Prof. Junling Li: the responsibility of a doctor
Introduction
The ancient Greek aphorism “know thyself” engraved on the forecourt of the Temple of Apollo epitomizes the human desire for the exploration into the unknown. In fact, never has mankind dragged their feet in understanding themselves, as in the achievements scientists have made all these years in the studies of disease and pathology.
Ere the 2017 WCLC journey, AME editors were sent across China to conduct in-depth interviews with an army of distinguished experts in the field of lung cancer. Together we learned how these soldiers fought for the nation that has the largest number of patients, and how they dedicated their lives to inventing the most-advanced weapons and probing into the enemy camp. From the past, they reflect and learn from mistakes; at present, they work hard and make changes; For the future, they make plans and improvements.
May this issue take you to the innermost world of these Chinese scholars, where you can delve into their wealth of knowledge and be inspired.
Expert’s introduction
Professor Junling Li, internal medicine MD, chief physician and PhD supervisor in Cancer Hospital Chinese Academy of Medical Sciences; deputy director of Cancer Hospital of Huanxing Chaoyang District Beijing; member of American Society of Clinical Oncology (ASCO); member of International Association for the Study of Lung Cancer (IASLC); deputy secretary general for Chinese Geriatric Oncology Society (CGOS); deputy chief for Lung Cancer Division in CGOS. His main specialties are chemotherapy and biological targeted therapy for malignant cancers and medical treatment for lung cancer. Professor Li has led and participated in multiple research projects and has published 23 articles as the first author or corresponding author, including 8 SCI articles, with a total IF of 20.684.
What occupation would you choose if you did not study medicine?
A teacher, I suppose, I was really interested in becoming a teacher and believed that I could be a good one, or maybe an engineer, because I like handicraft. When I was a boy, I was mischievous and often took apart stuff at home, such as my parents’ leather suitcase. I completed my university entrance exam in 1987. At that time, students were allowed to change their major after they had chosen one. My mother persuaded me to change my major to medicine because she believed that would be the best for me. I listened to her advice and started my study on medicine.
What would you like to do if you have a second chance to choose?
Being an animator probably, I was impressed when I took my daughter to visit Miyazaki Hayao’s studio, where boxes of pencil stubs were piled like hills. I have a patient who is an oil painter. He often goes to mountains and forests to create paintings. That is a good way to spend one’s life, I think, painting at his own will. It would be wonderful if everyone could live with such freedom.
Do you have any plans after retirement?
I yearn for a relaxing life. I particularly like the scene in the English movie Notting Hill, where the actress’s father was sitting on the sofa next to the fireplace, surrounded by many books. He was sipping his tea with a book in his hand. I also like an advertisement for a painkiller, which shows an old man fishing on a wooden wharf that extended to the centre of the lake. He sat on a board with his dog beside him. I would love to spend my retirement like that. A young doctor in my department heard my words and said, “stop dreaming, the lake will be crowded with people when you get to that age.” Ha-ha. Anyway, I would love to lead a meaningful life. Wherever I go, I always like making friends from all walks of life, chatting and drinking together. It is a pity that my physical condition does not allow me to drink too much.
From Alxa to Beijing
Prof. Li is a member of the Mongolian ethnic group. He was born in 1961 in a Sumu under Alxa Left Banner. Alxa League is at the most westerly area in Inner Mongolia Autonomous Region and is close to Gansu Province and Ningxia Autonomous Region. Sumu is a type of administrative district similar to a village, mostly distributed over pasturing area in Inner Mongolia Autonomous Region. According to Prof. Li, he grew up in the desert. Nevertheless, if not told, one may not associate his appearance with anything close to the classic image of a Mongolian warrior.
