Moderate aortic valve stenosis in patients with left ventricular systolic dysfunction—insights on prognosis and the potential role of early aortic valve replacement
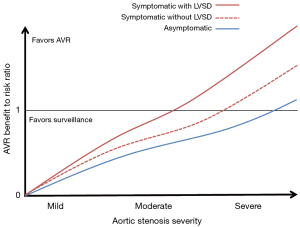
Aortic valve replacement (AVR) is the only definitive therapy for patients with hemodynamically significant aortic stenosis (AS), and the most pivotal issue in the longitudinal management of patients with AS is to identify the optimal timing for AVR when the benefits of the procedure most outweigh the risks. In 1968, Ross and Braunwald famously described the grim prognosis associated with the onset of symptoms in patients with AS (1), and since that seminal publication the favored approach has largely centered on proceeding with AVR at the onset of symptoms in those with severe AS. The benefit of AVR in patients with asymptomatic severe AS is less well established, and exercise testing has gained a meaningful role in guiding the decision on AVR in these patients (2,3). However, in asymptomatic patients with normal left ventricular ejection fraction (LVEF), AVR carries only a class II indication in the most recent American and European society guidelines highlighting the remaining uncertainty about timing of intervention in this group (4,5). Moreover, in patients with AS which is not considered severe by echocardiographic or invasive assessment, there has generally been no indication for AVR unless performed concomitantly with another open-heart operation. Conventional wisdom has suggested that patients with non-severe AS [aortic valve area or (AVA) >1.0 cm2] do not have hemodynamically significant valvular obstruction to cause symptoms or other functional impairment, and that AVR in patients without hemodynamically important obstruction would carry unwarranted risk without anticipated benefit (Figure 1).
However, in recent years the concept that moderate severity AS in patients with concomitant left ventricular systolic dysfunction (LVSD) may confer a significant risk of cardiovascular events has garnered considerable attention. In a recent study by Van Gils et al. in the Journal of the American College of Cardiology earlier this year, the authors report the clinical outcomes of a retrospective multicenter registry of 305 patients with LVSD (LVEF <50%) and moderate AS (AVA, 1.0–1.5 cm2 by echocardiographic continuity equation calculation) (6). The majority of patients were symptomatic [New York Heart Association (NYHA) class 2 in 42%, class 3 in 28%, and class 4 in 4%] although baseline use of heart failure medications was somewhat heterogeneous with only 13% taking optimal medical therapy with combined beta-blocker, angiotensin system antagonist, and mineralocorticoid receptor antagonist. The primary composite endpoint of death, AVR, or hospitalization for heart failure occurred in 24% at 1 year, 38% at 2 years, 47% at 3 years, and 61% at 4 years follow-up. When considering death alone, the risk remained substantial with a mortality rate of 9%, 18%, 25%, and 36% at 1, 2, 3, and 4 years, respectively. In multivariate Cox regression analysis, the authors identified male sex, NYHA class 3 or 4 symptoms, and peak aortic jet velocity as independent predictors of the primary composite endpoint.
These findings challenge the conventional wisdom of >50 years that moderate AS is not associated with untoward hemodynamic consequence and increased cardiovascular event rates and thus does not warrant AVR. The natural history of moderate AS in prior reports has been somewhat heterogenous across various populations, reflecting the importance of comorbid cardiovascular and non-cardiovascular disease in these patients. A historical series from the Mayo Clinic of 61 patients with moderate severity AS and preserved LVEF by cardiac catheterization reported a 59% rate of complication free survival in over 4-year follow-up (7). A more recent European series of 176 patients with mild-moderate AS reported 60% survival free of AVR at 5 years (8). van Gils et al. report a much lower rate of 41% event-free survival at 4-year follow-up among patients with moderate AS and LVSD (6). These findings confirm those of another recent series from the VA population in which 5-year event-free survival in 104 veterans with moderate AS was only 15% (9). Although it is difficult to compare event rates directly across studies due to important differences in study populations and end-point composites, the overall message is clear—moderate AS cannot be considered a benign entity due to very high rates of cardiovascular events over 3–5-year follow-up. The data by van Gils et al. further contribute to this understanding by highlighting the interaction between aortic valve stenosis and ventricular function.
