Long-term adherence to continuous positive airway pressure in patients with rapid eye movement-only obstructive sleep apnea: a prospective cohort study
Introduction
Obstructive sleep apnea (OSA) is a common disorder that results in repetitive closure of the upper airway during sleep and intermittent hypoxemia (1). Recent data estimate the prevalence of moderate to severe OSA to range from 10–17% in middle-aged and elderly men (2). OSA can occur during rapid eye movement (REM) and non-REM (NREM) sleep (3). OSA during REM sleep is a special form of OSA that occurs predominantly during REM sleep and is called REM-predominant OSA. A limited number of studies with a small number of patients and different definitions for REM-predominant OSA have assessed REM-predominant OSA and reported a clinical prevalence of 14% to 36% of all OSA cases (4). REM-predominant OSA tends to occur more frequently in women, children and young adults, and has a lower apnea hypopnea index (AHI) (5-7). Previous studies have shown that REM-predominant OSA is not independently associated with excessive daytime sleepiness or reduced quality of life after adjusting for the duration of NREM sleep (8-10). The clinical significance of REM-predominant OSA was underestimated for a long time. Hence, REM-predominant OSA was undertreated and under-investigated, which resulted in very limited data on the efficacy of treatment of REM-predominant OSA. Nevertheless, as REM sleep is associated with increased sympathetic activity and cardiovascular instability (11), theoretically, REM-predominant OSA may be associated with more serious cardiovascular adverse events compared to NREM OSA. Recent data suggest that REM-predominant OSA may be associated with a significant cardiovascular risk. The data from the Wisconsin Sleep Cohort showed that REM-predominant OSA was cross-sectionally and longitudinally associated with hypertension (12). Moreover, in the same cohort, a dose-response relationship between REM-AHI and non-dipping blood pressure (BP) was reported. Patients with an REM-AHI of ≥15 had a three-fold higher risk of developing non-dipping systolic BP, and a four-fold higher relative risk of non-dipping diastolic BP compared with individuals with an REM-AHI of <1 (13). A recent study showed that in patients not considered to have OSA (based on AHI <10), hypertension was associated with OSA during REM sleep (AHI-REM >20 hours) (14). Therefore, the treatment of REM-predominant OSA appears to be prudent to avoid potential cardiovascular complications. Moreover, REM-predominant OSA has been linked to type 2 diabetes (15). In contrast to NREM-AHI, REM-AHI was independently associated with higher levels of HbA1c (15).
Continuous positive airway pressure (CPAP) is widely considered to be the most effective treatment for OSA (16). Several studies have been conducted to assess CPAP adherence and to define factors that affect or predict CPAP adherence. However, those studies were conducted among patients who were diagnosed with OSA that was not restricted to REM sleep. Two previous studies assessed CPAP adherence among patients with REM-predominant OSA and both reported no difference in CPAP adherence between REM-predominant OSA and non-stage specific OSA (17,18). However, both studies were short-term, and one was retrospective and used both self-reports and objective assessments to define CPAP adherence. No study has prospectively assessed the long-term adherence to CPAP among patients with REM-only OSA. As REM-OSA patients are less symptomatic than non-stage specific OSA (3), we hypothesize that patients with REM-only OSA have lower CPAP adherence. Therefore, we conducted this study to assess long-term CPAP adherence among patients with REM-only OSA and to identify predictors of CPAP adherence among Saudi patients with OSA after the application of a new educational program.
Methods
Subjects
This prospective cohort study included CPAP-naïve consecutive patients who were referred with a clinical suspicion of OSA and had undergone an overnight polysomnography (PSG) in the University Sleep Disorder Center (USDC), King Saud University. Inclusion criteria were age ≥18 years, obstructive AHI ≥5 events/hour, total sleep time >250 min and total time spent in REM sleep ≥15 min, the completion of a therapeutic night and agreement to participate in the study during the period from January 2012 To March 2014. Exclusion criteria included previous surgical procedures for treatment of snoring or OSA. Several criteria have been used to define REM-only OSA; however, there is no standardized definition (17). In this paper we used strict criteria that mandate REM sleep duration of >15 min. Previous studies used less strict criteria (17,18). Before enrollment, patients were interviewed by a sleep physician; a detailed history was obtained and a physical examination was performed, and the data related to demographics, comorbidities and medications were collected. Exclusion criteria consisted of patients with congestive heart failure, daytime hypercapnia (PaCO2 >45 mmHg), neuromuscular diseases and the use of home oxygen. None of the included patients had been diagnosed with OSA or had used CPAP prior to their visit to the USDC. The Epworth Sleepiness Scale (ESS) was used to assess daytime sleepiness. The ESS is a validated questionnaire that has eight items to assess the likelihood of dozing in a variety of daily living situations (19).
