“Five on a dice” port placement for robot-assisted thoracoscopic right upper lobectomy using robotic stapler
Introduction
Robotic surgery has quickly established its role as a viable technique in thoracic surgery. One of the major barriers to easily adopting robot-assisted lobectomy with earlier versions of the da Vinci robot system (S, Si, Intuitive Surgical, Sunnyvale, CA) has been the lack of a curved tip vascular stapler that can be controlled by the operating surgeon at the surgical console to divide the pulmonary artery and the pulmonary vein. As a result, each procedure required the presence of a trained bedside assistant whose role included placing, manipulating, and firing the stapler around a major vascular structure (1-7). In other words, the most experienced person in the operating room would not perform the most dangerous part of the operation. These undesirable operating conditions can be avoided by having a second surgeon as the bedside assistant, but it is impractical to routinely have two surgeons available to perform a lung resection. Another option is to have the operating surgeon leave the console to scrub in to perform the stapling while the robot is left unattended. These alternatives are not ideal for wide adoption of robotic technology.
The new version of the da Vinci robot (Xi) addresses this major issue with a robot-controlled curved tip vascular stapler that allows the surgeon to have complete control of the operation. In order to fully take advantage of the robot’s capability, we postulate that we can develop a port placement strategy that allows for passive assistance during the right upper lobectomy. In this report, we show that a “five on a dice” port placement allows for an ergonomic retraction of the lung and easy division of any hilar structures using robot staplers. This method requires only passive assistance to the surgeon by the bedside assistant such as specimen retrieval and instrument exchange, as opposed to active assistance that requires manipulating and retracting lung tissue or by placing a stapler around a critical vascular structure.
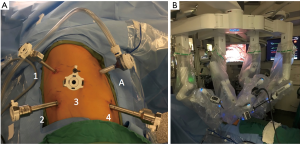
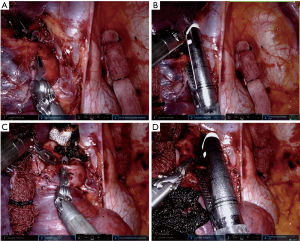
Operative techniques—robot right upper lobectomy (Figure 1)

“Five on a dice” port placement
- Place a 5-mm port by the tip of the scapula in the 7th intercostal space using the Xcel trocar under direct vision with a 5-mm 0-degree thoracoscope. Insufflate the chest to a pressure of 10 mmHg using the Airseal system (Conmed, Utica, NY). Communicate with the anesthesia team that you are insufflating the chest and to watch for hemodynamic changes;
- Place a 12-mm robot port in the 7th intercostal space in the mid-axillary line (Figure 2A, “4”);
- Place an 8-mm robot port in the 7th intercostal space between the first two ports (Figure 2A, “3”);
- Place a 12-mm robot port in the 9th intercostal space along the tip of the scapula (Figure 2A, “2”);
- Exchange the 5-mm port by the tip of the scapula to an 8-mm robot port (Figure 2A, “1”);
- Place a 12-mm Airseal port in the 4th intercostal space in the mid-axillary line as the assistant port (Figure 2A, “A”). This port was used to provide insufflation in the chest to 10 mmHg using CO2 and provide assistant to retrieve lymph node packets and suction under direct vision;
- Dock the Xi robot so that ports 1, 3, and 4 are in line with 7th intercostal space ports (Figure 2B);
- Insert two tightly rolled raytec sponges tied with a silk suture;
- Place the camera in port 3, the curved bipolar grasper in port 4, the cadiere forceps in port 2 and the tip up fenestrated grasper in port 1.
Overall concept of dissection and division of hilar structures
- Use the tip up fenestrated grasper with a sponge for retraction. Grab the lung parenchyma sparingly;
- Push forward to expose the posterior hilar structures (Figure 3A,B);
- Pull back to expose the anterior hilar structures (Figure 3C);
- Pull down to expose the superior hilar structures (Figure 3D);
- Lift up to expose the inferior hilar structure.
- Always have a camera in arm 3;
- Use the cadiere and curved bipolar grasper or long bipolar grasper in arm 2 or 4 for dissection;
- Place the stapler through port 2 or 4 to divide the hilar structures.
