Minimal access aortic valve replacement via limited skin incision and complete median sternotomy
Introduction
Aortic stenosis (AS) is a degenerative valvular disease that worsens over time. The natural history of AS is well studied with poor prognosis after the onset of angina, syncope, and dyspnea (1,2). Surgical aortic valve replacement (AVR) is an effective and well-established therapeutic strategy for AS with well-recognized guidelines for timing of intervention (3,4). Surgical AVR has typically been performed through a full median sternotomy with excellent outcomes. However, in recent years there has been an increasing impetus to perform minimal access AVR through approaches such as right thoracotomy (5-8), transverse or partial median sternotomies (9-12), and even partial “complex” sternotomies (13-15). Such approaches have been adopted in attempt to lessen surgical trauma and decrease the invasiveness of the surgical intervention. Reported advantages of minimal access AVR include better cosmetic results, less postoperative pain, shorter intensive care unit and hospital stays, shorter ventilation time, decreased blood loss and mortality and morbidity comparable to conventional full sternotomy (16-19). One well-recognized but less practiced surgical technique for surgical AVR is the complete median sternotomy via limited skin incision. This review article provides a detailed insight into the technical aspects, outcomes, pros and cons associated with minimal access AVR via limited skin incision and complete median sternotomy.
Technical aspects
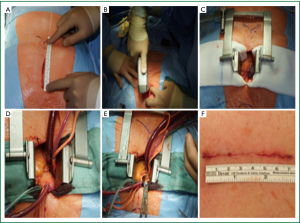
A midline skin incision is started 2 cm below the level of the sternal angle of Louis and extended to a maximum of 3 inches (Figure 1A). The soft tissue over the body and manubrium sterni is undermined to expose the xiphoid process and the suprasternal notch. A complete median sternotomy is performed using either a regular or an oscillating saw (Figure 1B). A Finocchietto retractor is inserted (Figure 1C) and the pericardium is opened through a vertical incision followed by traction sutures to expose the ascending aorta and the right atrial appendage. Two purse-string sutures are placed in the distal ascending aorta, another on the right atrial appendage. Aortic cannulation is performed using a 22 Fr (French) arterial cannula. For venous cannulation a single wire reinforced flat 32/40 Fr two-stage venous cannula is utilized. A DLP® aortic root cannula (Medtronic Inc., USA) inserted in the aortic root proximal to the cross clamp allows for the simultaneous delivery of cardioplegia and aspiration of the aorta and left heart (Figure 1D). Additional left ventricular vent is inserted through the right superior pulmonary vein. Systemic temperature is lowered to 34 °C and cardiac arrest is induced by antegrade cold blood cardioplegia. After aortic cross clamping standard aortotomy is performed (Figure 1E). Thereafter aortic valve replacement is undertaken as it would be in case of a standard median sternotomy with conventional skin incision. At the end of the procedure the sternum is closed with 4 to 5 pairs of 8 to 10 single steel wires depending on the length of the sternum. Soft tissue and skin are approximated with absorbable suture (Figure 1F).
Outcomes
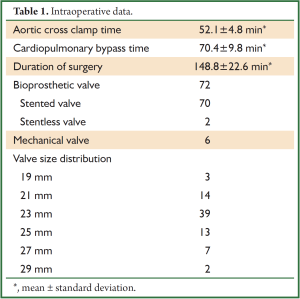
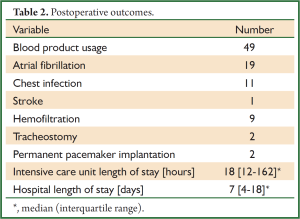
At the authors’ institution since January 2007 surgical AVR via limited skin incision and complete median sternotomy has been performed in 78 patients. The operation has been predominantly offered to octogenarians (56/78) and young female (20/78) as well as adolescent male patients (2/78). Hemodynamic lesions included stenosis (60/78), regurgitation (14/78) and mixed disease (4/78). Bioprosthetic valves were implanted in 72 patients while 6 patients received a mechanical valve. Valves ranging from size 19-29 mm were implanted (Table 1). Aortic root enlargement using a bovine pericardial patch was performed in 8 patients. Other intraoperative variables are presented in Table 1. All patients had uneventful surgery with satisfactory postoperative recovery. 30-day mortality was 0% and 1 patient experienced stroke with right sided hemiparesis which improved significantly at 12 months follow-up. Postoperative clinical outcomes are listed in Table 2. Intraoperative transesophageal echocardiography confirmed well seated prosthetic valves with no paravalvular leakage in any of the patients. At a mean follow-up of 2.4±1.1 years no reoperation due to prosthetic valve endocarditis or structural valve degeneration had to be done. Two patients required permanent pacemaker implantation and no sternal dehiscence or wound infection occurred during the follow-up. Similar outcomes have been reported by Alassar et al. (20) and Luciani and Mazzucco (21).
