Uniportal video assisted thoracic surgery with 2 cm skin incision for right middle lobectomy with systematic lymphadenectomy
Introduction
Nowadays, the incidence of lung cancer is very high, increasing at an annual rate of 26.9% (1). The amount of lung cancer surgery is enormous, as the operation ways are diverse including four-ports, three-ports, two-ports and uniportal video-assistant thoracic surgery (VATS). Uniportal VATS (single incision) refers to a small skin incision between ribs into which the thoracoscopic len and all surgical equipments are put in the process of the whole operation. In 2000, Rocco et al. (2) used single incision VATS to operate some simple surgery such as pulmonary bulla resection, lung tissue biopsy and so on. With the development of surgical instruments and surgical techniques, Gonzalez et al. (3) firstly reported uniportal VATS for lobectomy and lymph node dissection in 2011. Several clinical reports introduced that uniportal VATS has no significant difference compared with multi-ports VATS for the treatment of lung cancer (4-6). However, the diameter of single incision was not defined clearly, ranging from 4 to 6 cm mostly. We believed in less invasive and more precise that uniportal video-assisted thoracoscopic lobectomy with 2 cm incision could be. Actually, uniportal VATS with 2 cm incision has shown more advantages including less postoperative pain (7), less skin numbness, less paresthesia, quicker recovery, and better cosmetology (8) and stronger psychological comfort especially for young women. Therefore, we performed uniportal VATS with systemic lymphadenectomy on right middle lobe using a 2 cm diameter incision.
In present, more experience and exploration about uniportal VATS surgery are still needed. Therefore, we summarize the experience of precise uniportal VATS with 2 cm incision for right middle lobectomy.
Clinical data
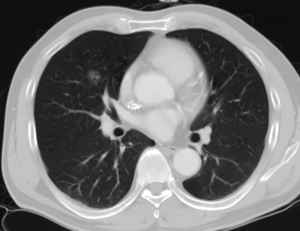
A 53-year-old man presented with a finding of a right middle lobe lesion in the process of routine health examination with chest computed tomography (CT) screening. Chest CT imaging showed a 15 mm × 13 mm solitary ground glass opacity (GGO) with air bronchogram in the right middle lobe, and mean CT value of the GGO was 618 Hu (Figure 1). He accepted standard anti-inflammatory treatment for 2 weeks, then he was scanned with CT again, the lesion was same as before. Lung function was evaluated via formal spirometry with a FEV1 of 3.54 L (105.1% predicted), a FVC of 4.25 L (97.7% predicted), a FEV1/ FVC ratio of 83.28% and MVV of 113.43 L (113.2% predicted). The bronchoscopy was examined and had no significant positive findings, but the patient refused steadfastly CT-guided biopsy. Therefore, he was examined with a positron emission tomography and computerized tomography scan (PET-CT) preoperatively to ensure that there was no evidence of metastatic disease.
Surgery procedures
As there are no changes for the lesion in the patient after standard anti-inflammatory treatment for two weeks, the density and form of GGO look like malignant lesion, moreover, the lesion located in the region of the hilar, and cannot be had wedge resection for frozen pathological examination, so we decided to make right middle lobectomy directly, and we had a radical lymphadenectomy after frozen pathology revealed adenocarcinoma.
Anesthesia and positioning
The patient was placed in the left lateral decubitus position with the upper arms extended to 90° and the forearms and hands covered his head without universal screen and arm board (Figure 2). To gain more operative space and protect the intercostal neurovascular bundles, a soft pillow was put under the left side of chest. General anesthesia was completed and intubation was achieved via a double lumen endobronchial tube. The surgeon and the assistant stood on both sides of the patient respectively to maintain the same thoracoscopic vision during all steps of surgery and to experience more coordinated movements. Usually, the surgeon held the suction tool in the left hand and the coagulation hook in the right hand. One assistant held the thoracoscope in two hands intently, another assistant operated endoscopic grasper and so on (Figure 3).


Ports
The skin incision, approximate 2 cm long in diameter (Figure 4), was operated in the 4th intercostal space in the posterior axillary line position. This incision was good for both the middle lobes resection and radical lymphadenectomy. Plastic wound protector kept the utility wound open and prevented the lung from expanding when suction was applied and prevented intercostal vessels and nerve from injury when instruments were operated (9). A 30°, standard-definition, 5-mm thoracoscope was usually placed at the posterior part of the utility incision with the working instruments in the anterior part for most of the surgical process.