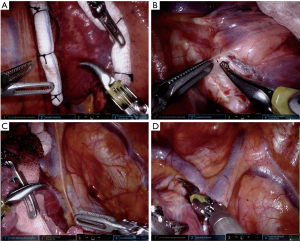
Inferior pulmonary ligament and station 9 lymph node
- Use the tip up fenestrated grasper with a sponge to lift the lung to expose the inferior pulmonary ligament;
- Use the cadiere to lift the ligament and use the bipolar grasper to divide to the inferior pulmonary vein;
- Remove the station 9 lymph node. Place it in a gloved finger that is cut at the tip and request an assistant to remove the specimen from the assistant port.
Posterior hilar dissection and station 7 lymph node
- Use the tip up fenestrated grasper with a sponge to push the lung forward to expose the posterior hilar structures;
- Lift the pleura overlying the inferior pulmonary vein and divide the posterior hilum. Continue until the bronchus intermedius and the right upper lobe bronchus are exposed;
- Remove the station 7 lymph node packet (Figure 4A,B).
Station 4 lymph node
- Remove the lymph node from station 4R using the cadiere in port 1 and the bipolar grasper in port 4 (Figure 4C).
- Remove the lymph node through the assistant port (Figure 4D).
Anterior and superior hilar dissection
- Use the tip up fenestrated grasper with a sponge to pull the lung backward to expose the anterior hilar structures;
- Identify the superior pulmonary vein and dissect below the vessel. Use the cadiere in port 4 and the bipolar grasper in port 2. Lift the tissue over the vessel, carefully dissect bluntly, and then divide the pleura with the bipolar grasper;
- Carry the dissection to the superior hilum;
- Use the tip up fenestrated grasper with a sponge to pull the lung downward to expose the superior hilar structures;
- Connect the anterior and posterior hilar dissections.
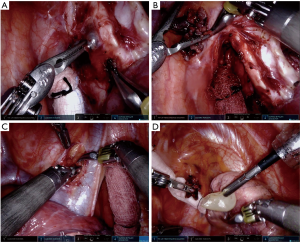
Right upper lobe branches of superior pulmonary vein
- Use the tip up fenestrated grasper with a sponge to pull the lung backward to expose the superior pulmonary vein;
- Dissect with cadieres in port 2 and port 4. Perform blunt dissection from the top and bottom. Once there is adequate dissection, use the tip up fenestrated grasper in port 2 to go around the right upper lobe branches of the superior pulmonary vein and retract with the cadiere on sponge in port 1 (Figure 5A-C);
- Place the white load curve tip 30-mm robot vascular stapler in port 2 and divide the vein. After the stapler is around the vessel, relax the retraction prior to clamping and firing the stapler (Figure 5D).
Truncus anterior pulmonary artery
- Use the cadiere with a sponge to pull the lung down to expose the truncus anterior;
- Place the cadiere in port 2 and the bipolar grasper in port 4. Dissect the tissue overlying the pulmonary artery. With the cadiere spread underneath the tissue, divide the tissue with the bipolar grasper. Dissect the entry and exit point;
- Place the tip up fenestrated grasper in the port 4 and go around the truncus anterior (Figure 6A);
- Place the white load curve tip 30-mm robot vascular stapler in port 4 and divide the truncus anterior pulmonary artery branch (Figure 6B).
Posterior ascending pulmonary artery
- Use the cadiere with a sponge to pull the lung posteriorly and down to expose the rest of the pulmonary artery;
- Carefully dissect between the pulmonary artery and right upper lobe bronchus on the pulmonary artery to find the posterior ascending pulmonary artery branch (Figure 6C);
- Place the white load curve tip 30-mm robot vascular stapler in port 4 and divide the posterior ascending pulmonary artery branch (Figure 6D);
- If the pulmonary artery is too small for a stapler, place a 3-0 silk suture around it, tie it robotically, and divide the specimen side with the robot vessel sealer.
Posterior fissure
- Release the lung from retraction;
- Grab the right lower lobe with a cadiere from port 4 and the right upper lobe with a cadiere from port 1;
- Place the blue load 45-mm stapler from port 2 and divide the lateral aspect of the posterior fissure.
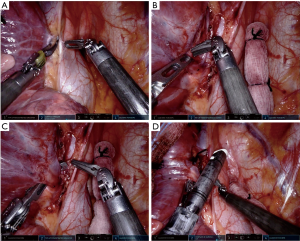
Right upper lobe bronchus
- Hold the right upper lobe bronchus with the cadiere from port 1;
- Remove the lymph node at the right upper lobe and right bronchus intermedius interface. Go around the right upper lobe bronchus with the tip up fenestrated grasper from port 4 (Figure 7A);
- Place the green load curve tip 30-mm robot stapler in port 4 and divide the right upper lobe bronchus (Figure 7B).
