Anatomical variations and pitfalls to know during thoracoscopic segmentectomies
With growing experience with thoracoscopic anatomical segmentectomies, the surgeon becomes more and more prudent and cautious during vascular dissection as he/she realizes there is not a unique and standard anatomy with variations but there is actually no regular anatomy. In other words, there are only variations. Although surgeons are performing pulmonary segmentectomies for years, they need a better understanding of anatomy when using a closed chest approach, because the vision is more limited and they cannot stretch and expose the parenchyma and broncho-vascular elements as they used to do with hands inside the chest cavity.
Throughout this article, we will describe most of the anatomical variations we have encountered during a consecutive series of 390 full thoracoscopic segmentectomies, either at surgery—with systematic shooting of anatomical features—or preoperatively by studying the 3-dimensional (3D) modelisation (1,2). This underlines the need for a thorough preparation of these procedures with use of 3D reconstructions, whose benefit has been stressed by many authors (3-9). By reading this paper and looking at the figures, those of the younger surgeons or those just embarking in this surgery will realize that even segmentectomies taken to be straightforward, e.g., lingulectomies or S6 segmentectomy, can be tricky.
This article will be based not only on our own experience but also on the “Illustrated anatomical segmentectomy for lung cancer” atlas by Nomori and Okada (10) that is a unique contribution to this topic and a precious support to the surgeon. Most data reported in this paper have been borrowed to this atlas.
In this article, we will describe only significant anatomical features of most common sublobar resections (SLR) and only those which have surgical consequences.
Right apico-posterior (S1+2) and posterior (S2) segmentectomies
Bronchus
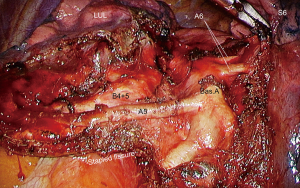
As it enters the parenchyma, the upper lobe bronchus triplicates into three segmental bronchi: apical (B1), posterior (B2) and anterior (B3). B1 and B2 can originate separately or as a common trunk (B1+2) (Figure 1). During a posterior approach, B2 can be mistaken for B1+2 if B1 and B2 are independent and if both bronchi are short.
Arteries
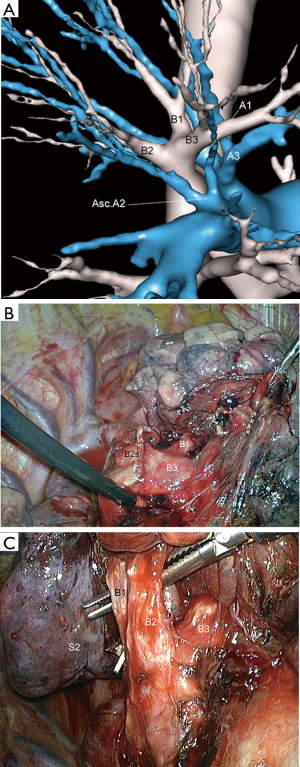
They arise from the truncus anterior (TA) and from the PA in the fissure, also named arterial truncus intermedius (ascending arteries). The TA duplicates into two branches: the apical artery A1 and the anterior artery A3 that must be preserved. The posterior segment is supplied by the ascending A2 (Asc.A2) that originates within the fissure from the posterior aspect of the pulmonary artery, opposite the middle lobe artery. It ascends to S2 and lies posteriorly to the lobar bronchus. In most patients, there is only one artery, while there are none or two in some patients. When there are two ascending A2, the most anterior one must not be mistaken for an anterior ascending branch (A3) which supplies the anterior segment (Figure 2).

In 72% of patients, a branch of the TA supplies S2 and is named recurrent A2 (Rec.A2). It usually runs along the bronchus. When present, the recurrent A2 can be at risk during dissection of B1 or B2.
In about 10% of patients, the ascending A2 artery originates from the superior supply of the lower lobe or forms a common trunk with A6.
Veins
In most cases, the segmental veins of the upper lobe are the two upper tributaries of the upper lobe vein: (I) V1 is the uppermost branch and is found in the hilum of the upper lobe. It is the most anterior and superior vessel; (II) V2+3 is the central vein and runs in the parenchyma and within the fissure. It gives a large posterior branch for V2 and small tributaries for V3. A small vein (V2t) draining S2 frequently cross the posterior aspect of the ascending A2 (Figure 3) and must be severed before dissecting this artery (11).
