 1.1–1.1, P<0.001), chronic obstructive lung disease (OR 3.3, 95% CI: 1.2–9.4, P=0.019), end-stage renal failure (OR 5.9, 95% CI: 1.5–23.0, P=0.010), SYNTAX score as a continuous variable [OR 1.6, 95% CI: 1.0–2.3, P=0.031 (per 10 point increment)], and SYNTAX score as a categorical variable [OR 3.9, 95% CI: 1.1–14.2, P=0.037 (high vs. low)]. In multivariate analysis adjusting for all covariates, SYNTAX score remained an independent predictor [OR 1.6, 95% CI: 1.0–2.6, P=0.046 (per 10 point increment) and OR 5.2, 95% CI: 1.2–23.5, P=0.032 (high vs. low)]. Similar results were obtained in a multivariate linear regression model with SYNTAX score as an independent predictor (beta 0.18, P=0.041). ROC analysis showed the area under the ROC curve for SYNTAX score was 0.65 (0.53–0.76) (Figure 2). SYNTAX score cut-off value of 22 was associated with 89% sensitivity and 26% specificity for severe atherosclerosis in the ascending aorta and a cut-off value of 33 was with 74% sensitivity and 64% specificity.
Full table
Discussion
The main finding of this study is that severe atherosclerosis of the ascending aorta is more prevalent in patients with high SYNTAX scores. SYNTAX score was found to be an independent predictor of severe atherosclerosis in the ascending aorta and patients with high score of 33 or more have a 5 fold greater chance of severe atherosclerosis as compared to those with low scores of 22 or less. Notably, this association remained the case even after adjustment of other well documented predicting factors such as age, renal failure, and peripheral vascular disease, and history of stroke (9). Ikeda et al. showed a strong association between carotid disease and SYNTAX score (7). This result along with ours suggests the extent and complexity of CAD represented by SYNTAX score may be a good surrogate for the burden of systemic atherosclerosis. SYNTAX score seems to be less influential on the survival post CABG, contrary to PCI, where SYNTAX score is a prognostic parameter, however SYNTAX score may be useful as a tool to help modify the surgical approach. A high score may warrant more extensive and comprehensive assessment of the ascending aorta.
Stroke in PCI vs. CABG
In most contemporary randomized controlled trials (RCT) comparing CABG and PCI, the peri-procedural stroke rate in the CABG arm is higher than the PCI arm (1.3% vs. 0.24% in STNTAX trial and 1.8% vs. 0.3% in FREEDOM trial) (5,10). Although the absolute difference is about 1%, both differences are statistically significant. A recent comprehensive meta-analysis analyzing 19 historical RCTs with more than 10,000 patients also showed the similar finding of approximately 1% absolute increased risk of stroke in CABG (1.2% vs. 0.34%, OR =2.94) (11). Although by the 5-year follow-up in the SYNTAX trial, the higher stroke rate in CABG compared to PCI was attenuated and eventually got out of statistical significance (4), this immediate and higher, even if slightly by 1%, risk for stroke is indeed threatening for patients and is often a reason to decline CABG. It is thus described as “the Achilles heel of CABG” (12).
No room left for CABG?
It is unlikely PCI further reduces the periprocedural stroke rate from an already extremely low rate of less than 0.5% but there seems to be some room left for CABG. While there is no randomized data showing the benefit of off-pump approach in reducing stroke (13-15), a recent meta-analysis comparing on vs. off approach with about 9,000 patients showed a significant 30% reduction in stroke favoring off-pump approach (16). The recent consensus statement from the International Society for Minimally Invasive Cardiothoracic Surgery (ISMICS) also bears this out. When the off-pump approach is furthered with a no aortic touch technique a recent meta-analysis with more than 10,000 patients, showed an additional 70% reduction in stroke (17). These findings suggest that the less aortic manipulation, the less strokes, and add to the importance of assessment of the atherosclerosis of the aorta.
Atherosclerosis in the ascending aorta
Several risk factors for stroke have been found such as advanced age, female gender, history of stroke, diabetes mellitus, and hypertension (18). In recent years, atherosclerotic aortic disease has been recognized as an important risk factor (19,20). Unlike other risk factors, aortic atherosclerosis, especially in the ascending aorta, is directly related to aortic manipulation, which is a common part of CABG surgery. Identification of the severe atherosclerosis, either preoperatively or intraoperatively, and a tailored approach based on the findings may be important in reducing the risk of stroke after CABG.
Limitations of the study
This is a retrospective observational study and only deals with patients who underwent isolated CABG and the finding may not be generalized to other patient cohorts. The perioperative strategy modified by SYNTAX score was not adopted during the study period so the actual effect on the clinical outcomes needs to be further investigated. SYNTAX score II, recently introduced, includes clinical variables known to be associated with increased risk of aortic atherosclerosis (21) and may be a more precise predictor.
Conclusions
SYNTAX score was associated with the severity of atherosclerosis in the ascending aorta. Patients with a high SYNTAX score of 33 or more had an approximately 5-fold higher chance of severe atherosclerosis in the ascending aorta than those with low score of 22 or less. In current practice, SYNTAX score is widely available and should be utilized not only as a guide of decision-making in PCI vs. CABG but should also help the comprehensive assessment of the ascending aorta.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study protocol was approved by the Icahn School of Medicine at Mount Sinai Institutional Review Board (IRB#: 15-01013).