Afterload reduction has been a long-standing cornerstone of heart failure medical therapy for patients with LVSD, with multiple large randomized controlled trials demonstrating a survival advantage in heart failure patients treated with afterload reducing agents (10-12). Moreover, data from our institution has previously demonstrated that aggressive afterload reduction with intravenous sodium nitroprusside improves hemodynamics parameters in critically ill patients with concomitant severe AS and LVSD (13). In context of AS, a substantial body of literature has focused on quantifying afterload as valvulo-arterial impedance (Zva) (systolic blood pressure + mean transaortic gradient/stroke volume index), a metric which incorporates both systemic arterial compliance and valvular impedance to characterize global left ventricular (LV) afterload (14-17). In a prospective cohort of 173 asymptomatic patients with severe AS and normal LV systolic function, Lancellotti et al. characterize the relationship between LV afterload and LV systolic performance in AS patients, demonstrating that increased Zva was associated with reduced LV systolic performance in terms of LV myocardial deformation by strain imaging (18). While vasodilator heart failure therapies have historically targeted the component of afterload contributed by systemic arterial compliance, the contribution of AS to ventricular afterload in patients with heart failure has been less well described. The data reported by van Gils et al. suggest that the even moderate AS contributes a significant burden of afterload on the left ventricle resulting in rates of major adverse coronary events (MACE) out of proportion to that expected based on the degree of LVSD alone.
Reducing global LV afterload with AVR may offer an opportunity to improve LV systolic function and clinical outcomes in patients with concomitant AS and LVSD, but the ideal strategy to manage patients with concomitant non-severe AS and LVSD remains uncertain. In a recent retrospective cohort from the Duke University Echo Database, Samad et al. reported that among 1,090 patients with moderate AS and LVSD, AVR (n=287) was associated with a 41% reduction in survival over a median follow-up of 1.2 years (hazard ratio, 0.59; 95% confidence interval, 0.44–0.78) (19). The observational methods of that study limit the ability to draw definitive conclusions about the benefits of AVR in patients with moderate AS and LVSD. However, taken together, the data from Samad et al. and van Gils et al. serve as prelude to the anticipated transcatheter aortic valve replacement (TAVR) UNLOAD trial which is a multicenter trial randomizing 600 patients with moderate AS and LVSD to TAVR with the 3rd generation SAPIEN 3 transcatheter heart valve vs. optimal medical therapy with a hierarchical primary outcome of death, disabling stroke, heart failure hospitalization, symptomatic aortic valve disease, non-disabling stroke, and change in Kansas City Cardiomyopathy Questionnaire at 1-year (20). The results of TAVR UNLOAD should provide further clarity on whether the high cardiac event rates reported by van Gils et al. can be modified by earlier AVR. Moreover, this trial should improve our understanding of the prognostic importance of moderate valvular impedance in patients with LV dysfunction.
In summary, van Gils et al. report that among mostly symptomatic heart failure patients with moderate AS, one in three patients is dead and less than one in two is alive without cardiac complications at 4-year follow-up. These data force cardiovascular clinicians to re-consider our approach to patients with moderate AS and comorbid LVSD. Optimal medical therapy for LVSD certainly remains the foundation for treating these patients, and the data from van Gils et al. clearly suggests that improvements in adherence to optimal guideline based medical therapy may be possible with only a small minority in that series taking beta-blocker, angiotensin-converting enzyme inhibitor/angiotensin receptor blocker (ACEI/ARB), and mineralocorticoid receptor antagonist (MRA) in combination. However, early AVR in these patients may provide an opportunity to deliver a durable and potentially life-saving therapy to this high-risk group. Future studies should provide important insights in this arena in the coming years.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare
References
- Ross J Jr, Braunwald E. Aortic stenosis. Circulation 1968;38:61-7. [Crossref] [PubMed]
- Magne J, Lancellotti P, Piérard LA. Exercise testing in asymptomatic severe aortic stenosis. JACC Cardiovasc Imaging 2014;7:188-99. [Crossref] [PubMed]
- Masri A, Goodman AL, Barr T, et al. Predictors of Long-Term Outcomes in Asymptomatic Patients With Severe Aortic Stenosis and Preserved Left Ventricular Systolic Function Undergoing Exercise Echocardiography. Circ Cardiovasc Imaging 2016;9:e004689. [Crossref] [PubMed]
- Nishimura RA, Otto CM, Bonow RO, et al. 2014 AHA/ACC guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Thorac Cardiovasc Surg 2014;148:e1-e132. [Crossref] [PubMed]
- Joint Task Force on the Management of Valvular Heart Disease of the European Society of Cardiology (ESC); European Association for Cardio-Thoracic Surgery (EACTS), Vahanian A, et al. Guidelines on the management of valvular heart disease (version 2012). Eur Heart J 2012;33:2451-96. [Crossref] [PubMed]
- van Gils L, Clavel MA, Vollema EM, et al. Prognostic Implications of Moderate Aortic Stenosis in Patients With Left Ventricular Systolic Dysfunction. J Am Coll Cardiol 2017;69:2383-92. [Crossref] [PubMed]
- Kennedy KD, Nishimura RA, Holmes DR Jr, et al. Natural history of moderate aortic stenosis. J Am Coll Cardiol 1991;17:313-9. [Crossref] [PubMed]
- Rosenhek R, Klaar U, Schemper M, et al. Mild and moderate aortic stenosis. Natural history and risk stratification by echocardiography. Eur Heart J 2004;25:199-205. [Crossref] [PubMed]
- Yechoor P, Blaustein AS, Bakaeen FG, et al. The natural history of moderate aortic stenosis in a veteran population. J Thorac Cardiovasc Surg 2013;145:1550-3. [Crossref] [PubMed]
- SOLVD Investigators, Yusuf S, Pitt B, et al. Effect of enalapril on survival in patients with reduced left ventricular ejection fractions and congestive heart failure. N Engl J Med 1991;325:293-302. [Crossref] [PubMed]
- McMurray JJ, Packer M, Desai AS, et al. Angiotensin-neprilysin inhibition versus enalapril in heart failure. N Engl J Med 2014;371:993-1004. [Crossref] [PubMed]
- Taylor AL, Ziesche S, Yancy C, et al. Combination of isosorbide dinitrate and hydralazine in blacks with heart failure. N Engl J Med 2004;351:2049-57. [Crossref] [PubMed]
- Khot UN, Novaro GM, Popović ZB, et al. Nitroprusside in critically ill patients with left ventricular dysfunction and aortic stenosis. N Engl J Med 2003;348:1756-63. [Crossref] [PubMed]
- Lancellotti P, Magne J. Valvuloarterial impedance in aortic stenosis: look at the load, but do not forget the flow. Eur J Echocardiogr 2011;12:354-7. [Crossref] [PubMed]
- Maréchaux S, Carpentier E, Six-Carpentier M, et al. Impact of valvuloarterial impedance on left ventricular longitudinal deformation in patients with aortic valve stenosis and preserved ejection fraction. Arch Cardiovasc Dis 2010;103:227-35. [Crossref] [PubMed]
- Samarendra P. Usefulness of valvuloarterial impedance to predict adverse outcomes in patients with asymptomatic aortic stenosis. J Am Coll Cardiol 2010;55:1164-5; author reply 1165-6. [Crossref] [PubMed]
- Hachicha Z, Dumesnil JG, Pibarot P. Usefulness of the valvuloarterial impedance to predict adverse outcome in asymptomatic aortic stenosis. J Am Coll Cardiol 2009;54:1003-11. [Crossref] [PubMed]
- Lancellotti P, Donal E, Magne J, et al. Impact of global left ventricular afterload on left ventricular function in asymptomatic severe aortic stenosis: a two-dimensional speckle-tracking study. Eur J Echocardiogr 2010;11:537-43. [Crossref] [PubMed]
- Samad Z, Vora AN, Dunning A, et al. Aortic valve surgery and survival in patients with moderate or severe aortic stenosis and left ventricular dysfunction. Eur Heart J 2016;37:2276-86. [Crossref] [PubMed]
- Spitzer E, Van Mieghem NM, Pibarot P, et al. Rationale and design of the Transcatheter Aortic Valve Replacement to UNload the Left ventricle in patients with ADvanced heart failure (TAVR UNLOAD) trial. Am Heart J 2016;182:80-8. [Crossref] [PubMed]


