Comparison of video-assisted thoracic surgery with open surgery in the treatment of ectopic mediastinal parathyroid tumors
Introduction
The mediastinal parathyroid is defined as a parathyroid found completely below the level of the clavicle, which included adenoma, adenocarcinoma and hyperplasia. The mediastinal parathyroid adenoma (MPA) was firstly described by Churchill in 1932 (1). During the process of embryonic development, the ectopic parathyroid gland was formed due to the arrest of descent process of thymus and parathyroid gland. The ectopic parathyroid gland is usually found in the neck; however, the mediastinal parathyroid tumor accompanied with hyperparathyroidism is rarely reported (2-4). The incidence of ectopic mediastinal parathyroid was reported to be in the range of 6% to 16% (5,6). In the current study, the ectopic mediastinal parathyroid tumors treated by surgeries in Shanghai Ruijin Hospital within recent 20 years were collected and retrospectively analyzed, including both surgical procedures and pathological studies.
Methods
This study included 21 cases of patients (13 males and 8 females) who were diagnosed with ectopic mediastinal parathyroid tumors and treated with surgical resection from May 1995 to May 2015 in Ruijin Hospital, Shanghai Jiao Tong University School of Medicine. Written informed consent was obtained from all the patients for clinical data collection and accompanying images, as well as potential publication. All the patients underwent the examination of blood calcium, blood phosphorus and PTH before and after surgery. The location of the tumors was examined by computed tomography (CT), magnetic resonance imaging (MRI), or Technetium-99m sestamibi scanning (99mTc-MIBI). Technetium-99m sestamibi scanning is considered the gold standard for clinical location. Ectopic mediastinal parathyroid tumors were finally confirmed by post-operational pathology. After surgery, all the patients followed up at least every three months till one year post-operation.
Statistical analysis
The software SPSS13.0 was utilized for statistical analysis. The measurement data was analyzed by t-test and the count data was analyzed by χ2 test.
Results
Clinical information
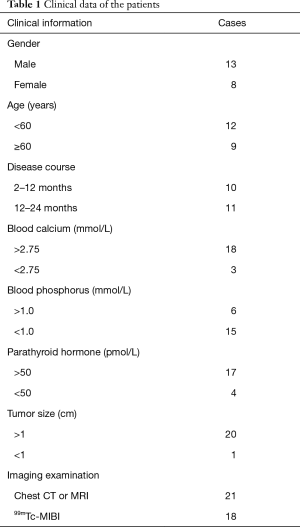
Twenty-one patients were firstly found hypercalcemia by physical examination without any specific symptoms, and were considered ectopic parathyroid tumors after diagnosis by Endocrinology Department. The clinical data includes demographic data, blood calcium, blood phosphorus, PTH and imaging examination. In our study, all the patients were found accompanied with high concentration of PTH, including 17 cases with a concentration of PTH >50 pmol/L. However, concerning blood calcium,
Eighteen cases in 21 were found hypercalcemia (>2.75 mmol/L), compared to 3 cases with normal blood calcium, as shown in Table 1. Among the 21 patients, 9 cases underwent video-assisted thoracic surgery (VATS), 13 cases (including one secondary open operation after VATS) underwent open surgery.
Full table
Localization and pathological diagnosis of ectopic mediastinal parathyroid tumor
There were 15 ectopic parathyroid tumors located in the front superior part of mediastinum, including 12 cases at posterior of sternum, 1 within thymus and 2 besides of thymus. There were 6 located in the middle part of mediastinum, including 2 at front superior of venae anonyma, 1 at posterior of venae anonyma and left posterior of arteriae anonyma, 1 at superior of aortic arch, 1 at right posterior of aortic arch, 1 at inferior of aortic arch, and 1 at front of ascending aorta. All 21 cases of mediastinal parathyroid tumor were confirmed by pathological study, including 16 cases of parathyroid adenoma (76.2%), 4 cases of parathyroid hyperplasia (19.0%), and only 1 case of parathyroid adenocarcinoma (4.8%).
Postoperative blood calcium
The blood calcium was examined at the first day after operation and found decreased in all 21 patients, 17 of which had blood calcium decreased and maintained at normal level by respective measurement at 1-week and 1-month postoperative. The hypocalcemia (1.80 mmol/L) was found in 1 patient at the first day after operation, and the blood calcium restored to normal range 2 days later. The blood calcium was found decreased in 3 patients after operation, but still exceeded the normal range within first postoperative week (two patients were found decreased to normal range 1-month postoperative, and another patient underwent secondary operation for hypercalcemia).