Right middle lobectomy (Figure 5)
Instruments must preferably be long and curved to allow simultaneous insertion of 2 or 3 instruments including a two-joint clamp (proximal and distal articulation ease of instrumentation), a suction and an electric coagulation hook except the thoracoscope lens (4). As the utility incision was very small, every instrument must be set good position and angle so as to be operated conveniently without “fight”. Moreover, the vessel and bronchus of right middle lobe were just below the incision, there was no operation angle for staple insertion, so the operation was very difficult. When horizontal and oblique fissure development was good and well-defined, we used the electric coagulation hook to dissect the visceral pleura in the ways of unidirectional operation, however, we found that a large lymph node (11th group) located in the oblique fissure. First of all, one right middle pulmonary artery was dissected carefully and was clamped with titanium clip, then was cut off with harmonic scalpel along the distal end, so did another artery. The large lymph node (11th group) was dissected carefully to avoid blooding. Secondly, horizontal fissure was cut open by harmonic scalpel, and right middle bronchus was dissected avoiding bronchial arterial hemorrhage, because there was no angle for staple insertion for the middle vein or bronchus from the incision, we used electric coagulation hook to cut right middle bronchus off at 2 cm in the distance to middle bronchus root, the key point was that the operation was careful to avoid damaging right middle vein. At this moment, the right middle pulmonary vein, stripping the surrounding tissue, was easily put in different angle, then was resected using a rotary stapler (Covidien Inc., Mansfield, MA, USA). When the lobectomy was completed, the lobe was removed in a protective bag through the utility incision. Lastly, the right middle bronchial trunk was hung up by a thread and resected by the rotated stapler with decent angle.
Completed mediastinal lymphadenectomy
Intraoperative frozen pathological section revealed adenocarcinoma, so completed mediastinal lymphadenectomy must be carried out. We were accustomed to use electric coagulation hook rather than harmonic scalpel to dissect the lymph nodes. At first, the assistant pulled the upper lobe backward and exposed hilum lymph nodes, 10th group lymph nodes was dissected. Secondly, the assistant pulled the upper lobes down in order to clearly expose mediastinal lymph nodes, mediastinal pleura was cut open along the right margin of vena cava, the azygos vein was severed with staple because of unable to enter more grasper for pull and exposure, the 2th group and 4th group lymph nodes were completely resected. Thirdly, the assistant pulled the upper lobe forward, the subcarinal lymph node (7th group) was resected radically avoiding esophagus damage. Finally, the lung tissue was re-expanded for air leakage testing for the bronchial stump and pulmonary resection margin (9). One thin 21F chest tube was placed in the anterior part of the incision up to the tip of the thoracic cavity prior to closure of the port site (Figure 6). No additional incisions were made for the chest tube placement.

Postoperative management
The operative time was 145 min. The time of right middle lobectomy was approximately 47 min, and the lymph node dissection spent approximately 50 min. Twenty-one lymph nodes were dissected. The volume of intraoperative bleeding was approximate 100 mL. This patient was directly sent back to the common ward with electrocardiograph monitoring, and early ambulation was asked on the 2nd day after operation, and postoperative drainage continued for 3 days. The chest tube was removed postoperatively when there was sufficient lung expansion on chest radiographs and no air leakage, then the patient went home. Postoperative hospitalization time was four days. There was no complication. Final pathology revealed a T1a2N0M0 lung invasive acinar adenocarcinoma with papillary element and no lymph node metastasis.
Discussion
In present, with the development of medical apparatus and instruments, video-assisted thoracic surgery had become a popular and safe operation including multi-ports and uniport VATS methods. Compared with multi-ports VATS lobectomy, uniportal VATS lobectomy could decrease the chest injury, postoperative pain, and postoperative paresthesia, possibly, only one intercostal space is involved to reduce the skin injury, muscle and nerve severing, and avoiding the use of a trocar could minimize the risk of intercostal nerve injury (3), After surgery, the area of the skin numbness decreased significantly. Additional, compared with multi-ports VATS surgery, uniportal VATS possessed the advantages of small wound and cosmetology, especially for young women. Therefore, uniportal VATS was welcomed by more and more thoracic surgeon (11).
According to the current conventional surgical instruments, 2 cm skin incision is the smallest minimally invasive surgery, operation is extremely difficult. In 2 cm incision, a suction, an electric coagulation hook and a double-jointed forceps always were put into thoracic cavity simultaneously except thoracoscope. Therefore, instruments must preferably be thin, long and curved. The camera must be at 30 degrees to provide a panoramic view. We used 5 mm thoracoscope which significantly spared the more incisional space for other instruments, but its light was a little darker (Figure 5), the surgeon’s eyes would suffer damage. Surgeon was necessarily equipped with ≤5 mm HD thoracoscope in the future.