The study was approved by the institutional review board of the College of Medicine, King Saud University (16/0533/IRB), and informed consent was obtained from the participants.
Study protocol
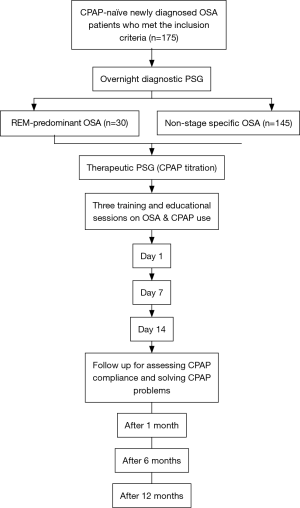
Figure 1 summarizes the study protocol. Patients spent two nights in the USDC. The first night was a diagnostic night, and the second night was a therapeutic night in which CPAP titration was applied. Therapeutic study was done within two weeks of the diagnostic study. After the therapeutic PSG, patients received an education and training session on OSA and CPAP usage. Follow-ups of patients were carried out prospectively in the clinic at 1, 6 and 12 months.
CPAP adherence in the REM-only OSA patients was compared with CPAP adherence of the non-stage specific OSA patients who followed the same study protocol.
Education and training program
A health educationalist explained to the patients the diagnostic and therapeutic overnight sleep studies and the CPAP titration procedure. The best mask was selected before the therapeutic study began. After the sleep study was completed, a meeting was arranged between each patient and a sleep physician. The meeting included a discussion about the results of the sleep study, OSA complications, the beneficial effects of CPAP therapy, and how to use the machine. All of the patients received an educational leaflet on OSA and CPAP therapy. The educational points were reviewed with the patients during each follow-up visit by a sleep technologist and a health educationalist.
In the first 2 weeks following the therapeutic sleep study, the patients underwent 3 training classes on the operation and maintenance of the CPAP machines, on mask fitting and removal, humidifiers and filters: (I) class 1: the day they received CPAP; (II) class 2: after 1 week of using CPAP; (III) class 3: after 2 weeks of using CPAP.
PSG
Standard PSG was performed with four leads of electroencephalography (EEG: C1-A4, C2-A3, O1-A4, O2-A3), electrooculography (EOG), chin electromyography (EMG), electrocardiography (EKG), oxygen saturation, chest and abdominal wall movements, air flow (thermistor and nasal pressure), and sleep position using Alice® diagnostic equipment (Philips, Respironics Inc., Murrysville, PA, USA). Scoring was performed manually according to established scoring criteria (20). Apnea was defined as a drop in the peak thermal sensor excursion of ≥90% of the baseline for ≥10 seconds. Hypopneas were scored if the nasal pressure signal decreased by ≥50% for at least ≥10 seconds, resulting in a ≥3% decrease in oxygen saturation from the pre-event baseline or an arousal. The AHI was calculated by dividing the number of apneas and hypopneas by total sleep time in hours and is expressed as events/hour. The desaturation index was calculated by dividing the number of desaturations (drop in oxygen of ≥3%) by the total sleep time and is expressed as events per hour of sleep. Obstructive AHI was calculated during REM sleep (REM-AHI) and during NREM sleep (NREM-AHI). REM-only OSA was defined as an obstructive AHI of ≥5, with a REM-AHI that was twice the NREM-AHI (REM-AHI/NREM-AHI of >2), a NREM-AHI of <15, and a minimum of 15 min of REM sleep. Patients who had an obstructive AHI >5 events/hour, and did not meet the criteria for REM-only OSA were included in the non-stage specific OSA group.
OSA was defined according to the International Classification of Sleep Disorders (ICSD 2005) (21).
CPAP titration protocol
The use of therapeutic PSG with CPAP titration was decided by the treating physician if the patient met the definition of OSA (22). CPAP titration was performed according to the American Academy of Sleep Medicine guidelines (23). All of the machines had a built-in heated humidifier.