Surgery procedures
The therapeutic effects of VATS (n=8) and chest open surgery (n=12) were compared (Table 2). One patient who received secondary open chest operation after VATS was excluded. For open surgery, in order to obtain a better exposure field, median sternotomy was performed in 13 cases (Figure 1A). While regarding to minimally invasive surgeries, bi-portal approach was adopted: the observation hole was positioned at the 6th intercostal spaces of axillary midline and the operation hole was positioned at the 4th intercostal spaces of the anterior axillary line, as is shown in Figure 1B. Tumor and adjacent fat tissue were completely resected and carefully intraoperative examined by the operator.
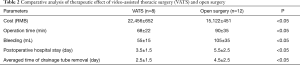
Full table

In contrast to conventional open surgery, the cost of VATS was relatively higher; however, VATS was superior to open surgery in many aspects such as shorter averaged operation time, less intraoperative bleeding amount, shorter postoperative hospital stay, and quicker averaged time of drainage tube removal (P<0.05; Table 2).
Discussion
Primary hyperparathyroidism (PTH) was the major cause for hypercalcemia in clinical (7). The over secretion of PTH by parathyroid could lead to general bone absorption and decalcification, with the consequence of a serial symptoms involved bone, urine system, nerve system, psychology, and digestive system. Around 80% PTH was caused by parathyroid tumors (8). It was reported that the descending process of parathyroid and thymus was arrested during embryonic development, and remained at the carotid sheath, between trachea and esophagus, suprasternal fossae, or close to thymus, to form an ectopic parathyroid. Currently, the surgical removal was considered the most effective therapy for ectopic parathyroid. It was reported that surgeries were not only effective for patients with symptoms but also effective for patients without overt symptom but accompanied with increased blood calcium (>0.25 mol/L), decreased creatinine clearance rate (<60 mL/min), or bone density less than −1.0 (9).
The recurrence rate of ectopic mediastinal parathyroid with hyperparathyroidism was high by pure simple investigation surgery, and the secondary operation to remove tumor tissues was usually needed (10). Therefore, the accurate localization by preoperative imaging was very critical for the success of the treatment. The diagnosis and localization of parathyroid tumor could be accomplished by chest CT; and 99Tc-MIBI imaging has been considered as golden standard for localization of parathyroid tumor due to its high sensitivity. The selection of surgery mode should be based on the chest CT and imaging analysis; and the current study also suggested the chest CT and 99mTc-MIBI were the effective and reliable diagnostic methods. The conventional surgeries included chest open surgery (intercostal incision and sternum middle incision) and thoracoscopic operation with the major objective to remove functional parathyroid tumor tissues. Our findings indicated that thoracoscopic operation had equivalent therapeutic effect compared with open surgery, meanwhile the operation time was significantly decreased and postoperative recovery was more rapid. The robot operation has been also carried out for ectopic parathyroid tumor (11-13), with the equivalent long-term therapeutic effect compared with conventional operations. However, the high cost of robot operation has been the major hurdle for widely utilization.
In the current study, the adenoma was the major type (76.2%) of ectopic parathyroid tumor. And the surgical treatment was demonstrated to be an effective method especially for patients accompanied with hypercalcemia. The blood calcium was significantly decreased after removal of functional tumor tissues, and the blood calcium restored to the normal range in all the patients within three days after surgeries. The incidence of ectopic mediastinal parathyroid was relatively low, and the front part of mediastinum was the position for parathyroid tumor more commonly. Given the satisfied therapeutic outcome of surgery, once the ectopic mediastinal parathyroid tumor was confirmed, the surgery was recommended to perform timely, especially the micro invasive thoracoscopy.
However, for the small tumor less than 1 cm, the thoracoscopic operation might be failed or lead to tumor residue due to inaccurate localization, which could be ascribed to the less tangible sensitivity of thoracoscopy compared with figures. In the current study, there was one woman with tumor size less than 1.0 cm, and the secondary open surgery had to be carried out because the incomplete removal of tumor by thoracoscopy. Therefore, it was suggested by the current study that the thoracoscopic operation should be carefully considered for small ectopic mediastinal tumor; the tumor with difficulty in the locating should be removed after the thorough removal of fat tissues around thymus, in order to complete dissection to ensure the therapeutic effect and avoid the secondary operation. In the past 20 years, with the progress of medical techniques, VATS (even robotic-assisted surgery) has been increasingly used in different surgical fields including thoracic surgery. Valsecchi and colleagues considered that VATS and medical thoracoscopy (MT) should have their own clinical indications and be performed by different specialists in the same medical center (14). Recently, it has also been reported that radio-guided detection techniques were developed for surgical treatment of parathyroid adenomas. The MIRP (minimally invasive radio-guided parathyroidectomy) technique allows a low dose (1 mCi) of Tc-99m MIBI without intraoperative PTH assay and frozen section analysis leading to excellent cure rate for PHPT (15).