References
- Sianos G, Morel MA, Kappetein AP, et al. The SYNTAX Score: an angiographic tool grading the complexity of coronary artery disease. EuroIntervention 2005;1:219-27. [PubMed]
- Windecker S, Kolh P, Alfonso F, et al. 2014 ESC/EACTS Guidelines on myocardial revascularization: The Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS)Developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI). Eur Heart J 2014;35:2541-619. [Crossref] [PubMed]
- Amsterdam EA, Wenger NK, Brindis RG, et al. 2014 AHA/ACC Guideline for the Management of Patients with Non-ST-Elevation Acute Coronary Syndromes: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2014;64:e139-228. [Crossref] [PubMed]
- Mohr FW, Morice MC, Kappetein AP, et al. Coronary artery bypass graft surgery versus percutaneous coronary intervention in patients with three-vessel disease and left main coronary disease: 5-year follow-up of the randomised, clinical SYNTAX trial. Lancet 2013;381:629-38. [Crossref] [PubMed]
- Serruys PW, Morice MC, Kappetein AP, et al. Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. N Engl J Med 2009;360:961-72. [Crossref] [PubMed]
- Head SJ, Farooq V, Serruys PW, et al. The SYNTAX score and its clinical implications. Heart 2014;100:169-77. [Crossref] [PubMed]
- Ikeda N, Kogame N, Iijima R, et al. Carotid artery intima-media thickness and plaque score can predict the SYNTAX score. Eur Heart J 2012;33:113-9. [Crossref] [PubMed]
- Glas KE, Swaminathan M, Reeves ST, et al. Guidelines for the performance of a comprehensive intraoperative epiaortic ultrasonographic examination: recommendations of the American Society of Echocardiography and the Society of Cardiovascular Anesthesiologists; endorsed by the Society of Thoracic Surgeons. J Am Soc Echocardiogr 2007;20:1227-35. [Crossref] [PubMed]
- Schachner T, Nagele G, Kacani A, et al. Factors associated with presence of ascending aortic atherosclerosis in CABG patients. Ann Thorac Surg 2004;78:2028-32; discussion 32. [Crossref] [PubMed]
- Farkouh ME, Domanski M, Sleeper LA, et al. Strategies for multivessel revascularization in patients with diabetes. N Engl J Med 2012;367:2375-84. [Crossref] [PubMed]
- Palmerini T, Biondi-Zoccai G, Reggiani LB, et al. Risk of stroke with coronary artery bypass graft surgery compared with percutaneous coronary intervention. J Am Coll Cardiol 2012;60:798-805. [Crossref] [PubMed]
- Rastan AJ, Mohr FW. Three years after SYNTAX trial--change in practice? Eur J Cardiothorac Surg 2011;40:1279-81. [Crossref] [PubMed]
- Lamy A, Devereaux PJ, Prabhakaran D, et al. Off-pump or on-pump coronary-artery bypass grafting at 30 days. N Engl J Med 2012;366:1489-97. [Crossref] [PubMed]
- Shroyer AL, Grover FL, Hattler B, et al. On-pump versus off-pump coronary-artery bypass surgery. N Engl J Med 2009;361:1827-37. [Crossref] [PubMed]
- Puskas JD, Williams WH, Mahoney EM, et al. Off-pump vs conventional coronary artery bypass grafting: early and 1-year graft patency, cost, and quality-of-life outcomes: a randomized trial. JAMA 2004;291:1841-9. [Crossref] [PubMed]
- Afilalo J, Rasti M, Ohayon SM, et al. Off-pump vs. on-pump coronary artery bypass surgery: an updated meta-analysis and meta-regression of randomized trials. Eur Heart J 2012;33:1257-67. [Crossref] [PubMed]
- Misfeld M, Brereton RJ, Sweetman EA, et al. Neurologic complications after off-pump coronary artery bypass grafting with and without aortic manipulation: meta-analysis of 11,398 cases from 8 studies. J Thorac Cardiovasc Surg 2011;142:e11-7. [Crossref] [PubMed]
- Selim M. Perioperative stroke. N Engl J Med 2007;356:706-13. [Crossref] [PubMed]
- Filsoufi F, Rahmanian PB, Castillo JG, et al. Incidence, topography, predictors and long-term survival after stroke in patients undergoing coronary artery bypass grafting. Ann Thorac Surg 2008;85:862-70. [Crossref] [PubMed]
- van der Linden J, Hadjinikolaou L, Bergman P, et al. Postoperative stroke in cardiac surgery is related to the location and extent of atherosclerotic disease in the ascending aorta. J Am Coll Cardiol 2001;38:131-5. [Crossref] [PubMed]
- Farooq V, van Klaveren D, Steyerberg EW, et al. Anatomical and clinical characteristics to guide decision making between coronary artery bypass surgery and percutaneous coronary intervention for individual patients: development and validation of SYNTAX score II. Lancet 2013;381:639-50. [Crossref] [PubMed]


