Clinical utility of the ventricular septal defect diameter to aorta root diameter ratio to predict early childhood developmental defects or lung infections in patients with perimembranous ventricular septal defect
Introduction
Ventricular septal defect (VSD) is the most common type of congenital heart disease (1). While some VSDs can undergo spontaneous postnatal closure by the time the child reaches 5 years of age (2), the outcomes are usually growth retardation and recurrent infections (3). It is very important, accordingly, for pediatric cardiologists to predict which complications will occur and to choose the most suitable time for treatment. This will result in achieving more scientific-based and individualized therapy in children with VSD.
Previous studies found that VSD diameter closely correlated with the different outcomes. However, using simple VSD diameter to evaluate disease severity has certain shortcomings, due to the effects of age, body weight, and defect shape on the diameter (4). Recently, the ratio between VSD area and body surface area has been considered a more objective reflection of disease severity, providing an important reference for both prognosis and treatment efficacy (5). There is a significantly different spontaneous closure rate between the patients with ratios either smaller or larger than 0.5 cm2/m2 (6). However, the method to calculate the ratio is cumbersome to achieve in clinical practice, due to difficulties in obtaining the body surface index directly. This has resulted in restricted application of the ratio.
Quantitative assessments of the cardiac shunt have been used to indicate VSD severity. The systemic-pulmonary circulation ratio (QP/QS ratio), left ventricular end diastolic diameter (LVDd) and left ventricular fractional shortening (FS) have all been evaluated, with the most widely used method being the QP/QS ratio (5). Catheterization is an invasive and expensive technique that is difficult to apply in the clinical setting, even though it is regarded as the gold standard for measuring VSD severity (7). With the development of color Doppler echocardiography, the measurement of QP/QS ratio has gradually become recognized as a useful method to determine the severity of VSD (5,6). Conventional ultrasonic pulse wave Doppler (PWD) is the most common method to measure the QP/QS ratio clinically, but this technique is limited due to measurement errors that may be related to its relatively complex operation. Other methods to measure the cardiac shunt have proven to be insufficient (8,9).
Therefore, there is a clear need to find a simpler method to assess VSD severity, and this measurement should overcome the effects of age, body mass, and defect shape. Because VSD is a congenital heart disease with a persistent left-to-right cardiac shunt, we hypothesized that the ratio between the diameter of the defect and the aortic root diameter (DVSD/DAR) would be a more suitable variable to accurately reflect the degree of shunted blood and the severity of VSD.
Based on the location of the defect, VSD is divided into four types: perimembranous VSD (pmVSD), muscular VSD (mVSD), subarterial VSD (sVSD) and mixed-type VSD. The hemodynamics vary among the different types, and thus in different treatments and prognoses. The pmVSD is the most common type, so children with isolated pmVSD were enrolled in the present study. Accordingly, we calculated the ratio of DVSD/DAR by color Doppler echocardiography in children with pmVSD and determined its relatedness to the children’s subsequent growth and infection issues. We evaluated whether this ratio could predict the degree of shunted blood and the severity of VSD.
This procedure is easy to perform, since the diameters of the pmVSD and aortic root are easy to measure. This makes the new method more useful in clinical practice.
Methods
Patients
Patients with isolated pmVSD of either gender (n=987) were recruited from the First Affiliated Bethune Hospital, Jilin University, between January 2004 and December 2011. Enrollment criteria included: (I) age ranging from 0.5 to 4.5 years, and (II) isolated pmVSD. Exclusion criteria were: (I) complications of VSD affecting the systemic-pulmonary circulation ratio, such as VSD with membrane aneurysm and aortic valve prolapse; (II) other types of VSD, such as mVSD, sVSD, and mixed-type VSD; (III) VSD as a component of other congenital heart defects (such as Tetralogy of Fallot); (IV)VSD combined with other serious congenital disorders such as cerebral palsy; (V) VSD combined with other serious diseases of other systems, such as leukemia.
Healthy subjects (n=987) having normal findings on physical, electrocardiography, and echocardiography examinations served as the control group. The two groups were age- and gender-matched. The study was approved by the Ethics Committee of the First Affiliated Bethune Hospital, Jilin University and all subjects gave informed consent.