Definitions of successful CPAP titration and good adherence
Successful titration was defined as a residual AHI of <5 events/hour on optimal CPAP pressure, including supine REM sleep at the designated optimal pressure during the CPAP titration study (23). In REM-only OSA, successful CPAP titration was defined as REM-AHI of <5 events/hour.
In this project, we used the American Thoracic Society (ATS) definition of CPAP adherence (24). Good adherence was defined as the use of CPAP regularly for >4 hours/night, for >70% of the recorded period. Partial adherence was defined as CPAP use for more than 2 hours/night associated with a subjective improvement in OSA-related symptoms, namely improved daytime sleepiness as measured by the ESS, and subjective improvement in quality of life (24). Those who stopped using CPAP or who did not meet the above criteria were identified as non-users (24). CPAP adherence was assessed by downloading mask-on time tracking data from CPAP machines to a computer through a card that contained a microprocessor chip, which allows for the objective measurement of CPAP therapy adherence (25).
The CPAP adherence follow-up protocol
The patients were followed prospectively at 1, 6, and 12 months after the initiation of CPAP therapy for the assessment of CPAP adherence, the management of CPAP problems, and a review of the educational points about OSA and the advantages of CPAP therapy. During each follow up visit, patients were interviewed to check for technical problems and side effects related to the CPAP machine and its usage. The downloaded data provided information on adherence, residual AHI, and mask leak. CPAP adherence was determined objectively during each visit. In between follow up visits, patients had direct access to the USDC via a telephone call during daytime working hours for troubleshooting and were able to visit the CPAP clinic if needed within 1–2 weeks.
A data entry form that included commonly faced side effects such as mask discomfort, intolerance and claustrophobia, nasal congestion or dryness, nasal bridge redness or ulceration, gastric distension, eye discomfort or irritation, air leak, air hunger and noisy machine was completed (26). Data were collected during each visit.
Statistical analysis
The data are shown as the mean ± standard deviation (SD) and median (25th–75th percentile) in case of non-normal distribution. The comparison of categorical variables between groups was performed with the chi-square test. The comparison of continuous variables was performed with Student’s t-test or Mann-Whitney U test if normality theory violated. To explore associations between CPAP adherence and independent factors, a preliminary analysis used a univariable logistic regression model; one explanatory variable was tested in the model at a time after adjusting for age, gender, PSG parameters, comorbidities CPAP side-effects and levels of education. Subsequently, variables with significant p-values were evaluated further using a multi-variable logistic regression model (27). A P value of ≤0.05 was considered statistically significant. The variables had no multicollinearity based on correlation matrix. The data were analyzed using Statistical Package for Social Sciences (SPSS), IBM version 22 (SPSS Inc., Chicago, IL, USA) software.
Results
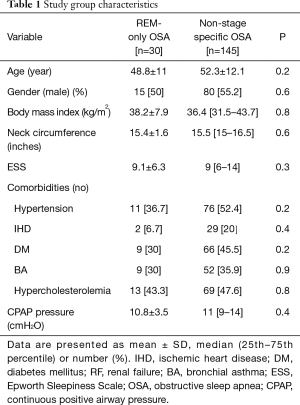
During the study period, 175 patients agreed to participate in the study. Thirty patients met the criteria for REM-only OSA, and the remaining (n=145) patients formed the non-stage specific OSA group. The mean age of participants was 51.7±12 years, the body mass index (BMI) was 36.6 (31.7–43.4) kg/m2 and AHI was 53.0 (20.4–91.0) events/hour. Table 1 shows the characteristics of both groups. There were no differences in age, BMI, ESS, comorbidities or the optimal CPAP pressure that was needed to eliminate obstructive events.
Full table
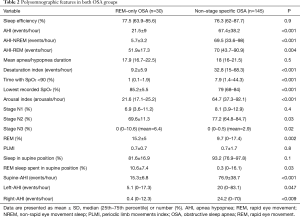
Table 2 shows the polysomnographic features of participants in both OSA groups. AHI and desaturation index were significantly lower in the REM-only OSA patients [21.5±9 vs. 67.4±38.2 events/hour, and 9.2±5.9 vs. 32.8 (15–68.3) events/hour, respectively]. Moreover, the percentages of N3 stage and REM sleep stage were significantly higher in the REM-only OSA patients.