Right anterior segmentectomy (S3)
Bronchus
B3 is the anterior branch of the upper bronchus. It is usually independent from the apico-posterior truncus (B1+2) or from B1 and B2 and is usually easily recognized by its anterior direction, while B1 and B2 have a cephalad direction. Lymph nodes are frequently found at the origin of B3. Even for benign conditions, removal of these nodes is required for an optimal disclosure of B3 root.
Arteries
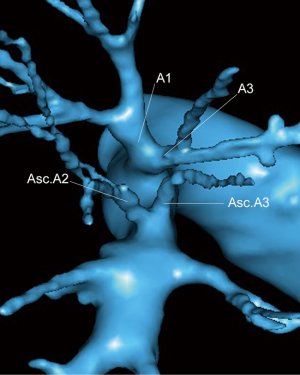
A3 is the lowermost branch of the TA. An ascending A3 is present in some patients, raising close to the ascending A2 and recognizable by its anterior direction. In some cases, there are two ascending arteries in the fissure. The posterior one (Asc.A2) for segment 2 and the anterior one (Asc.A3) for segment 3 (Figure 4). The latter must not be confused with a middle lobe artery which must always be identified before any ligation or clipping of an ascending artery.
Veins
There are two types of veins: (I) a large V3 that is the lowermost branch of the central vein and (II) 1 or 2 small ascending veins branching from the central vein that are easily recognized as they come directly from the anterior segment.
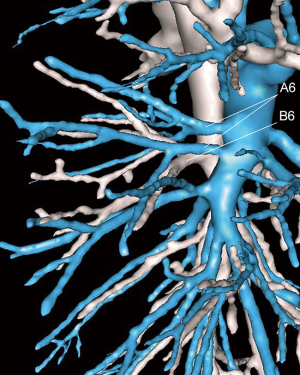
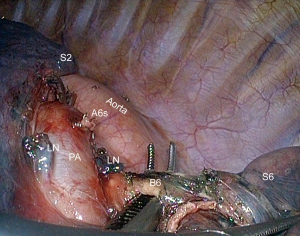
Right superior segmentectomy of the lower lobe (S6)
Bronchus
The superior segmental bronchus originates opposite or slightly above the middle lobe bronchus. It lies posteriorly to the segmental artery and separates into two main branches, rarely into 3. B6 is single in most patients but can seldom be double.
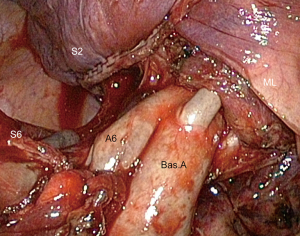
Arteries
The superior segment of the right lower lobe is supplied by an artery (A6) which originates within the fissure at the same level than the basal trunk. It is usually single, but can be double (Figure 5) and even triple. In some patients, the superior segmental artery originates from the ascending artery of the upper lobe (A2), or from the basal trunk (12) (Figure 6).
Veins
The vein to the superior segment is the uppermost and smaller segmental tributary (V6) of the inferior pulmonary vein (IPV).