Subgroups
The pmVSD group was subdivided into four groups, according to age: 0.5 to <1.5 y, male n=160 cases and female n=139 cases; 1.5 to ≤2.5 y, male n=151 cases and female n=129; 2.5 to <3.5 y, male n=122 and female n=105; and 3.5 to <4.5 y, male n=100, female n=81.
Each age group was further subdivided into four groups according to DVSD/DAR ratio: (I) 1/5≤ DVSD/DAR <1/4; (II) 1/4≤ DVSD/DAR <1/3; (III) 1/3≤ DVSD/DAR <1/2; and (IV) 1/2≤ DVSD/DAR <2/3.
Height and weight measurements
Measurements were made according to the method of normal physical development research for children 0-6 years of age. This method was provided by the Chinese Ministry of Health.
Color Doppler echocardiography
Two-dimensional echocardiograms were obtained with a TOSHIBA SSH-880CV echocardiography ultrasound (TOSHIBA, Japan). One operator, who was blinded to the different groups, acquired and analyzed all of the images. A 3 MHz frequency probe was placed in the three to four left parasternal intercostals under supine or left lateral position. All measurements were made according to American Society of Echocardiography guidelines (10). Three consecutive cardiac cycles were measured, and average values were obtained.
The following parameters were derived:
- The pmVSD size: the minimum diameter of pmVSD at left ventricular long axis section, the maximum diameter at aorta short axis apical four -chamber and apical five-chamber section, the defect size was calculated as follows, (maximum diameter + minimum diameter)/2.
- The QP/QS ratio: measurement of diameter and velocity time integral of aortic root and the main pulmonary artery at sections of left ventricular long axis and aortic short axis, QP/QS ratio was calculated as follows: (πr12 V1)/ (πr22 V2); r1, radius of the main pulmonary artery; r2, radius of the aortic root; V1, velocity time integral of the main pulmonary artery; and V2, velocity time integral of aortic root.
- The number of pmVSD, location, color Doppler, and blood flow crossing the septum.
- DVSD/DAR, ventricular septal defect size/diameter of aortic root.
Follow-up investigation
Follow-up questionnaires were used, in addition to the following: (I) initial diagnosis date; (II) the echocardiography report, including pmVSD number, size, location, aortic root diameter, and complications of a membranous ventricular septal aneurysm; (III) measurements of height and weight; and (IV) details on complications such as the occurrence of respiratory tract infections, including details on the duration and treatment.
Lower respiratory tract infection score evaluation methods
Lower respiratory tract infections were evaluated by determining pulmonary blood flow. We adopted a semi-quantitative method that recorded respiratory tract infections and developed a scoring system. The scoring rules were: bronchitis, 1 point; pneumonia, 2 points; Killip II heart failure, 1 point, Killip III or IV heart failure, 2 points; and infections lasting > two weeks, 1 point.
Statistics
Data are expressed as mean ± standard deviation. One-way ANOVA was used for statistical analysis where appropriate. A linear regression analysis was used to assess relationships between DVSD/DAR and other measurements. All statistical analyses were performed by software SPSS 17.0, and P<0.05 was considered statistically significant.
Results
Height decreased in the C and D DVSD/DAR ratio groups
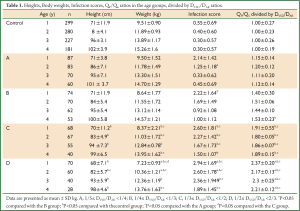
Compared with the control group, the average heights of groups A and B were not different, while heights in groups C and D were decreased for all ages (all P<0.05; Table 1).
Full Table
Body weight decreased in the C and D DVSD/DAR ratio groups
Compared with the control group, the average body weights of groups A and B were not different, while body weights in groups C and D were decreased for all ages (all P<0.05; Table 1). Compared with group C, body weights for group D were lower in the 1 year subgroup (P<0.05).
Respiratory tract infections increased in the C and D DVSD/DAR ratio groups
Compared with the control group, infection scores of groups A and B were significantly increased only in the 1 year age subgroups (both P<0.05; Table 1). Infection scores of each age subgroup of groups C and D were increased (all P<0.05). Moreover, infection scores of group D were higher than group C in the 1 year subgroup (P<0.05).
QP/QS increased in the C and D DVSD/DAR ratio groups
Compared with the control group, QP/QS of each age subgroup were increased as the DVSD/DAR ratio increased (all P<0.05; Table 1). QP/QS of group C and D were higher than group A and group B (both P<0.05; Table 1). Moreover, QP/QS of group D was more than 2.