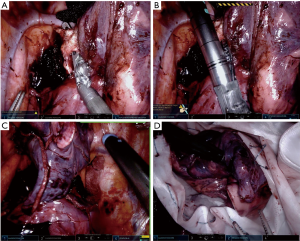
Anterior fissure and lung
- Release the lung from retraction;
- Hold the right upper lobe with the cadiere from port 1 and the right middle lobe with the cadiere from port 2;
- Place the blue load 45-mm robot stapler in port 4 and divide the anterior fissure, medial portion of the posterior fissure (Figure 7C);
- Place the lung in a Cook bag for retrieval (Figure 7D).
Removal of right upper lobe lung
- Place the right upper lobe lung in a Cook bag (Figure 7C,D);
- Enlarge the 7th intercostal space mid axillary line port (Figure 2A, “4”) to 3–4 cm to remove the Cook bag from the right upper lobe lung.
Comments
This technique fully utilizes the da Vinci Xi’s capabilities in a minimally invasive lobectomy. Unlike performing a lobectomy using the da Vinci S and Si platforms or video-assisted thoracoscopic surgery (VATS) in which a skilled assistant is needed for active assistance, the da Vinci Xi and its instrumentation allow for an assistant to provide only passive assistance, such as specimen removal and suctioning. All of this can be done under direct vision since the assistant port is placed in the 4th intercostal space. In VATS lobectomy, as well as some techniques using the S and Si platform, the assistant may be asked to retract the lung from the hilum, to dissect around the hilar structures, and to use blunt dissection to expose the vessel. In contrast, our technique highlights retracting the lung with a sponge and dissecting around the hilar structure by picking up the tissue on top of the vessel. This utilizes the robot’s 10× magnification and fine control that makes this seemingly difficult procedure much easier. Moreover, it allows surgeons to reach the plane of Leriche faster and with minimal blood loss since the bipolar grasper is used to divide the tissue on top of the vessel. This dissection is possible for all of the vessels due to the location of ports 2 and 4 and allows surgeons to easily place the stapler around the hilar structures. While we describe a right upper lobectomy in this paper, we have adopted this port placement and technique for all pulmonary resections.
Overall, the “five on a dice” port placement allows for the full use of the Xi robot’s capabilities to make the robot-assisted lobectomy a safer and more ergonomic operation.
Acknowledgements
We thank Ann Saikin for language editing of the manuscript.
Footnote
Conflicts of Interest: MP Kim and EY Chan have consulted for Olympus, Medtronic and Boston Scientific.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Cerfolio RJ, Bryant AS, Skylizard L, et al. Initial consecutive experience of completely portal robotic pulmonary resection with 4 arms. J Thorac Cardiovasc Surg 2011;142:740-6. [Crossref] [PubMed]
- Park BJ. A complete video-atlas of five robotic-assisted lobectomies. Ann Cardiothorac Surg 2012;1:100-1. [PubMed]
- Park BJ, Flores RM, Rusch VW. Robotic assistance for video-assisted thoracic surgical lobectomy: technique and initial results. J Thorac Cardiovasc Surg 2006;131:54-9. [Crossref] [PubMed]
- Cerfolio RJ. Total port approach for robotic lobectomy. Thorac Surg Clin 2014;24:151-6. v. [Crossref] [PubMed]
- Cerfolio RJ, Bryant AS. Robotic-assisted pulmonary resection - Right upper lobectomy. Ann Cardiothorac Surg 2012;1:77-85. [PubMed]
- Wei B, Eldaif SM, Cerfolio RJ. Robotic Lung Resection for Non-Small Cell Lung Cancer. Surg Oncol Clin N Am 2016;25:515-31. [Crossref] [PubMed]
- Dylewski MR, Ohaeto AC, Pereira JF. Pulmonary resection using a total endoscopic robotic video-assisted approach. Semin Thorac Cardiovasc Surg 2011;23:36-42. [Crossref] [PubMed]
- Kim MP, Chan EY. “Five on a dice” port placement for robot-assisted thoracoscopic right upper lobectomy using robotic stapler. Asvide 2017;4:582. Available online: http://www.asvide.com/articles/1907