Full table
Within the REM-only OSA group, 12 (40%) patients had mild OSA (AHI 5–15 events/hour), and 18 (60%) had moderate OSA (AHI from >15–30 events/hour). Among non-stage specific OSA patients, mild OSA was diagnosed in 27 (26%) patients, moderate OSA was diagnosed in 15 (10%) patients, and severe OSA (AHI ≥30 events/hour) was diagnosed in 118 (81%) patients.
CPAP adherence
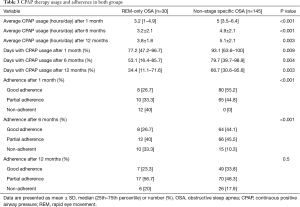
Table 3 presents CPAP usage and adherence at 1, 6 and 12 months. The number of hours used per day was significantly lower in the REM-only OSA group at 1, 6 and 12 months. However, the number of hours of CPAP use per day in the REM-only OSA patients increased from 3.2 (1–4.9) hours after 1 month to 3.8±1.8 hours at the end of the study. The percentage of patients who continued to use CPAP was significantly lower in the REM-only OSA group at 1 and 6 months. However, this difference disappeared at 12 months. Approximately 80% of the enrolled participants in both groups were still using CPAP at the end of the study. At the end of the study, 23.3% of REM-only OSA patients met the criteria for good adherence and 56.7% met the criteria for partial adherence. The percentage of days during which CPAP was used was significantly lower in the REM-only OSA patients at 1, 6 and 12 months (Table 3).
Full table
Predictors of good CPAP adherence
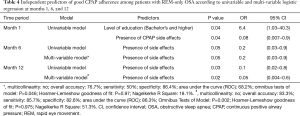
Table 4 shows the predictors of good CPAP adherence at months 1, 6, and 12 using univariable and multi-variable logistic regression analysis. During month 1, a bachelor and postgraduate level of education was a predictor of good CPAP adherence, while “presence of CPAP side effects” was a predictor of lower CPAP adherence according to univariate analysis. At months 6 and 12, “presence of side effects” was an independent predictor of CPAP adherence. Reported side effects included one or more of the following: mask discomfort, noise complaints, nose/mouth dryness or eye discomfort or irritation
Full table
Side effects
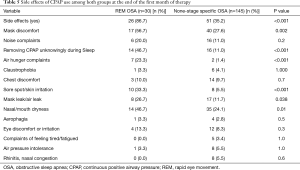
At the end of the first month of the study, side effects in general were more in the REM-only OSA. Side effects were reported in 86.7% of the REM-only OSA vs. 35.2% in the non-stage specific OSA (P<0.001). Table 5 presents a comparison between the two groups with regards to side effects. Mask discomfort, facial skin irritation and nasal congestion were reported more in the REM-only OSA.
Full table
Discussion
In this study, we assessed long-term CPAP adherence prospectively and objectively among patients with REM-only OSA after they had completed an education and support program. The strength of this study is that we used a strict definition of REM-only OSA by including duration of REM sleep of at least 15 min as a criterion. Previous studies used less strict criteria (17,18).
The study shows that more than 80% of patients with REM-only OSA were still using CPAP at the end of the study. However, at the end of the study, the average nightly use of CPAP was 3.8 hours/night, which does not cover the whole nocturnal sleep period (26). Moreover, as REM sleep increases in the early morning hours, using CPAP only for 4 hours is insufficient (10). Patients usually start using CPAP at bedtime; hence, if the mean duration of CPAP use is approximately 4 hours, it is likely that a significant proportion of the early morning REM-OSA remains untreated. This has significant clinical implications as recent data has suggested that REM-predominant OSA may be associated with a significant cardio-metabolic risk (12,13). Mokhlesi et al. reported that there was a strong longitudinal association between REM-predominant OSA and nocturnal incident non-dipping of systolic and diastolic BP (13). Moreover, Grimaldi et al. found that the use of CPAP for 3 hours and 4 hours after lights off would leave 75% and 60% of REM-related obstructive events untreated, respectively (15). In their analysis, the investigators predicted that those 4 hours of CPAP use would be associated with a decrease in HbA1c by approximately 0.25%. However, 7 hours of CPAP use would cover more than 85% of REM sleep and would be associated with a decrease in HbA1c by as much as 1% (15). The currently accepted definition of adequate adherence of 4 hours nightly of CPAP use for 70% of nights translates into 2.8 hours every night (13,28). Hence, this definition of adequate CPAP adherence needs to be revisited, and a new definition is needed, particularly for patients with REM-predominant OSA. Not using CPAP in the early morning during REM sleep may partially explain why CPAP therapy does not lower BP in some patients. Further research is needed to define the optimal duration of CPAP use that is needed to control BP and improve glycemic control, particularly in patients with REM-predominant OSA. Therefore, future studies should look into the cardio-metabolic complications of REM-predominant OSA and the number of hours of CPAP use that is needed to reduce complications. Moreover, it is important to increase the awareness of practitioners about the impact of not using CPAP in the early morning sleep hours on cardio-metabolic complications in patients with REM-predominant OSA, and practitioners need to encourage patients to use CPAP for the entire sleep period.