Full Table
Full Table
Advantages & disadvantages
Over the past two decades minimal access cardiac surgery has been increasingly adopted with a view to reducing the invasiveness of the surgical procedures. The predominant perception leading to enhanced interest in minimal access cardiac surgery is that smaller incisions and limited dissection may abolish intraoperative trauma and complications, thereby accelerating postoperative recovery and minimizing procedure-related costs. Furthermore, smaller surgical scars and more rapid recovery enhance patient satisfaction. Interestingly, evidence from randomized controlled trials as well as meta-analysis has failed to show a convincing superiority of minimally invasive AVR over conventional AVR (17,22,23). At the same time, most commonly reported minimal access approaches for AVR share greater potential for sternal stump dehiscence, instability, overriding, and fracture. The risk for sternal instability may be more pronounced in cases where emergency conversion from partial to complete sternotomy is required leading to complex sternal fractures.
We have adopted the full sternotomy via limited skin incision approach as a preferred approach for minimal access AVR in octogenarians and young females as in our experience, similar that of others (20,21), the cosmetic result is comparable to that of a partial sternotomy while the exposure is superior to that afforded by partial sternotomy. Moreover, there is no need for special surgical instruments to obtain this access. Additional advantages include ease of conversion to conventional approach by extending the limited skin incision, similar closure technique as for traditional full median sternotomy, and avoidance of femoral vessels cannulation thereby preventing groin complications.
In octogenarians this approach reduces the operative time (20). The median sternotomy ensures symmetric retraction of the sternum, resulting in enhanced exposure of the heart and great vessels thereby facilitating cannulation, cross-clamping, native valve excision, prosthetic valve implantation and suturing of the aortotomy. Smooth conduct of operation without struggle translates into shorter operative time with subsequent improved outcomes in octogenarians in whom shorter operative time correlates strongly with faster recovery.
For females the skin incision for this approach offers the best cosmetic result as it commences 2 cm below the sterna angle of Louis which means that the upper part of the scar is hardly visible even with clothes with low neck line.
Perhaps the only limitation of this approach is the risk of sternal instability which is usually a reflection of poor technique of sternal closure. However, in our experience as well as that of Alassar and associates (20) sternal dehiscence or sternal wound infection has not been encountered.