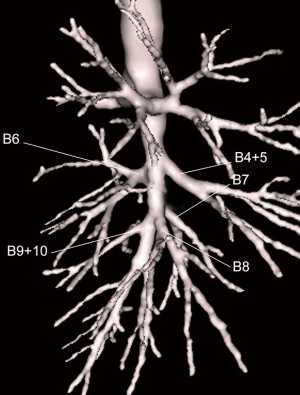
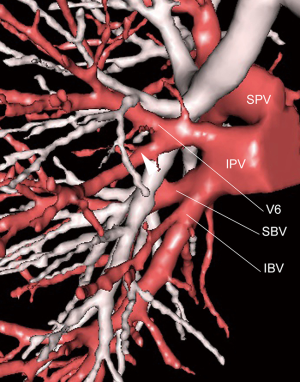
Right basilar segmentectomy (S7–10)
Bronchus
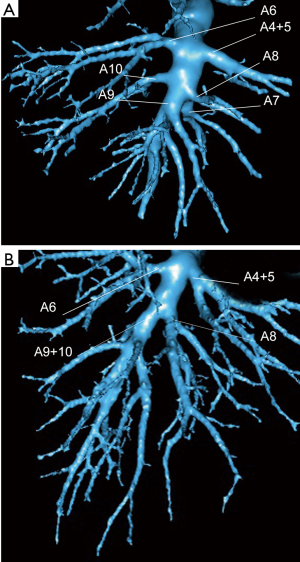
The origin of the common basal trunk is found in the fissure 1 to 2 cm beyond the origin of B6. The basilar bronchial trunk usually separates in three branches: B7, B8 and B9+10 (Figure 7) that run posterior to the corresponding segmental arteries. In rare cases (8%), instead of the usual B8 and B9+10 pattern, the branching is reverse, i.e., B8+9 and B10 and in 6% of patients, B7, B8, B9 and B10 are independent.
Arteries
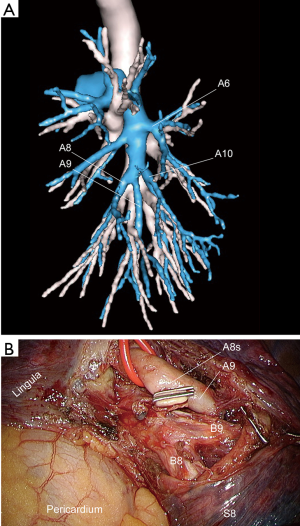
The arterial supply of the basal segments is the termination of the pulmonary artery after the birth of A6. It runs anterior to the segmental bronchus and usually separates into two main trunks, one for S7+8 and one for the posterior and lateral segments S9+10. It can also separate into 3 to 4 segmental branches. A7 can be lacking (16%). A8 and A9+10 are usually presenting as 2 separate trunks (90%) (Figure 8).
A middle lobe artery can arise from the basilar trunk, sometimes at a low level (Figure 9). This means an extensive dissection or the basilar trunk and/or segmental arteries is necessary to avoid accidental stapling of a middle lobe artery.
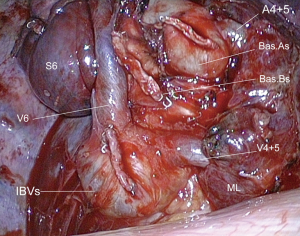
Veins
The basal segments are drained by two venous trunks, the inferior basilar vein (IBV) for S9+10 and the superior basilar vein (SBV) for S7+8. In some patients, there is only one common venous trunk or, on the contrary, a multiramified vein. In most cases, the two basilar veins receive tributaries from adjacent segments. This means that—as an example—ligating the S9+10 vein at the level of the central vein when performing a segmentectomy is at risk of sacrificing a venous branch draining S8.
The superior vein (V6) must be clearly identified before stapling these two trunks. The middle lobe vein can join the IPV (Figure 10). Conversely, the basilar vein can drain into the middle lobe vein.
Lingula sparing left upper lobectomy (S1–3)
Bronchi
In its most common pattern, the upper lobe bronchus splits immediately into the lingular bronchus and a common stem that usually separates into an anterior bronchus (B3) and an apico-posterior bronchus (B1+2). These three segmental bronchi have a short course that can make their identification and dissection difficult. Confusion between the anterior bronchus (B3) and the lingular bronchus is theoretically possible, as both B3 and B4+5, have an anterior course. However, when dissected in the fissure, the lingular bronchus is usually not visible if the lingular artery has not been divided. Only its origin is usually seen.
Arteries
There are two different supplies to the let upper lobe: the TA and the posterior arteries. The TA is often broad and short. It usually gives two main tributaries, the uppermost (A1+2) for S1 and S2 and the lowermost (A3) for S3. The posterior arteries originate in the fissure and distribute themselves over the curve of the pulmonary artery (Figure 11). Their number varies from 1 to 5, but most often from 2 to 3.