Only two previous studies have assessed CPAP adherence among patients with REM-predominant OSA (17,18). Both studies reported that there was no difference in CPAP adherence between REM-predominant OSA and non-stage specific OSA. However, the two studies did report short-term adherence data. The study by Su et al. was a retrospective study that assessed CPAP adherence among REM-predominant OSA patients in the first 90 days of use with both subjective (self-reported) and objective data (18). The other study by Conwell et al. assessed CPAP adherence in the first 30 days of CPAP use in patients with REM-predominant OSA (17). Although Conwell et al. reported no difference in adherence between patients with REM-predominant OSA and non-stage specific OSA, the mean duration of CPAP use per night in REM-predominant OSA was comparable to our findings (3.6 hours) (17).
Our study is the first study to report long-term adherence data in patients with REM-only OSA who had undergone an educational program and had been closely monitored. CPAP adherence among patients with REM-only OSA was lower than patients with non-stage specific OSA at months 1 and 6 and was lower than previously published adherence data in Saudi patients with general OSA (26). However, there was no difference in adherence between the two groups at 12 months (Table 3). Although the overall adherence was comparable in the REM-only and non-stage specific groups at the end of the study, the mean hours of CPAP usage per day was significantly lower in the REM-only OSA group. The lower adherence among the individuals with REM-only OSA may reflect the lower severity of OSA in this group. Previous studies have reported that CPAP adherence correlates with OSA severity, which is reflected by AHI or the oxygen desaturation index (29,30). In addition to a significantly higher AHI and desaturation index in the non-stage specific OSA patients, stage N2 was higher and stages N3 and REM were lower in the non-stage specific OSA patients. A higher N2 stage and lower REM and N3 stages may reflect an increased OSA severity. Stage N2 has been shown to increase in percentage across OSA severity; REM sleep showed an inverse pattern (31), which reflects worse sleep quality (31). It is likely that patients with more severe OSA, as reflected by an increased N2 stage and a reduced REM sleep stage have better CPAP adherence. Hence, our results are in agreement with the findings of previous studies that demonstrated that the severity of OSA correlates with CPAP adherence. There was a decrease in adherence rate at the end of the study in NREM related OSA; however, no much change occurred in REM-OSA in our study. The decline is adherence in the non-stage specific OSA is comparable to previous studies that assessed long-term adherence (26,32). Our study is the first study to assess long-term CPAP adherence in patients with REM-predominant OSA; therefore, there are no available data to compare with our results. Patients with REM-predominant OSA may behave differently. Nevertheless, long-term good CPAP adherence continued to be better in non-stage specific OSA at the end of the study.
The nightly duration of CPAP use in patients with REM-only OSA increased from 3 hours/night during the first month of CPAP use to 3.8 hours/night at the end of the study. The increased duration of CPAP use over time may reflect the positive impact of the educational and training sessions on CPAP adherence. A recent meta-analysis of 30 randomized parallel controlled trials demonstrated that supportive ongoing interventions increased machine usage by approximately 50 min/night, and the percentage of patients who used their machines for longer than 4 hours/night increased from 59% to 75% (33). Moreover, educational interventions increased machine usage by approximately 35 min/night, and increased the percentage of patients who used their machines for longer than 4 hours/night from 57% to 70% (33).
Several studies have attempted to use demographics or initial PSG results to predict subsequent CPAP adherence among patients with general OSA (34). There have been no data available on the predictors of CPAP adherence among patients with REM-only OSA. The “presence of CPAP side effects” remains a consistent independent predictor of CPAP adherence in our cohort of patients with REM-only OSA.