Relationship between DVSD/DAR ratio and measurements of growth, development, and infection rates
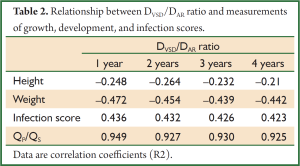
By linear regression analysis, the DVSD/DAR ratio positively correlated with QP/QS and infection scores (Table 2). Further, the DVSD/DAR ratio negatively correlated with height and body weight (Table 2).
Full Table
Discussion
A congenital heart defect is defined as an abnormality in cardiovascular structure or function that is present at birth, even if it is discovered much later (11). Ventricular septal defects represent the most common type and accounts for 25% of all congenital heart disease. Although VSDs can undergo spontaneous postnatal closure, frequent outcomes include growth retardation, recurrent infections, heart failure, and death (12). Ventricular septal defect size is a major factor affecting prognosis and is usually assessed by measuring the diameter of the defect (4). VSD is divided into three types, according to the defect diameter: a small VSD has diameter <5 mm; a medium VSD has diameter ≥5 and <10 mm; and a large VSD has diameter ≥10 mm (13). However using simple VSD diameter to evaluate disease severity has certain shortcomings, due to the effects of age, body weight, defect shape, and defect type. Other methods, including catheterization, determining the VSD area to body surface area ratio, or determining the QP/QS ratio, are either invasive or cumbersome to measure in the clinical practice (5,6). Therefore, it is very important to find a more simple measurement to determine the severity of VSD.
In the present study, height and weight values of each age subgroup were decreased as the DVSD/DAR ratio increased, with the DVSD/DAR ratio negatively correlating with both height and weight. This indicates that the DVSD/DAR ratio reflects the growth condition of children with pmVSD. The DVSD/DAR ratio negatively correlated with pmVSD, regardless of age. This result is similar to a previous study by our team using simple pmVSD size, where we showed that in pmVSD patients, the size of the left-to-right shunt and abnormal hemodynamics in the pulmonary circulation are important factors in the etiology of impaired growth (14). Furthermore, we found that growth condition was not different to the healthy children in pmVSD patients with DVSD/DAR <1/3. The height and weight values of each age subgroup were decreased as the DVSD/DAR ratio increased, with the DVSD/DAR ratio negatively correlating with both height and weight.
Because left ventricular systolic pressure was significantly higher than the right ventricle in VSD, there exists a left-right shunt in ventricular leading to systemic circulation insufficiency and pulmonary circulation congestion (15). Children with VSD not only have limited growth but also have serious pulmonary disease, such as recurrent incidences of infection in the lung. Increasing evidence supports the concept that pulmonary infection condition reflects pulmonary blood flow and susceptibility to infection (16). Accordingly, we studied the relationship between DVSD/DAR ratio and pulmonary infection. Compared with control group, infection scores of groups A and B were significantly increased only in the 1 year age subgroup and were significantly increased in all subgroups in groups C and D. Mechanistically, a large pmVSD is more likely to develop left ventricular-to-right atrial shunt resulting in pulmonary circulation congestion (17).
Linear regression analysis showed that the DVSD/DAR ratio positively correlated with both QP/QS and the infection score. These results suggested that the DVSD/DAR ratio could reflect the pulmonary infection condition. Moreover pulmonary infection scores were not increased in pmVSD patients with DVSD/DAR <1/3, compared with the healthy children. Therefore, pmVSD children with DVSD/DAR <1/3 had no limitations in growth and normal pulmonary health.
The indications for surgical treatment of pmVSD are: age >2 years with QP/QS >2:1 or with infection, growth retardation, or other clinical symptoms (indicating the ineffectiveness of drug therapy). In the present study, in cases of DVSD/DAR <1/3, pmVSD had little effect on growth and QP/QS did not change significantly. In this case, surgical intervention was not necessary and follow-up was given regularly. When 1/2≤ DVSD/DAR <2/3, indicators of growth were significantly decreased and QP/QS was significantly increased. Moreover, the pmVSD was less likely to spontaneously close. Therefore, according to other indicators, selective surgical intervention should be done to reduce the further adverse effects of pmVSD.