On the day of the interview, Prof. Li wore a pair of glasses with thin metal frame, well-ironed shirt, suit pants and a tie. As soon as he entered the appointed café, he stepped forward to shake hands with each of us. When we gave him our business cards, he would carefully read the information before putting them into the top left pocket on his shirt. He would lean in with enthusiasm when being asked about interview questions and would sit upright when talking enthusiastically about his interested topics. He spoke slowly with a soft voice, putting his listeners at ease. Looking back, the way Prof. Li talks and acts are gentlemanlike and quite different from the alleged image of a man from a nomadic area, although he emphasised multiple times that he does have some “nomadic” characteristics as well.
Prof. Li moved from his hometown to Ningxia Autonomous Region in 1978 and started his study in the Department of Medicine in Ningxia Medical University. After graduation, he worked in the Department of Internal Medicine in a local general hospital. At that time, he borrowed a book titled Cecil Textbook of Medicine. It was translated by Prof. Xiancai Wang, a famous medical translator who was selected as the Advanced Figure of the Year. The book contains twelve volumes in total and Oncology is in the eleventh volume, where the first line of the chapter still remains in Prof. Li’s mind, “In order to become a good medical oncologist, one needs to be good at general practice first.”
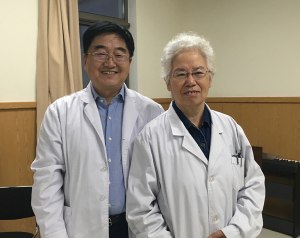
Coincidently, the director of the department intended to guide Prof. Li to focus on the field of Oncology at that time. And that was how Prof. Li started his work in medical oncology. In 1993, Prof. Li got a chance to study as a visiting scholar in Cancer Hospital Chinese Academy of Medical Sciences. As soon as he arrived there, he liked it and thought that it was the perfect place for him. So, after one year of study, Prof. Li tried to stay there with the support from his mentor Prof. Datong Chu and postgraduate supervisor Prof. Xiangru Zhang (Figure 1). He then followed Prof. Chu to study biotherapy and chemoimmunotherapy for cancers. He was one of the few physicians who managed to stay in the Cancer Hospital in that year. As both his mentor and supervisor are outstanding experts in the field of lung cancer, Prof. Li naturally started to focus on this area as well, mainly working on medical treatment and targeted therapy for lung cancer.
Prof. Li relocated himself from a desert area in Inner Mongolia to Ningxia, then to Beijing. He also upgraded himself academically from a bachelor degree in an ordinary provincial medical university to a master degree in one of the top medical schools in mainland China, Peking Union Medical College. He then completed his doctoral degree in clinical medicine there as well. He gradually figured out his focused research area, starting from internal medicine to medical oncology, and then to medical oncology for lung cancer. With efforts, Prof. Li completed a journey with multiple great leaps.
From 5:15 am to 12:00 am
A quarter past five the immovable time at which Prof. Li wakes up every morning. After getting up, he would turn on the computer and log into an online platform where he checks messages left by his patients. When he arrives at the hospital, he would like to stay in his car for a little while, either contemplating in silence or listen to jazz music for a few moments. He enjoys spending some time in solitude like this.
Prof. Li’s fondness of jazz music can be dated back to 2004 when he attended the 40th Annual Meeting of American Society of Clinical Oncology (ASCO) in New Orleans, USA. He fell in love with jazz music at its birthplace. “Previously, I did not like jazz music because it sounds a bit disorderly to me but now whenever I listen to jazz, I feel peaceful.”
At 7 am every Monday, Prof. Li starts his outpatient clinic with 2 cups of his favourite Starbucks coffee. When it gets to 1:30 pm, he will move to another office to do the VIP outpatient clinic and continues that till 5:30 pm. Then he will have the daily meeting with his postgraduate students, lasting for about 1 hour. He normally finishes work when it is close to 7 pm, but when he gets home he can only have a brief break. Then he needs to start his next task—case management outside the hospital. He needs to reply patients’ messages on the online platform and deal with consultation phone calls. He normally needs to answer 20 to 30 patients’ messages and only can manage to officially finish work between 11 pm to 12 am.