A limitation of this study is that it was conducted in a single tertiary research center, and the data cannot be extrapolated to other sleep disorder centers or to patients in the community. Moreover, as we studied REM-only OSA, which is usually a milder form of OSA, our findings cannot be applied to patients with mixed REM and NREM OSA, even if the AHI-REM was higher than AHI-NREM.
Conclusions
In summary, this prospective long-term study shows that CPAP adherence is lower among patients with REM-only OSA compared to patients with non-stage specific OSA. Although approximately 80% of patients with REM-only OSA continue to use CPAP after 12 months of the initiation of CPAP therapy, the mean duration of CPAP use was 3.8 hours/night. This duration of CPAP use is not long enough to cover the early morning hours, which contains more REM sleep periods. The “presence of CPAP-related side effects” was a persistent predictor of poor CPAP adherence. Future studies should define the optimal duration of nocturnal CPAP use that is needed in patients with REM-only OSA to prevent cardio-metabolic complications.
Acknowledgements
Funding: This study was supported by a grant from the Strategic Technologies Program of the National Plan for Sciences and Technology and Innovation in the Kingdom of Saudi Arabia (08-MED511-02).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the institutional review board of the College of Medicine, King Saud University (16/0533/IRB), and informed consent was obtained from the participants.
References
- Semelka M, Wilson J, Floyd R. Diagnosis and Treatment of Obstructive Sleep Apnea in Adults. Am Fam Physician 2016;94:355-60. [PubMed]
- Peppard PE, Young T, Barnet JH, et al. Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol 2013;177:1006-14. [Crossref] [PubMed]
- Köseoğlu HI, Kanbay A, Demir O. A Different Clinical Type of OSAS: REM-predominant OSAS. Eurasian J Pulmonol 2015;17:92-7. [Crossref]
- Mokhlesi B, Punjabi NM. "REM-predominant " obstructive sleep apnea: an epiphenomenon or a clinically important entity? Sleep 2012;35:5-7. [Crossref] [PubMed]
- Haba-Rubio J, Janssens JP, Rochat T, et al. Rapid eye movement-related disordered breathing: clinical and polysomnographic features. Chest 2005;128:3350-7. [Crossref] [PubMed]
- Goh DY, Galster P, Marcus CL. Sleep architecture and respiratory disturbances in children with obstructive sleep apnea. Am J Respir Crit Care Med 2000;162:682-6. [Crossref] [PubMed]
- Alotair H, Bahammam A. Gender differences in Saudi patients with obstructive sleep apnea. Sleep Breath 2008;12:323-9. [Crossref] [PubMed]
- Chervin RD, Aldrich MS. The relation between multiple sleep latency test findings and the frequency of apneic events in REM and non-REM sleep. Chest 1998;113:980-4. [Crossref] [PubMed]
- Chami HA, Baldwin CM, Silverman A, et al. Sleepiness, quality of life, and sleep maintenance in REM versus non-REM sleep-disordered breathing. Am J Respir Crit Care Med 2010;181:997-1002. [Crossref] [PubMed]
- Mokhlesi B. REM-predominant obstructive sleep apnea: to treat or not to treat? J Clin Sleep Med 2012;8:249-50. [PubMed]
- Somers VK, Dyken ME, Mark AL, et al. Sympathetic-nerve activity during sleep in normal subjects. N Engl J Med 1993;328:303-7. [Crossref] [PubMed]
- Mokhlesi B, Finn LA, Hagen EW, et al. Obstructive sleep apnea during REM sleep and hypertension. results of the Wisconsin Sleep Cohort. Am J Respir Crit Care Med 2014;190:1158-67. [Crossref] [PubMed]
- Mokhlesi B, Hagen EW, Finn LA, et al. Obstructive sleep apnoea during REM sleep and incident non-dipping of nocturnal blood pressure: a longitudinal analysis of the Wisconsin Sleep Cohort. Thorax 2015;70:1062-9. [Crossref] [PubMed]
- Appleton SL, Vakulin A, Martin SA, et al. Hypertension Is Associated With Undiagnosed OSA During Rapid Eye Movement Sleep. Chest 2016;150:495-505. [Crossref] [PubMed]
- Grimaldi D, Beccuti G, Touma C, et al. Association of obstructive sleep apnea in rapid eye movement sleep with reduced glycemic control in type 2 diabetes: therapeutic implications. Diabetes Care 2014;37:355-63. [Crossref] [PubMed]
- Epstein LJ, Kristo D, Strollo PJ Jr, et al. Clinical guideline for the evaluation, management and long-term care of obstructive sleep apnea in adults. J Clin Sleep Med 2009;5:263-76. [PubMed]
- Conwell W, Patel B, Doeing D, et al. Prevalence, clinical features, and CPAP adherence in REM-predominant sleep-disordered breathing: a cross-sectional analysis of a large clinical population. Sleep Breath 2012;16:519-26. [Crossref] [PubMed]
- Su CS, Liu KT, Panjapornpon K, et al. Functional outcomes in patients with REM-predominant obstructive sleep apnea treated with positive airway pressure therapy. J Clin Sleep Med 2012;8:243-7. [PubMed]
- Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep 1991;14:540-5. [Crossref] [PubMed]
- Berry RB, Brooks R, Gamaldo CE, et al. The AASM Manual for the Scoring of Sleep and Associated Events: Rules, Terminology and Technical Specifications, Version 2.1. Darien, Illinois: American Academy of Sleep Medicine, 2014.
