Successful repair of thoracic outlet syndrome in a growing young patient due to posterior sternoclavicular joint dislocation
Introduction
Posterior sternoclavicular dislocation is an extremely rare injury, usually related to heavy trauma, such as a traffic accident (1,2). The anatomical proximity of vital mediastinal structures can complicate closed reduction, especially during emergency situations (1,3,4). We present a rare case, in which an emergent open reduction using both sutures reduction and simultaneous plate stabilization of a posterior sternoclavicular dislocation was performed for thoracic outlet syndrome due to compression of great vessels and nerves.
Case presentation
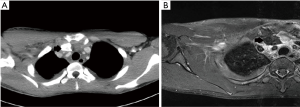
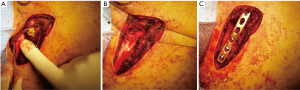
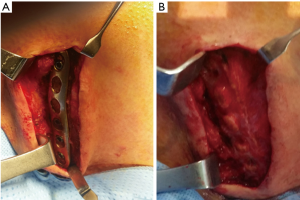
A 17-year-old Korean man visited our hospital emergency department after heavy trauma to the right shoulder and chest. He had fallen down a flight of stairs five days previously. He had progressive severe pain at the right sternoclavicular joint and shoulder, limited motion in the right shoulder (especially, abduction of the right arm), swelling in the right forearm, a tingling sensation in the right hand, and unable to grip. Both radial and ulnar arteries pulse were found. Chest computed tomography (CT) and shoulder magnetic resonance imaging (MRI) showed a posterior dislocation of the right clavicular head with rupture of all sternoclavicular joint ligaments; a hematoma around the clavicular shaft; compression of the right brachiocephalic, subclavian, and internal jugular veins; compression of the brachial plexus; and a right hemopneumothorax (Figure 1A,B). He was diagnosed with thoracic outlet syndrome due to posterior sternoclavicular dislocation. Due to suspicious neurovascular injuries, an emergent open reduction was conducted for posterior sternoclavicular dislocation under general anesthesia. The surgical approach was performed from the right mid-clavicle to the upper portion of the sternal body in order to allow for direct visualization of potential vascular complications. The operative findings showed posterior sternoclavicular dislocation with complete rupture of the sternoclavicular joint capsule, ligaments, and tendons, and hematoma around the clavicle shaft and head. However, there was no active bleeding or definitive vascular injury and no definitive fracture in the sternum or clavicle (Figure 2A). In order to avoid a substernal dissection and injuries to the mediastinal structures, two oblique holes were made using a 3.2-mm drill at the manubrium and medial end of the clavicle 1 cm from the joint. Two Ethibond EXCEL® Polyester 2-0 sutures passed through these holes, and the joint was reduced with knots (Figure 2B). Cartilage, joint capsule, and tendons could not be repaired because of complete and irregular rupture. Because there was no other structure available to stabilize the precarious joint, we added internal stabilization using unicortical locking plate osteosynthesis (Synthes, 3.5 mm) (Figure 2C). The patient’s postoperative course was uneventful without any complications. The patient’s symptoms were greatly improved immediately after the surgery and were completely resolved by the seventh postoperative day. His shoulder was immobilized with an arm sling for two weeks. He resumed almost full weight bearing four weeks after the surgery. After six months, the plate was removed (Figure 3A,B), and the patient continued to have full weight bearing ability without any motion restrictions.
Discussion
Dislocation of the sternoclavicular joint is very rare and is never seen by many surgeons, especially the posterior subtype (2-4). However, because of the anatomical proximity of the structures in superior mediastinum and thoracic outlet, including the great vessels, esophagus, trachea and lungs, and brachial plexus, posterior sternoclavicular dislocations are potentially fatal (1,3,4). Systematic and swift evaluation is mandatory for proper management of these patients (3).