By the time we met Prof. Li at our appointed time, 2:30 pm on a Tuesday, he had already seen 35 patients with appointments plus 12 walk-in patients. He had only 10 minutes for lunch. However, Prof. Li said he had long been used to such workload.
Prof. Li does not do outpatient clinic on Wednesday and Thursday, but he needs to do ward rounds in two inpatient areas. On Friday, he needs to attend the morning meeting in hospital. He has five doctoral students and two master students now and is responsible for supervising them and guiding them to work on their research projects. He also needs to spare some time to do clinical research and often needs to attend academic meetings on weekend (Figure 2).
When talking about such heavy workload, Prof. Li frankly said, “I feel exhausted.” Nowadays, patients often find doctors unapproachable, expressionless, and impatient, but doctors have their own frustration. Prof. Li said, “Imagine that one has to talk from morning to night and the conversation gradually drains him. I used to be like that too. At the end of a day, it felt like that my will can no longer control my physical conditions, and I cannot help but feel irritated and agitated.”
From 5 to 30 minutes
The mode of outpatient treatment is the one that Prof. Li has been wanting to implement. “My ideal outpatient treatment mode is where a patient books an appointment with the physician, such as from 10 am to 10:30 am. During the half an hour, doctors and patients can communicate adequately. Then, the patient can just go home.” Under such a mode, patients can retain as much of their normal life as possible and minimize the amount of disturbance their disease may bring to their lives.
However, in order to make this ideal a reality, there are many obstacles to overcome. China is a country with a large population, and by extension, a large number of patients in hospitals as well. Prof. Li attended an online medical forum organized by Health and Family Planning Commission and Health News not long ago. Jianfeng Bai from People’s Daily raised the issue, saying “The average time American doctors spend with a patient is 30 to 45 minutes and the time for the follow-up interview is about half an hour, while Chinese doctors only spend about 5 minutes to see a patient. These numbers are even lower with doctors from India, who spend an average of 2 minutes for a patient.”
That is also one of the reasons why China cannot implement outpatient clinic at a large scale at the moment. “How can we possibly achieve shared doctor-patient shared decision making, which is to have in-depth communication with patients, to make them understand what we’re saying and make a decision after consideration, in such a short period of time?”
Despite the reality, Prof. Li insists on providing consultation for his patients for 10 minutes on average, and for some patients, half an hour or more. He also has a special habit of persisting in organizing patients’ case reports and would not simply copy and paste the information. Once, he organized a patient’s case report for a whole 40 minutes, and the patient was moved by his endeavour.
“The follow-up treatment plan for a cancer patient must be based on his/her previous treatment plan, and preferably not to repeat the plan the patient has already undergone.” Prof. Li inherited this habit from his mentor Prof. Xiangru Zhang.
Prof. Li really hoped patients or their family to organize their medical records before coming to the hospital, so as to save more time to talk about treatment plans with the patient. In order to help patients, Prof. Li wrote an article to guide patients on what to prepare before coming to the hospital.
“It is not easy to find an available appointment timeslot and it will cost a patient ¥500 a time if the patient would like to have a VIP outpatient clinic from me. If the patient does not bring adequate documents, it would be a waste of money and effort. For instance, a patient only brought his most recent scan result, but didn’t bring the one taken previously. Without comparison of the two, I couldn’t tell if the treatment was effective and could not guide the patient in their next step of treatment. Therefore, I ask my patient to not only bring the current scan report but also previous ones to provide complete information.”