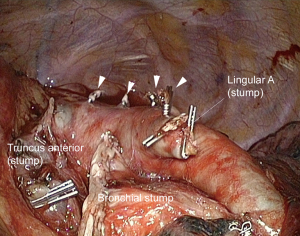
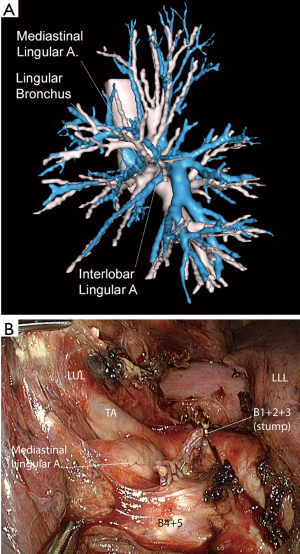
The presence of a mediastinal lingular artery (18%) should be search on 3D reconstruction (Figure 12). If present, dissection of the TA must be conducted with caution as this artery runs anterior between the vein and the B1+2+3 bronchial trunk and is in close contact with the bronchus. Dissecting around the bronchus should be done smoothly.
Veins
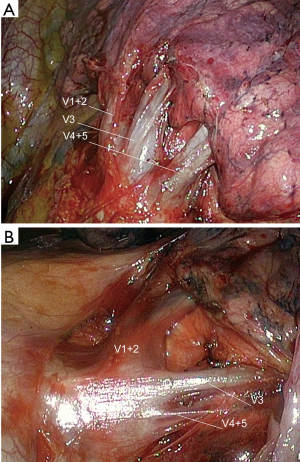
The superior pulmonary vein has usually three major tributaries (Figure 13A). The superior branch (V1+2) drains S1 and S2 segments. The middle branch (V3) drains S3 and the lowermost branch drains the lingula. In some rare cases, V1+2 can form a common trunk with V3. Even when 3D reconstruction demonstrates a clear pattern of the venous anatomy with a distribution of the lowermost venous branch to the lingula, V4+5 can be tiny (Figure 13B). It can be preferable to preserve the inferior branch of V3. In some cases, it is almost impossible to determine if the adjacent vein to the lingular one comes from the lingula or from S3. It seems prudent to preserve this vein, especially if the lingular vein is small.
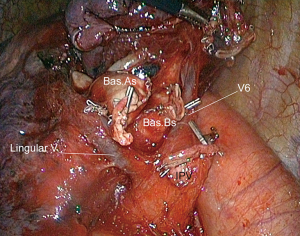
Lingulectomy (S4+5)
Bronchus
The lingular bronchus originates from the bifurcation of the upper lobe bronchus and has a short course before it enters the parenchyma. In rare cases, the lingular bronchus can rise from the basilar bronchial trunk.
Arteries
The main supply to the lingula comes from the lingular trunk, which is the most anterior branch of the posterior segmental arteries. It originates from the anterior aspect of the pulmonary artery within the fissure and splits into two segmental branches. In 26% of the patients, these two branches car rise separately from the main pulmonary artery.
An accessory lingular artery coming from the mediastinum, also named mediastinal or prebronchial lingular artery, is present in 18% of the patients. Its presence should be suspected when the usual lingular artery is tiny or absent. However, having 2 of these arteries with a normal diameter is not unusual.
An A3 artery can rise close to A4+5 or even form a common trunk with the lingular artery (Figure 14).
An artery to the basilar trunk or to A8 can rise from A4. This underlines the need for an extensive dissection of the lingular artery. If this variation is encountered, the branches of the lingular artery must be controlled separately.
Veins
The lingular vein is the lowermost tributary of the superior pulmonary vein. It is easily recognizable when the superior pulmonary vein has three major roots (V1+2, V3 and lingular). However, in some patients, there are multiple radiating venous branches. In these cases, it is safer to divide only the lowermost branch. Once the lingula will become mobile thanks to the arterial and bronchial division, the venous drainage will become more apparent.
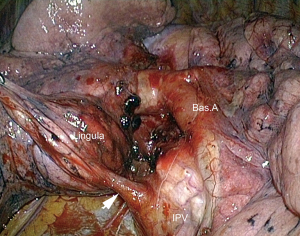
A lingular vein can drain into the IPV (Figure 15).