It was very important to choose intercostal incision. On the left side, we were accustomed to choose the fifth intercostals in the left mid-axillary line, there would be relatively enough distance and decent angle in the process of lobe resection or segment resection, and convenient to the 4th, 5th, and 6th groups lymphadenectomy. However, on the right side, in order to facilitate the 2th and 4th group lymphadenectomy, the fourth intercostal is selected in the right mid-axillary line, therefore, it is more difficult to remove the right middle lobe.
The arrangement of the instruments was also important. We preferred to rest the camera at the dorsal end of the incision directed towards the operating area and positioned instruments of low mobility at the distal end of the incision. The remaining larger incisional space allowed for easier operation and reduced interference. For horizontal and oblique fissure good developing, we used harmonic or electric coagulation hook to dissect the gap. But for horizontal and oblique fissure bad developing, we carefully dissected the anatomic triangle (the intersection of horizontal and oblique fissure) and mediastinal pleura, and dissociated the lung tissue gap between right upper vein and right middle vein with an angled clamp, and could find a “channel”, and cut the horizontal fissure open with stapler along the “channel”. Then right middle artery was dissected easily. When there was no angle for stapler insertion or it was difficult to achieve from the incision, as with the middle lobe artery, we used vascular clips-Hemlock in the proximal blood vessels, and titanium clips in the distal blood vessels, then necessarily used Harmonic scalpel to cut off the blood vessels. The point was that we used electric coagulation hook to sever the right middle bronchus avoiding the difficult of stapler insertion.
Compared with upper lobe resection and lower lobe resection, in the process of right middle lobe resection with uniportal VATS, the incision was near the hilum, the stapler was vertical with the vessel and bronchus of right middle lobe, and had no enough insertion angle, so we thought the operation was the relatively more difficult in all kinds of lobectomy with 2 cm skin incision uniportal VATS. The practice is necessary for novice surgeons and assistance is strictly required during the learning curve for uniportal VAT lobectomy, especially with a 2.0-cm-diameter port (12).
Acknowledgements
Funding: This project was supported by the National Natural Science Foundation of China (81371702).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
References
- Comprehensive genomic characterization of squamous cell lung cancers. Nature 2012;489:519-25. [Crossref] [PubMed]
- Rocco G, Martin-Ucar A, Passera E. Uniportal VATS wedge pulmonary resections. Ann Thorac Surg 2004;77:726-8. [Crossref] [PubMed]
- Gonzalez D, Paradela M, Garcia J, et al. Single-port videoassisted thoracoscopic lobectomy. Interact Cardiovasc Thorac Surg 2011;12:514-5. [Crossref] [PubMed]
- Gonzalez-Rivas D, Paradela M, Fernandez R, et al. Uniportal video-assisted thoracoscopic lobectomy: two years of experience. Ann Thorac Surg 2013;95:426-32. [Crossref] [PubMed]
- Shen Y, Wang H, Feng M, et al. Single versus multipleport thoracoscopic lobectomy for lung cancer: a propensity-matched study. Eur J Cardiothorac Surg 2016;49 Suppl 1:i48-53. [PubMed]
- Hsu PK, Lin WC, Chang YC, et al. Multiinstitutional analysis of single-port video-assisted thoracoscopic anatomical resection for primary lung cancer. Ann Thorac Surg 2015;99:1739-44. [Crossref] [PubMed]
- Akter F, Routledge T, Toufektzian L, et al. In minor and major thoracic procedures is uniports uperior to multiport video-assisted thoracoscopicsurgery? Interact Cardiovasc Thorac Surg 2015;20:550-5. [Crossref] [PubMed]
- Yang HC, Noh D. Single incision thoracoscopic lobectomy through a 2.5 cm skin incision. J Thorac Dis 2015;7:E122-5. [PubMed]
- Shen G, Chai Y, Huang L, et al. Uniportal video-assisted thoraco- scopic right upper lobectomy with systematic lymphadenectomy. J Thorac Dis 2016;8:2275-80. [Crossref] [PubMed]
- Liu R, Tan Q, Huang J, et al. Uniportal VATS with 2 cm incision for right middle lobectomy. Asvide 2017;4:519. Available online: http://www.asvide.com/articles/1838
- Gonzalez-Rivas D, Marin JC, Granados JP, et al. Uniportal video- assisted thoracoscopic right upper sleeve lobectomy and tracheoplasty in a 10-year-old patient. J Thorac Dis 2016;8:E966-9. [Crossref] [PubMed]
- Wang Q, Cai YX, Deng Y, et al. Modular 3-cm uniportal video-assisted thoracoscopic left upper lobectomy with systemic lymphadenectomy. J Thorac Dis 2016;8:2264-8. [Crossref] [PubMed]