Conclusions
Full sternotomy via limited skin incision approach for minimal access AVR is a safe and effective strategy. This approach provides the “best of both worlds” by combining the cosmetic benefit of a limited skin incision with the advantages of a complete median sternotomy. However, it is disappointingly underutilized. With increasing numbers of octogenarians being referred for surgical AVR this approach could be preferentially offered to this high-risk group of patients with the potential of expedited recovery and low-cost without unnecessarily enhancing the risk of surgery.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Carabello BA, Paulus WJ. Aortic stenosis. Lancet 2009;373:956-66. [PubMed]
- Schwarz F, Baumann P, Manthey J, et al. Circulation 1982;66:1105-10. [PubMed]
- Bonow RO, Carabello BA, Chatterjee K, et al. 2008 focused update incorporated into the ACC/AHA 2006 guidelines for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to revise the 1998 guidelines for the management of patients with valvular heart disease). Endorsed by the Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. J Am Coll Cardiol 2008;52:e1-142. [PubMed]
- Vahanian A, Alfieri O, Andreotti F, et al. Guidelines on the management of valvular heart disease (version 2012): the Joint Task Force on the Management of Valvular Heart Disease of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS). Eur J Cardiothorac Surg 2012;42:S1-44. [PubMed]
- Cosgrove DM 3rd, Sabik JF. Minimally invasive approach for aortic valve operations. Ann Thorac Surg 1996;62:596-7. [PubMed]
- Minale C, Reifschneider HJ, Schmitz E, et al. Single access for minimally invasive aortic valve replacement. Ann Thorac Surg 1997;64:120-3. [PubMed]
- Benetti FJ, Mariani MA, Rizzardi JL, et al. Minimally invasive aortic valve replacement. J Thorac Cardiovasc Surg 1997;113:806-7. [PubMed]
- Lazzara RR, Kidwell FE. Right parasternal incision: a uniform minimally invasive approach for valve operations. Ann Thorac Surg 1998;65:271-2. [PubMed]
- Svensson LG. Minimal-access “J” or “j” sternotomy for valvular, aortic, and coronary operations or reoperations. Ann Thorac Surg 1997;64:1501-3. [PubMed]
- Gundry SR, Shattuck OH, Razzouk AJ, et al. Facile minimally invasive cardiac surgery via ministernotomy. Ann Thorac Surg 1998;65:1100-4. [PubMed]
- Kasegawa H, Shimokawa T, Matsushita Y, et al. Right-sided partial sternotomy for minimally invasive valve operation: “open door method Ann Thorac Surg 1998;65:569-70. [PubMed]
- Tam RK, Almeida AA. Minimally invasive aortic valve replacement via partial sternotomy. Ann Thorac Surg 1998;65:275-6. [PubMed]
- Nair RU, Sharpe DA. Minimally invasive reversed Z sternotomy for aortic valve replacement. Ann Thorac Surg 1998;65:1165-6. [PubMed]
- Doty DB, DiRusso GB, Doty JR. Full-spectrum cardiac surgery through a minimal incision: mini-sternotomy (lower half) technique. Ann Thorac Surg 1998;65:573-7. [PubMed]
- Moreno-Cabral RJ. Mini-T sternotomy for cardiac operations. J Thorac Cardiovasc Surg 1997;113:810-1. [PubMed]
- von Segesser LK, Westaby S, Pomar J, et al. Less invasive aortic valve surgery: rationale and technique. Eur J Cardiothorac Surg 1999;15:781-5. [PubMed]
- Bonacchi M, Prifti E, Giunti G, et al. Does ministernotomy improve postoperative outcome in aortic valve operation? A prospective randomized study. Ann Thorac Surg 2002;73:460-5. [PubMed]
- Tabata M, Umakanthan R, Cohn LH, et al. Early and late outcomes of 1000 minimally invasive aortic valve operations. Eur J Cardiothorac Surg 2008;33:537-41. [PubMed]
- Doll N, Borger MA, Hain J, et al. Minimal access aortic valve replacement: effects on morbidity and resource utilization. Ann Thorac Surg 2002;74:S1318-22. [PubMed]
- Alassar Y, Yildirim Y, Pecha S, et al. Minimal access median sternotomy for aortic valve replacement in elderly patients. J Cardiothorac Surg 2013;8:103. [PubMed]
- Luciani GB, Mazzucco A. Aortic valve replacement via minimal-access complete sternotomy. Tex Heart Inst J 2000;27:286-8. [PubMed]
- Dogan S, Dzemali O, Wimmer-Greinecker G, et al. Minimally invasive versus conventional aortic valve replacement: a prospective randomized trial. J Heart Valve Dis 2003;12:76-80. [PubMed]
- Murtuza B, Pepper JR, Stanbridge RD, et al. Minimal access aortic valve replacement: is it worth it? Ann Thorac Surg 2008;85:1121-31. [PubMed]