From shaking hands to drawing “fishbone diagram”
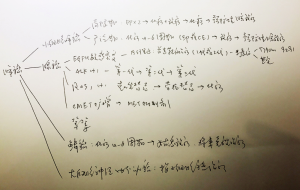
Every time Prof. Li welcomes a patient, he will take the initiative to shake hands. For him, handshaking is an expression of respect for the patient and the beginning of equal communication. Whenever he communicates with patients, he will try to explain their conditions in the simplest words and in the most concise way. He will also take a piece of paper and draw a “fishbone diagram” for the patient to explain. “This is lung cancer. It can be divided into small cell lung cancer and non-small cell lung cancer. Non-small cell lung cancer can be divided into adenocarcinoma, squamous cell carcinoma, and large cell lung carcinoma. Adenocarcinoma can be divided into EGRF mutation, ALK positive etc. EGRF mutation, again, can be divided into EGRF 19 mutation and EGRF 21 mutation. And then I explain how we treat this particular condition, and this other condition, so patients will have a clear understanding.” Prof. Li may draw such “fishbone diagrams” for a couple of times during a day for patients (Figure 3).
“I need to explain a lot of things every day. One time, a patient came to ask me why the scanning of the nodules looked a bit different from that taken last time. He was referring to a nodule of 3 to 4 mm. I explained to him that the way CT scanning works is like when we cut potato or winter melon into slices. The rays in CT scanning can provide slices of 5 mm. This focus of infection is only 3–4 mm, thus it could be detected during one scan and not in the next.” Prof. Li continued, “There are also a number of patients that become worried when the scanning shows multiple nodules. However, the imaging department thinks it is not enough to decide the nature of the nodules. In such cases, I need to explain to the patient that he does not need to worry too much or be too scared, and that we just need to carry out regular tests.”
Despite the fact that there is still a long way to go in achieving his ideal treatment mode, Prof. Li has managed to shorten the distance between him and his patients and try to communicate with patients as well as possible. Even sometimes, when he gets home tired late at night, and reads some patients’ messages expressing anger or provocation, he would choose to put himself in the patient’s shoes and try to understand their uncontrollable emotions caused by the disease and obstacles in life.
With regard to his own emotions, Prof. Li chooses a quiet and peaceful way to deal with them.
From humanistic medicine to One Piece
In his spare time, Prof. Li likes to read books, mainly books on humanistic medicine or biographies. He has read the biographies of Steve Jobs and Howard D. Schultz. For Prof. Li, reading biographies always helps him find some resonance in other people’s stories.
“I am almost 60 years old, but there are still many books and movies that I have yet to read and watch.” Prof. Li likes movies, but as opposed to literary films and classic black-and-white films, Prof. Li enjoys the time he spends watching movies with his children the most.
He has watched with his children all of Miyazaki Hayao’s animes, the entire series of Harry Potter, “and then she began to watch One Piece, which I couldn’t enjoy any more. Nevertheless, Prof. Li, who can blurt out the English name of One Piece, must know about it to some extent.
Prof. Li enjoys being alone and also enjoys the company of his family, which silently dissolves all his negative energy, allowing him to reclaim his energy, move on, and bring new hope for more patients.
Prof. Li once posted a few lines from Better: A Surgeon’s Notes on Performance by Atul Gawande on his social media platform, “The world is chaotic, disorganized, and vexing, and medicine is nowhere spared that reality. To complicate matters, we in medicine are also only humans ourselves. We are distractible, weak, and given to our own concerns. Yet still, to live as a doctor is to live so that one’s life is bound up in others’ and in science and in the messy, complicated connection between the two. It is to live a life of responsibility. The question, then, is not whether one accepts the responsibility. Just by doing this work, one has. The question is, having accepted the responsibility, how one does such work well.”
To answer this question, Prof. Li has provided a perfect answer with his own experience (Figure 4).
Conversation with Prof. Junling Li
AME: When it comes to communication with patients, are there any differences between general outpatient clinic and outpatient clinic for patients with cancers/lung cancers?
Prof. Li: I mainly look at lung cancer, so almost all of my patients are lung cancer patients. They have been clearly diagnosed before they see me. A patient may come for subsequent adjuvant therapy after the surgery, may come for induction therapy before surgery, may come because s/he has had recurrence or metastasis, or may come for systemic treatment for advanced stage lung cancer. Most of them are aware of their illness and are mentally prepared for it.