- American Academy of Sleep Medicine. International classification of sleep disorders (ICSD): Diagnostic and coding manual. 2nd ed. Westchester(IL): American Academy of Sleep Medicine, 2005.
- American Academy of Sleep Medicine. International Classification of Sleep Disorders. 3rd ed. Darien, IL: American Academy of Sleep Medicine,2014.
- Kushida CA, Chediak A, Berry RB, et al. Clinical guidelines for the manual titration of positive airway pressure in patients with obstructive sleep apnea. J Clin Sleep Med 2008;4:157-71. [PubMed]
- Schwab RJ, Badr SM, Epstein LJ, et al. An official American Thoracic Society statement: continuous positive airway pressure adherence tracking systems. The optimal monitoring strategies and outcome measures in adults. Am J Respir Crit Care Med 2013;188:613-20. [Crossref] [PubMed]
- Weaver TE, Sawyer AM. Adherence to continuous positive airway pressure treatment for obstructive sleep apnoea: implications for future interventions. Indian J Med Res 2010;131:245-58. [PubMed]
- BaHammam AS, Alassiri SS, Al-Adab AH, et al. Long-term compliance with continuous positive airway pressure in Saudi patients with obstructive sleep apnea. A prospective cohort study. Saudi Med J 2015;36:911-9. [Crossref] [PubMed]
- Hidalgo B, Goodman M. Multivariate or multivariable regression? Am J Public Health 2013;103:39-40. [Crossref] [PubMed]
- Sawyer AM, Gooneratne NS, Marcus CL, et al. A systematic review of CPAP adherence across age groups: clinical and empiric insights for developing CPAP adherence interventions. Sleep Med Rev 2011;15:343-56. [Crossref] [PubMed]
- Kohler M, Smith D, Tippett V, et al. Predictors of long-term compliance with continuous positive airway pressure. Thorax 2010;65:829-32. [Crossref] [PubMed]
- McArdle N, Devereux G, Heidarnejad H, et al. Long-term use of CPAP therapy for sleep apnea/hypopnea syndrome. Am J Respir Crit Care Med 1999;159:1108-14. [Crossref] [PubMed]
- Bianchi MT, Cash SS, Mietus J, et al. Obstructive sleep apnea alters sleep stage transition dynamics. PLoS One 2010;5:e11356. [Crossref] [PubMed]
- Chai-Coetzer CL, Luo YM, Antic NA, et al. Predictors of long-term adherence to continuous positive airway pressure therapy in patients with obstructive sleep apnea and cardiovascular disease in the SAVE study. Sleep 2013;36:1929-37. [Crossref] [PubMed]
- Wozniak DR, Lasserson TJ, Smith I. Educational, supportive and behavioural interventions to improve usage of continuous positive airway pressure machines in adults with obstructive sleep apnoea. Cochrane Database Syst Rev 2014;1:CD007736. [PubMed]
- BaHammam AS, Hussain A, Al-Asmri M. Adherence to and Complications of CPAP in Obstructive Sleep Apnea: Key Determinants. In: Esquinas AM, editor. Noninvasive Mechanical Ventilation: Theory, Equipment, and Clinical Applications. Switzerland: Springer International Publishing, 2016:703-15.