The sternoclavicular joint is comprised of strong structures (intra-articular disk and costoclavicular, capsular, and interclavicular ligaments and tendons), which yield substantial strength that can endure intense forces toward the joint, and thus experiences a low incidence of dislocation (2-4). Therefore, tremendous force is required for sternoclavicular dislocation, and posterior dislocation is rarer than anterior dislocation. Patients with posterior sternoclavicular dislocation usually present with intense pain, short of breath or dyspnea, dysphagia, or thoracic outlet syndrome (due to decreased circulation to the ipsilateral extremity or venous congestion in the extremity or neck and compression of the brachial plexus) (2,3). Chest CT is essential for evaluation of the sternoclavicular joint because it is difficult to evaluate the sternoclavicular joint by simple radiographic studies due to superposition of the medial clavicle, ribs, sternum, and vertebrae, and indiscrimination among sprains, dislocations, and medial clavicular fractures (3,4). In addition, chest CT should be performed to ascertain any injury to the vital structures surrounding the sternoclavicular joint (3). Occasionally, MRI should also be conducted to evaluate the integrity of the sternoclavicular joint soft tissue (ligament, tendon, and capsule) and the neurovascular bundle in thoracic outlet and mediastinum (2,3). Due to the high risk of injury to mediastinal structures, a closed reduction should be attempted as soon as possible, as open reductions are usually not required for posterior sternoclavicular dislocation (2,3). However, in this case report, because chest CT revealed suspicious vascular injuries, an emergent open reduction was chosen. MRI was also performed to evaluate the integrity of the sternoclavicular joint soft tissue and showed that the joint soft tissue was completely and irregularly ruptured. Therefore, repair of the soft tissue appeared unfeasible.
Primary repair of the ligamentous structures for stabilization is usually not feasible, especially after reduction, and there is no definitive consensus on an optimal method of repair (1,2,4-6). Soft stabilization procedures involving repair of surrounding ligaments and reconstruction with fascia, muscle tendon, or carbon fiber, and by resection of the clavicular head require long-term postoperative immobilization and retrosternal dissection (3,4). Therefore, plate stabilization of the sternoclavicular joint seems more attractive as it avoids retrosternal dissection and reduces the postoperative immobilization period (1,4,5). However, some studies have suggested that plate stabilization should be avoided due to serious complications arising from the use of metal materials, such as migration or fractures (1,3). In this case study, because soft tissue in the joint was completely and irregularly ruptured and repair of the soft tissue did not appear feasible, we reduced the joint with two sutures through oblique holes drilled at the manubrium and the medial end of the clavicle. These drill holes were made obliquely in order to avoid substernal dissection and injuries to mediastinal structures (4). However, additional stabilization using a locking plate osteosynthesis was also conducted because the reduction using only sutures did not result in complete stability. The most important factors for open reduction are method of and sufficient duration for stabilization. In our case, reduction was conducted with only sutures without repair of the soft tissue, and insufficient for proper stability (4,5). Therefore, additional stabilization using a locking plate osteosynthesis was completed, which also reduced the immobilization period. However, body growth should be considered in a growing young patient (1,2), and the plate should be removed after stabilization. In our case, we removed the plate six months after the open reduction surgery (4). If we performed the open reduction only using sutures, joint stability would not have been obtained postoperatively and prolonged immobilization would have been required. Conversely, if we performed the open reduction using only a locking plate, stability of the joint would also have been suspicious after removal of the plate, and complications due to prolonged use of metal materials might have arisen, especially in this growing young patient. The combined technique described in this case report is a feasible and promising method to secure enough time for permanent stabilization for posterior sternoclavicular dislocation repairs
Conclusions
Posterior dislocation of the sternoclavicular joint is an extremely rare injury, but can be fatal. Systematic and swift evaluation is mandatory for posterior sternoclavicular dislocation. This technique, using both sutures reduction and simultaneous plate stabilization, will offer excellent results, especially in a growing, young patient.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This case study was approved by Institutional Review Board for Uijeongbu St. Mary’s Hospital (IRB number: UC16ZISE0010) and written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Tepolt F, Carry PM, Taylor M, et al. Posterior sternoclavicular joint injuries in skeletally immature patients. Orthopedics 2014;37:e174-81. [Crossref] [PubMed]
- Chaudhry S. Pediatric posterior sternoclavicular joint injuries. J Am Acad Orthop Surg 2015;23:468-75. [Crossref] [PubMed]
- Groh GI, Wirth MA. Management of traumatic sternoclavicular joint injuries. J Am Acad Orthop Surg 2011;19:1-7. [Crossref] [PubMed]
- Stahel PF, Barlow B, Tepolt F, et al. Safe surgical technique: reconstruction of the sternoclavicular joint for posttraumatic arthritis after posterior sternoclavicular dislocation. Patient Saf Surg 2013;7:38. [Crossref] [PubMed]
- Quispe JC, Herbert B, Chadayammuri VP, et al. Transarticular plating for acute posterior sternoclavicular joint dislocations: a valid treatment option? Int Orthop 2016;40:1503-8. [Crossref] [PubMed]
- Wiesler ER, Chloros GD, Xu NM, et al. A rare cause of thoracic outlet syndrome. Arch Orthop Trauma Surg 2008;128:33-5. [Crossref] [PubMed]