AME: Some patients’ family members will ask the doctor to hide the patient’s actual conditions. What do you think about that?
Prof. Li: I would encourage family members to tell the truth to the patients. Some family members are always making up stories. Although it is a white lie, it is a tiring process, and at some point, they realise that they can no longer make up stories and would ask me to join them in lying to the patient. I cannot lie to the patient and say, “it is only a nodule and it is benign.” And I find that most of the patients are aware of the truth at the bottom of their heart. It is just a tacit agreement between the patients and their families, neither party would speak out the truth.
AME: How do you communicate with your patients?
Prof. Li: I think doctors need to be empathetic so that they can truly feel their patients. I remember one time when I attended an Annual Meeting of ASCO, there was a half-day special session. All participants were oncologists who were also cancer patients themselves. They shared their feelings, which left a deep impression on me. After that I started to pay special attention to equal communication with patients, by maintaining eye contact and listening to them properly. I would tell them about their conditions and the next step of treatment in detail. I would give them enough time to consider. All of these cannot be completed within the short period during outpatient clinic. So, I pay special attention to case management outside the hospital, letting the patients leave me messages on the Internet, and I write back to them.
AME: Medicine is a very special profession; are there any differences you’ve observed when doctors face cancer, as opposed to people from other professions?
Prof. Li: I have noticed a phenomenon that if medical professionals, especially those from our department, are diagnosed with cancer, they normally have long life expectancy. It may be because they are so familiar with the disease and will actively cooperate with treatment plans. When talking about the diseases, they are also relatively open-minded.
In 1990s, Prof. Zongyi Yang, a famous physician from the department of radiotherapy for thoracic cancers in our hospital, was diagnosed with lung cancer. He analyzed his conditions and imaging data with us and predicted how long he could live. It was like he was not talking about himself, but about someone else. He was just too familiar with this disease.
AME: Will you tell your patients their estimated life expectancy?
Prof. Li: I will let them know two numbers. One is the median. For example, I will tell a patient that according to the clinical data, 50% of the patients with your conditions survived for 4 years, but I cannot tell you about your exact years of survival. The other number I will tell the patient is the maximum we have recorded, for instance, a patient who survived for 10 years with the same conditions as the patient, so as to encourage him/her.
AME: How do you think of the saying “lung cancer is an incurable disease”?
Prof. Li: It depends on the concept of “cured”. In the 1990s, NSCLC was not treated because there was no effective treatment method. Later, therapies including cisplatin was introduced, and then, Gemzar, Navelbine, docetaxel, paclitaxel helped to increase patients’ median survival time to about 10 months. After ECOG-E4599, a combination therapy of paclitaxel and TC, the survival time of NSCLC patients was increased to more than one year for the first time. Nowadays, TKI medications are available. Medicines like iressa, erlotinib, icotinib, multi-target tyrosine kinase inhibitors, pemetrexed could help patients to increase the median survival time to more than 3 and a half years. Patients with ALK-positive lung cancer could survive for more than four years with appropriate treatment. Although lung cancer is still incurable, we have been improving to control the disease. In the future, if most patients diagnosed with lung cancer can survive for 10 years, there would be less fear towards this disease.
AME: Just now you mentioned “controlling the disease”, can you share this idea with us?
Prof. Li: A lot of patients do not get nervous when having fluctuations on blood pressure or blood sugar, however, they have zero tolerance towards the volatility of tumor markers, as if the goal of treatment is to make sure the number of tumor markers does not rise. Therefore, they would like to pay a lot to and try various treatment methods to achieve this goal. As a result, we try to introduce the concept that lung cancer is a kind of chronic disease that can be controlled, not cured. Controlling disease means allowing the number of tumor markers to fluctuate within a certain range, so long as the image is stable and the quality of life of the patients is not affected, the patient should not worry too much.
AME: When the survival time for patients with advanced lung cancer is extended, how do we improve their quality of life?