In conclusion, adenoma is the major pathological type of ectopic mediastinal parathyroid tumors, and the correct diagnosis with precise preoperative location was the keys for the treatment of ectopic mediastinal parathyroid tumors accompanied with hyperparathyroidism. The surgical treatment was demonstrated to be an effective therapy with satisfied therapeutic outcome, especially for VATS due to its clinical advantages.
Acknowledgements
Funding: This study was supported by the grant from Science and Technology Commission of Shanghai Municipality Medical Guidance Science & Technology Support Project (16411966100).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by Institutional Ruijin Hospital Ethics Committee Shanghai Jiao Tong University School of Medicine (No. 2017139). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Bauer W, Federman DD. Hyperparathyroidism epitomized: the case of Captain Charles E Martell. Metabolism 1962;11:21-9. [PubMed]
- Kim YS, Kim J, Shin S. Thoracoscopic removal of ectopic mediastinal parathyroid adenoma. Korean J Thorac Cardiovasc Surg 2014;47:317-9. [Crossref] [PubMed]
- Di Cosimo C, Metere A, Chiesa C, et al. Mediastinal parathyroid adenoma: a case report. Eur Rev Med Pharmacol Sci 2012;16:845-7. [PubMed]
- Gratian LF, Hyland KA, Scheri RP. Hyperparathyroid crisis due to asymmetric parathyroid hyperplasia with a massive ectopic. Endocr Pract 2014;20:e180-2. [Crossref] [PubMed]
- Phitayakorn R, McHenry CR. Incidence and location of ectopic abnormal parathyroid glands. Am J Surg 2006;191:418-23. [Crossref] [PubMed]
- Hamidi S, Soltani A, Hedayat A, et al. Primary hyperparathyroidism: A review of 177 cases. Med Sci Monit 2006;12:CR86-9. [PubMed]
- Liman ST, Topcu S, Dervisoglu E, et al. Excision of ectopic mediastinal parathyroid adenoma via parasternal videomediastinoscopy. Ann Thorac Cardiovasc Surg 2014;20:67-9. [Crossref] [PubMed]
- Dong JY, Guan Y, Zhu Y, et al. Surgical treatment of 368 cases of hyperthyroidism. Chin J Gen Surg 2011;4:289-91.
- Kim YS, Kim J, Shin S. Thoracoscopic Removal of Ectopic Mediastinal Parathyroid Adenoma. Korean J Thorac Cardiovasc Surg 2014;47:317-9. [Crossref] [PubMed]
- van Heerden JA, Grant CS. Surgical treatment of primary hyperparathyroidism: an institutional perspective. World J Surg 1991;15:688-92. [Crossref] [PubMed]
- Harvey A, Bohacek L, Neumann D, et al. Robotic thoracoscopic mediastinal parathyroidectomy for persistent hyperparathyroidism: case report and review of the literature. Surg Laparosc Endosc Percutan Tech 2011;21:e24-7. [Crossref] [PubMed]
- Ismail M, Maza S, Swierzy M, et al. Resection of ectopic mediastinal parathyroid glands with the da Vinci robotic system. Br J Surg 2010;97:337-43. [Crossref] [PubMed]
- Profanter C, Schmid T, Prommegger R, et al. Robot-assisted mediastinal parathyroidectomy. Surg Endosc 2004;18:868-70. [Crossref] [PubMed]
- Valsecchi A, Arondi S, Marchetti G. Medical thoracoscopy: Analysis on diagnostic yield through 30 years of experience. Ann Thorac Med 2016;11:177-82. [Crossref] [PubMed]
- Mehrabibahar M, Mousavi Z, Sadeghi R, et al. Feasibility and safety of minimally invasive radioguided parathyroidectomy using very low intraoperative dose of Tc-99m MIBI. Int J Surg 2017;39:229-33. [Crossref] [PubMed]