In summary, using the DVSD/DAR ratio as a measurement to evaluate pmVSD severity may avoid the drawbacks of measuring the simple defect diameter. Though its reliability and prognosis value need to be further confirmed, we recommend that DVSD/DAR ratio can used as one additional reference index to determine the size of the perimembranous ventricular septal defect.
Study limitations
The potential limitation in this study is the small population sample size. A multicenter trial with larger sample size and longer-term evaluation is warranted to determine if the independent clinical contribution of DVSD/DAR ratio is a sensitive, noninvasive marker of VSD.
Acknowledgements
This study was partly supported by the key grant from the department of science and technology of Jilin Province (20110457).
Disclosure: The authors declare no conflict of interest.
References
- Paladini D, Palmieri S, Lamberti A, et al. Characterization and natural history of ventricular septal defects in the fetus. Ultrasound Obstet Gynecol 2000;16:118-22. [PubMed]
- Miyake T, Shinohara T, Fukuda T, et al. Spontaneous closure of perimembranous ventricular septal defect after school age. Pediatr Int 2008;50:632-5. [PubMed]
- Chen CW, Li CY, Wang JK. Growth and development of children with congenital heart disease. J Adv Nurs 2004;47:260-9. [PubMed]
- van den Heuvel F, Timmers T, Hess J. Morphological, haemodynamic, and clinical variables as predictors for management of isolated ventricular septal defect. Br Heart J 1995;73:49-52. [PubMed]
- Sivakumar K, Anil SR, Rao SG, et al. Closure of muscular ventricular septal defects guided by en face reconstruction and pictorial representation. Ann Thorac Surg 2003;76:158-66. [PubMed]
- Shirali GS, Smith EO, Geva T. Quantitation of echocardiographic predictors of outcome in infants with isolated ventricular septal defect. Am Heart J 1995;130:1228-35. [PubMed]
- Kurotobi S, Sano T, Matsushita T, et al. Quantitative, non-invasive assessment of ventricular septal defect shunt flow by measuring proximal isovelocity surface area on colour Doppler mapping. Heart 1997;78:305-9. [PubMed]
- Mansencal N, Martin F, Farcot JC, et al. Echocardiographic automated cardiac output measurement of pulmonary output and quantification of intracardiac shunt. Int J Cardiol 2005;104:25-31. [PubMed]
- Kosecik M, Sagin-Saylam G, Unal N, et al. Noninvasive assessment of left-to-right shunting in ventricular septal defects by the proximal isovelocity surface area method on Doppler colour flow mapping. Can J Cardiol 2007;23:1049-53. [PubMed]
- Sahn DJ, DeMaria A, Kisslo J, et al. Recommendations regarding quantitation in M-mode echocardiography: results of a survey of echocardiographic measurements. Circulation 1978;58:1072-83. [PubMed]
- Hoffman JI, Kaplan S. The incidence of congenital heart disease. J Am Coll Cardiol 2002;39:1890-900. [PubMed]
- Kleinman CS, Tabibian M, Starc TJ, et al. Spontaneous regression of left ventricular dilation in children with restrictive ventricular septal defects. J Pediatr 2007;150:583-6. [PubMed]
- Axt-Fliedner R, Schwarze A, Smrcek J, et al. Isolated ventricular septal defects detected by color Doppler imaging: evolution during fetal and first year of postnatal life. Ultrasound Obstet Gynecol 2006;27:266-73. [PubMed]
- Manso PH, Carmona F, Jácomo AD, et al. Growth after ventricular septal defect repair: does defect size matter? A 10-year experience. Acta Paediatr 2010;99:1356-60. [PubMed]
- Bhatt M, Roth SJ, Kumar RK, et al. Management of infants with large, unrepaired ventricular septal defects and respiratory infection requiring mechanical ventilation. J Thorac Cardiovasc Surg 2004;127:1466-73. [PubMed]
- Bol Raap G, Meijboom FJ, Kappetein AP, et al. Long-term follow-up and quality of life after closure of ventricular septal defect in adults. Eur J Cardiothorac Surg 2007;32:215-9. [PubMed]
- Wu MH, Wang JK, Lin MT, et al. Ventricular septal defect with secondary left ventricular-to-right atrial shunt is associated with a higher risk for infective endocarditis and a lower late chance of closure. Pediatrics 2006;117:e262-7. [PubMed]