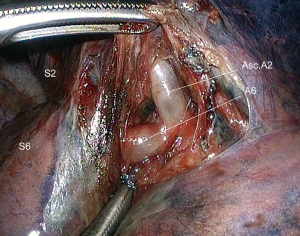
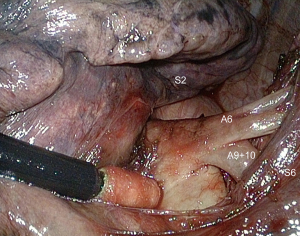
Left superior segmentectomy of the lower lobe (S6)
Bronchus
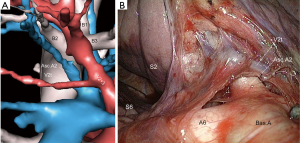
The superior segmental bronchus B6 is the first branch of the lower lobe bronchus. It arises laterally and posteriorly and lies posterior to the segmental artery. In obese or in some kyphotic patients, the bronchus can be located deeply and remote from A6, so that its identification and dissection can be difficult. It may be advisable to approach B6 from the back and from below, after division of V6 (Figure 16).
Arteries
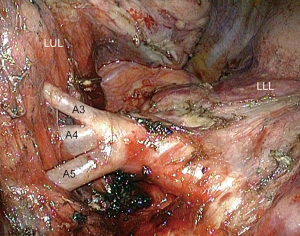
The superior segment of the left lower lobe is supplied by a single (80%) (Figure 17A) or double (18%) (Figure 17B,C) or even triple (2%) artery that originates from the posterior surface of the pulmonary artery in the posterior portion of the fissure. When single, A6 artery bifurcates in 2 or 3 branches. The artery runs anterior to the segmental bronchus. A lymph node is frequently encountered close to the posterior aspect of A6. It can tightly adhere to the artery and exposes to a vascular tear during dissection.
Branches to segments 9 and 10 can be close to A6 and should not be confused with a branch of A6 (Figure 18).
Vein
The superior segment is drained by the superior branch of the IPV (V6).
V6 can receive a venous branch from the basilar segments (Figure 19). In this case, only the uppermost tributary of V6 must be clipped.
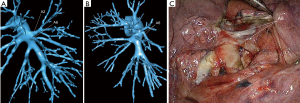
Left basilar segmentectomy (S8–10)
Bronchus
The origin of the common basal trunk is found in the fissure 1 to 2 cm beyond the origin of B6 and the lingular bronchus.
Arteries
The arterial supply of the basal segments is the termination of the pulmonary artery after the birth of the lingular artery and A6. It runs anterior to the segmental bronchus and usually divides into two main trunks, one for S8 and one for the posterior and lateral segments S9+10. It can also separate into 3 or 4 segmental branches.
A lingular artery can originate from the basilar artery, sometimes at a low level (Figure 20). It is thus essential to dissect the basilar arteries on a sufficient length to avoid inadvertent clipping of the lingular artery.
Veins
The basal segments are drained by two venous trunks, the inferior basilar vein (IBV) for S9+10 and the superior basilar vein (SBV) for S8. The superior vein (V6) must be clearly identified before stapling these two trunks.
The lingular vein can meet up with the IPV (Figure 21).
Left S8 segmentectomy (S8)
Bronchus
In most patients (80%), the basilar bronchial trunk usually separates in two branches: B8 and B9+10 which lie posterior to the segmental arteries. In rare cases (16%), the three bronchi are independent.
Arteries
The basilar arterial trunk branches separate in most cases (74%) in two arteries: A8 and A9+10, more seldom (10%) in three independent arteries or in two trunks A8+9 and A10 (16%). But all arteries to the lower lobe must be clearly identified to avoid misidentification, such as a low A8a being mistaken for an A9+10 (Figure 22) When in doubt during dissection, it is preferable to control only the anterior branch of A8 (A8b), then the bronchus and eventually check the direction of the second branch. The branching of the arteries and bronchi can be difficult to understand without help of a 3D modelisation. Instead of common B9+10 trunk, B9 can have a common birth with B8. Same as for the corresponding arteries. There is a risk of dividing B9 with B8 or A9 together with A8.