Prof. Li: Patients with advanced lung cancer normally spend their life with constant treatment, which requires clinical physicians to simplify the treatment, reduce side effects, and minimize the interference to patients’ normal life as much as possible. This is quite demanding and is exactly what we are striving for. With the application of targeted drugs, highly effective low-toxicity drugs and antiangiogenic drugs, we can meet the above requirements in some patients, but there is still a lot to be worked on.
AME: How do you communicate with patients who are having palliative care?
Prof. Li: It is really hard, especially in China. A medical humanities lecturer once said that the Chinese are unprepared for death because we have no religious beliefs. Patients hope to live as long as possible, even at the end of their lives, they still hope for miracles. But now things are starting to get better thanks to advances in the treatment of lung cancer. Patients tend to be more unperturbed when facing death after years of treatment. They will also express their long-term wish and do not want to suffer too much. Then, I will try to control their symptoms, take out pericardial effusion when needed, and find specialist in pain treatment or nutritionists to help them as well.
AME: You gave a lecture on the topic titled “Why do different doctors have different treatment plans for patients?” before. Can you tell us why you choose this topic?
Prof. Li: There was a book titled Debate on Therapeutics, which tells us that there are different treatments for the same disease. Take the flu for instance, some may say patients need to take medications, some may say they only need to drink hot water, some may say to keep warm, and some may say to just eat boiled mutton. Different as they are, they all have their reasons. Take treatment to TB for instance, there are long-range and short-range treatment plans. With strong basis on evidence-based medicine, patients may receive radiotherapy plans for either a month or two weeks. It tells us that there are many treatments plans available, which is something good. I think it is ok to accept these differences and one can speak out his own reasons to provide a plan, as long as it is ethical and consistent with the guidelines. Medical professionals with different specialties should not go against each other. Different backgrounds may lead to different treatment theories and the way to understand the disease. I think different theories can coexist as long as it is good for the patient.
AME: We know that TKI resistance is bound to happen. How do you communicate with patients about this problem?
Prof Li: Before using TKI treatment plan, we need to tell patients that drug resistance is bound to happen, where 50% of patients may experience resistance for about one year. This will help patients be mentally ready for it. Then we need to tell patients what the next step of treatment after their drug resistance occurs will be. After a period of time, they won’t be so afraid of drug resistance. A peaceful mind can also improve the patient’s life.
AME: What will you normally do after TKI resistance occurs?
Prof. Li: The way drug resistance develops can vary. In most treatments involving TKI, the drug resistance develops gradually, characterized with slow rise in tumor markers, slight satiation in focus of infection, gradual growth in the size of the focus of infection, or the overall control may be quite good, but intracranial or adrenal metastasis has occurred.
I like fixing things. For instance, once my daughter wore out her trousers, I fixed it with a sew-on patch of a rabbit. When it comes to cancer treatment, I think it is the same thing. I am trying to patch up treatment plans as long as we can make sure the disease does not advance rapidly. We try to make the curative effect last for a while. If the intracranial metastasis or focus of infection grows larger, the patient should be advised to do a partial radiotherapy. Until it does not work anymore, then we will adjust the plan before the patient’s condition deteriorates. I will try to discuss different treatment plans with patients in a heart-to-heart manner and let them consider and decide.
AME: You often suggest to your patients to not purposefully avoid the use of painkillers. Why is that?
Prof. Li: Pain is intolerable and for a lung cancer patient, the pain is endless. It affects a patient’s sleep. If one cannot sleep well, his body cannot get good rest and he will become anxious and irritated. His physical conditions will also deteriorate, which is bad for his treatment.
AME: Many patients are worried about becoming addicted to painkillers, what is your opinion on that?
