Radical resection of upper right lung under thoracoscopic guidance
Clinical data
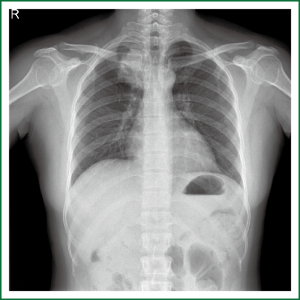
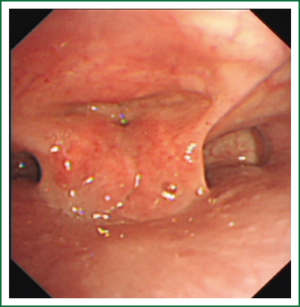
The patient is a 42-year-old woman born in Jieyang, Guangdong, who was admitted for chest tightness and cough for more than three months. Chest CT examinations at the local hospital showed a right upper lung mass in a diameter of about 6 cm. Physical examination revealed: weak breath sounds at the right upper lung, and otherwise healthy. Chest X-ray (Figure 1) showed: a mass of about 6 cm × 4 cm in size in the apical segment of right upper lung. Preoperative CT examination was conducted in the other hospital, for which electronic image was not available. Bronchoscopy (Figure 2) suggested: narrowed opening of the apical segment of right upper lung due to external pressure; cancer cells were found after lavage and brush biopsy. Cranial MR, abdominal ultrasound, whole body bone scan and other tests revealed no signs of distant metastases. Functions of important organs (heart, lung, liver, kidney, brain, etc.) were normal. The patient was otherwise healthy without a history of any specific disease.
Preoperative assessment
Justification for surgery: preoperative bronchoscopy revealed adenocarcinoma cells with a definite diagnosis. The preoperative clinical stage was cT2NxM0, suggesting definite surgical indication. Preoperative pulmonary function tests showed good ventilation and ventilatory functions. Other tests revealed no contraindications to surgery.
Feasibility of surgery: despite a large diameter, the tumor was a peripheral mass. Bronchoscopy suggested narrowed opening of the apical segment of right upper lung due to external pressure, but there was no sign of tumor invasion of the right upper lobe bronchus. Therefore, lobectomy was feasible.
Choice of surgical approach: despite a large diameter, the tumor was a peripheral mass, which was operable laparoscopically. Due to the difficulty in retrieving the specimen, however, smashing before removal of the tumor was not advisable. As a result, the working port was appropriately enlarged (to 5-6 cm). Conversion to small-incision or even traditional incision surgery could be considered according to the specific circumstances during surgery.
Anesthesia and positioning
General anesthesia was delivered with tracheal intubation while the patient was in the left lateral decubitus position.
Operation (Video 1)
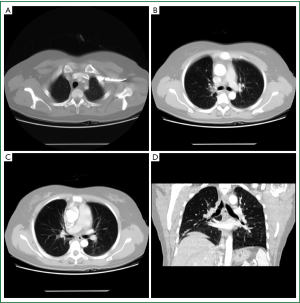
A conventional 3-port approach was taken at the right chest (Figure 3). An approximately 1.5-cm observation port was created in the 7th intercostal space at the middle axillary line, an approximately 5-cm working port in the 4th intercostal space at the anterior axillary line, and an approximately 2-cm auxiliary port in the 8th intercostal space between the posterior axillary and subscapularis lines. Exploration into the chest revealed no pleural adhesion or pleural effusion. The mass was at the apical segment of the right upper lobe, in a diameter of 5 to 6 cm, with the margin being about 3 cm from the beginning of the pulmonary artery at the posterior apical segment. The mediastinal pleura anterior to the hilum were first divided to reveal and separate the superior right pulmonary vein, which was then transected. When dividing and transecting the posterior segment of the superior right pulmonary artery, due to the size of the tumor, the surgical field was difficult to be exposed, leaving a limited length for the division and narrow space for the operation. Hence, careful and gentle operation was needed when handling the stapler. Upon completion of the vascular treatment, the interlobular fissures and bronchi were taken care of. The patient had poorly differentiated fissures, so we used to a tunnel method, in which the lung tissue was divided along from the intersection between the horizontal and oblique fissures until the pulmonary artery, and tunnels were created from the upper part of the pulmonary artery towards the anterior and posterior directions, which were then separately transected. This procedure demanded delicate operation and sophisticated anatomical understanding. After the fissures were separated, the right upper bronchus was exposed and divided. The surrounding lymph nodes were dissected, and the bronchus was transected. Mediastinal lymph node dissection mainly involved the 2, 3, 4 and 7 groups.
The anesthesia time was 160 minutes, the operative time 125 minutes.
Postoperative management
With smooth extubation in 30 minutes after surgery, the patient manifested good spontaneous breathing. A repeat chest X-ray test showed good lung re-expansion. Oxygenation, airway management, prevention of infection and other routine treatment were prescribed postoperatively.
Postoperative pathology
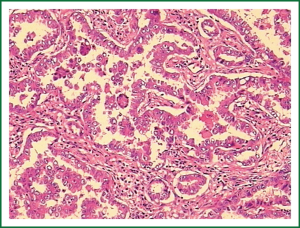
Highly differentiated adenocarcinoma, two metastatic nodes among the hilar lymph nodes, and no metastasis were found in other groups (Figure 4). Postoperative staging: the preoperative stage was T2N1M0, II B.
Follow-up treatment
The patient recovered smoothly without any complications, and was discharged eight days after surgery. Four cycles of chemotherapy (paclitaxel + cisplatin) were administered uneventfully. Chest CT scan (Figure 5) four months after surgery showed: no enlargement of mediastinal and hilar lymph nodes, no signs of recurrence or metastasis in the lung bilaterally.
Acknowledgements
Disclosure: The authors declare no conflict of interest.