Vein
The superior basal vein (SBV), which is the middle root of the IPV, does not always represent the venous drainage of segment 8. Its posterior branch can drain segment 9. It is advisable to divide only the anterior branch of the vein (V8a) which runs immediately behind the bronchus, rather than controlling V8 centrally in the IPV.
Left S9+10 segmentectomy (S9+10)
Bronchus and arteries
These have been described in the previous paragraph. Instead of A8 and A9+10 (Figure 23), the following branching pattern can be encountered in 20% of patients: A8+9 and A10 (Figure 22A,B) or totally independent basal arteries (A8, A9 and A10). The same distribution is valid for bronchi. Preoperative modelisation is helpful to avoid anatomical misjudgment.
Vein
The inferior basal vein (IBV), which is the lower root of the IPV, does not always represent the venous drainage of S9 and S10. One of its branches can drain S8. If any doubt, only the lowermost branch of the vein must be divided. It is however safer to control veins in the parenchyma. There are frequently no basal veins but just a branching into a common basal vein and V6. This stress the need to favor venous control in the parenchyma rather than centrally in the IPV.
Acknowledgements
Three-dimensional modelisations used for the illustrations of this work were made possible thanks to a grant from the Ligue contre le Cancer-Comité de Paris.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Gossot D, Zaimi R, Fournel L, et al. Totally thoracoscopic pulmonary anatomic segmentectomies: technical considerations. J Thorac Dis 2013;5:S200-6. [PubMed]
- Gossot D. Atlas of endoscopic major pulmonary resections. 2nd edition. Tokyo: Springer-Verlag, 2010.
- Chen-Yoshikawa TF, Date H. Update on three-dimensional image reconstruction for preoperative simulation in thoracic surgery. J Thorac Dis 2016;8:S295-301. [PubMed]
- Fukuhara K, Akashi A, Nakane S, et al. Preoperative assessment of the pulmonary artery by three-dimensional computed tomography before video-assisted thoracic surgery lobectomy. Eur J Cardiothorac Surg 2008;34:875-7. [Crossref] [PubMed]
- Hagiwara M, Shimada Y, Kato Y, et al. High-quality 3-dimensional image simulation for pulmonary lobectomy and segmentectomy: results of preoperative assessment of pulmonary vessels and short-term surgical outcomes in consecutive patients undergoing video-assisted thoracic surgery†. Eur J Cardiothorac Surg 2014;46:e120-6. [Crossref] [PubMed]
- Ikeda N, Yoshimura A, Hagiwara M, et al. Three dimensional computed tomography lung modeling is useful in simulation and navigation of lung cancer surgery. Ann Thorac Cardiovasc Surg 2013;19:1-5. [Crossref] [PubMed]
- Iwano S, Yokoi K, Taniguchi T, et al. Planning of segmentectomy using three-dimensional computed tomography angiography with a virtual safety margin: technique and initial experience. Lung Cancer 2013;81:410-5. [Crossref] [PubMed]
- Yang Q, Xie B, Hu M, et al. Thoracoscopic anatomic pulmonary segmentectomy: a 3-dimensional guided imaging system for lung operations. Interact Cardiovasc Thorac Surg 2016;23:183-9. [Crossref] [PubMed]
- Sato M, Yamada T, Menju T, et al. Virtual-assisted lung mapping: outcome of 100 consecutive cases in a single institute. Eur J Cardiothorac Surg 2015;47:e131-9. [Crossref] [PubMed]
- Nomori H, Okada M. Illustrated anatomical Segmentectomy for Lung Cancer. Tokyo: Springer-Verlag, 2012.
- Shimizu K, Nagashima T, Ohtaki Y, et al. Analysis of the variation pattern in right upper pulmonary veins and establishment of simplified vein models for anatomical segmentectomy. Gen Thorac Cardiovasc Surg 2016;64:604-11. [Crossref] [PubMed]
- Nagashima T, Shimizu K, Ohtaki Y, et al. Analysis of variation in bronchovascular pattern of the right middle and lower lobes of the lung using three-dimensional CT angiography and bronchography. Gen Thorac Cardiovasc Surg 2017;65:343-9. [Crossref] [PubMed]