Prof. Li: Painkillers are different from drugs, which brings euphoric feelings to people due to its high increase in plasma concentration in a sudden. While a patient takes pain killer, his plasma concentration gradually increases to a stable level to control the pain and is not easily addictive. When the disease is under control and there is no longer any pain, the patient does not need to continue to take painkillers. In addition, the side effects of pain killers, such as constipation, nausea, headache may also deter patients from taking them. Therefore, the dosage will be controlled when pain reduction is maximized while avoiding side effects.
AME: You mentioned in the previous report that the goals of regulating treatment are to cure cancer, improve the quality of life and prolong survival. Why did you choose these three goals?
Prof. Li: Some patients are afraid of the side effects from treatment and refuse to undergo surgery or chemoradiotherapy. They would choose some folk prescription, or find some alternative treatment, or undergo some untraditional treatment methods. These are not standard treatment methods.
In what we call a standard treatment, if the patient has early-stage lung cancer, he would be advised to undergo partial treatment, surgery or local radiotherapy. There is a chance to cure the cancer. If the cancer is not curable, we will help patients to improve the quality of life so that he can do what he wants to for the rest of his life. We will carry out treatment for him according to evidence-based medicine. In different stages of the cancer, we try to provide effective treatment, improve his quality of life, which will naturally prolong the patient’s life expectancy. I believe they are complementary.
AME: How is immunotherapy for lung cancer progressing?
Prof. Li: Nowadays, we are trying immunotherapy for almost all types of cancers. Some patients do benefit from it. In terms of lung cancer, about 30% of them benefit from it. At present, immunotherapy works relatively well in patients with high PD-L1 expression, high TMB, or smoking history.
AME: Would you often advise patients to adhere to immunotherapy when conditions permit?
Prof. Li: At present, for most patients, immunotherapy is way too expensive. For instance, using Keytruda for 10 months will cost about ¥920,000, which is not affordable for an average person. Therefore, we have to consider a patient’s financial capacity. I do not want to see a patient sell his house and lose all his property and risk his family for treatment. One should try his best within limits.
AME: What do you think is currently the biggest problem when facing immunotherapy?
Prof Li: The difficulty is to find out who is suitable for immunotherapy and who is not. For instance, now we exclude immunotherapy for patients with EGFR sensitive mutation and positive ALK. There may be a solution in the future but immunotherapy is currently ineffective or counterproductive for such patients.
AME: You still have a ward in Huanxing hospital. Can you tell us something about it?
Prof. Li: The team over there is relatively young, and the patients are quite sick. Therefore, we pay more attention to the humanistic care to these patients. I have tried to advocate improving patients’ medical experience over there, which is to make patients have a more comfortable medical environment, make them feel like they’re being cared, provide appropriate treatment methods, provide good doctor-patient communication so that patients can trust doctors.
In addition, I have tried to improve the medical environment. For instance, to deodorize the smell in the toilets, we adopted some deodorization methods and provide hand sanitizer and toilet paper. The landscape outside the ward window was also slightly altered, because for many patients, all they could see was the little view looking from the ward window.
Once there was a guy whose father was our patient. Every day he came to visit his father, he would bring many pictures and the record of the traffic flow outside the hospital for his father. I was especially moved. For some people, they cannot go wherever they would like to go. For patients with advanced cancer and patients undergoing palliative care, we need to show empathy to their inner needs. That is why we have tried to improve in those aspects.
AME: You have also done a lot of jobs to popularize medical science in the public. Why would you want to do this?
Prof. Li: The best treatment for a disease is to prevent it. If our nation can ban smoking, the incidence of lung cancer will definitely drop dramatically. However, people do not pay much attention to health issues. So, I believe that regardless if they are patients, their family members or doctors, we all need to learn about medical science. Even if I turn myself into a machine to see patients continuously, there are still limitations. What pains me is that nowadays, more and more young people have developed lung cancers. Some of them are at their peak, who are the backbone of their families and the core members of their workplaces.
Acknowledgements
The editor would like to thank Bella Poon for proofreading this article.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
(Editors: Siying Yan, Vivian Kong, AME Publishing Company,