An update on mandibular advancement devices for the treatment of obstructive sleep apnoea hypopnoea syndrome
Introduction
Obstructive sleep apnoea hypopnoea syndrome (OSAHS) is a common sleep disorder characterised by intermittent upper airway collapse resulting in oxygen desaturation and sleep fragmentation. Excessive daytime sleepiness (EDS) is associated with cognitive impairment, mood disturbance and decreased quality of life (QoL). OSAHS is also linked with increased risk of road traffic accidents, cardiovascular disease and all-cause mortality (1,2). It affects 2–7% of adults (3) and an estimated 1% of UK men have severe OSAHS (4). Many cases go untreated due to not being diagnosed or intolerance of treatment. The consequences are estimated to cost the NHS around £432 million each year (2,5).
The pathogenesis of OSAHS is a complex interaction of multiple factors including pharyngeal anatomy, dilator muscle dysfunction and reduced lung volume (6). Whilst the relative contributions of these mechanisms vary between patients, the common result is sleep related upper airway collapse. The gold standard treatment remains continuous positive airway pressure (CPAP) therapy (7). It pressurises the upper airway to prevent collapse, reducing the frequency of apnoeas and hypopnoeas. However, CPAP effectiveness is limited by intolerance and poor compliance, with failure rates of 46–83% (8). There is a pressing need for alternatives to CPAP.
In recent years, oral appliances have emerged as the leading alternative to CPAP. These devices are by no means a homogenous group as they differ greatly in both design and action. Nevertheless, the tongue is affected by all the appliances, either directly by forward movement of the muscle, or indirectly by advancing the mandible. The most commonly used appliances are mandibular advancement devices (MAD) and there is now a strong body of evidence supporting their use in OSAHS. Clinical guidelines recommend MAD ahead of CPAP in mild OSAHS and in more severe OSAHS when CPAP is refused or not tolerated (7,9,10). However, there are still barriers to MAD provision. Their effectiveness can be difficult to predict and there is still debate about the required level of design sophistication. These uncertainties prevent more widespread inclusion of MAD within clinical sleep services.
This review will focus on the efficacy, effectiveness, design features, side-effects of and patient selection for MAD therapy. Comparison will also be made between MAD and CPAP therapy.
Mechanism of action of MAD
MAD prevent upper airway collapse by protruding the mandible forward, thus altering the jaw and tongue position. They are also referred to in the literature as mandibular advancement splints (MAS) or mandibular repositioning appliances (MRA). Both video endoscopy and magnetic resonance imaging (MRI)-guided studies have determined that these devices predominantly increase the volume of the airway at the level of the velopharynx (11,12). The airway space is mostly enlarged laterally, thought to be due to traction on soft tissue connections between the pharynx and the mandibular ramus (13).
It was previously thought that even an inactive oral appliance (i.e., not protruding the mandible) may reduce apnoeic episodes. However, numerous randomised controlled trials (RCT) have established the efficacy of MAD over placebo including inactive appliances (14-16). The lack of significant difference between the inactive appliances and a no intervention control in one study is further evidence that the mechanism of action is through mandibular protrusion (16).
Efficacy of MAD
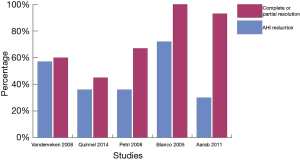
Treatment objectives for OSAHS address both the physiological and symptomatic aspects of the disease. The physiological goals target obstructive events, sleep fragmentation and oxygen desaturation. Symptomatic goals target snoring, sleepiness, QoL and possibly comorbidities. However, even published studies that share treatment objectives can vary in their definition of treatment success. This variability complicates the interpretation of efficacy. The apnoea-hypopnoea index (AHI) is the number of apnoea and hypopnoea events per hour of sleep. Most studies define treatment success as achieving a certain AHI target (usually ≤5–10/hour) or a certain percentage reduction in AHI (usually 50%). Studies since 2005 that looked at therapy with bespoke MADs (custom made from dental impressions) have reported mean AHI reductions of between 30% and 72%. Reviewing the data of these studies revealed a complete response (AHI <5) or partial response (≥50% reduction in AHI from baseline, but AHI >5) of between 45% and 100% (Figure 1) (15-19). Studies with higher response rates recruited patients with lower AHI at baseline. Blanco et al. (15) reported a 100% response rate, however the study had limitations due to small sample size and a high proportion of subjects withdrawing from the trial.
Apart from reductions in AHI, studies have also shown that MAD can improve the arousal index, oxygen saturation parameters and increase Rapid eye movement (REM) sleep duration (20-22). Partners of those on MAD therapy also benefit from reduction in snoring (15,20-22).
Health outcomes of MAD
EDS is reduced by MAD treatment. When measured subjectively using the Epworth Sleepiness score (ESS) all recent studies have shown a significant improvement in EDS with MAD treatment compared to inactive appliances (14-16,20-22). Published objective sleepiness outcomes are few and results vary. An early study (20) found that MAD improved mean sleep latency on Multiple Sleep Latency Test (MSLT) compared to an inactive appliance. However, when examining alertness with the Maintenance of Wakefulness Test, another study found no effects of either CPAP or MAD on mean sleep latency compared to placebo (23). In a more recent study both CPAP and MAD improved Oxford sleep resistance test scores to a similar extent (24). The varying results are probably a function of the different tests used, and variability in treatment implementation and compliance between studies.
Earlier meta-analyses were inconclusive about the effects of MAD therapy on QoL (25), but this may have been due to small studies and inconsistent methodologies. More recently, both generic and disease specific QoL measures have been shown to improve with MAD when compared to inactive controls (18). Perceived health status and QoL questionnaires specific for OSAHS showed considerable improvements after MAD (15). Generic questionnaires such as the Short Form 36 (SF-36) have also showed improvement in multiple studies (16,26).
Systolic and diastolic blood pressure (BP) have been shown to improve with MAD treatment (14,27). This is especially the case in hypertensive patients. A study with long follow-up data reported that positive effects on BP persisted for up to 4.5 years (28). BP benefits are not seen in all OSA intervention studies, including those testing CPAP. A well-designed pragmatic RCT comparing CPAP to MAD showed no effect on BP for either treatment in moderate to severe OSAHS (29). However, a recent meta-analysis demonstrated an overall benefit of MAD therapy to BP (30).
MAD compared to CPAP
CPAP is considered the gold standard treatment for OSAHS. It is highly efficacious in reducing obstructive events as measured by the AHI and can improve EDS, QoL and BP. Although efficacious, CPAP effectiveness is often limited by low adherence. When applying the popular minimum acceptable CPAP compliance threshold of 4 hours per night, failure rates have ranged from 29% to 83% depending on the study population (8,31).
Numerous studies have compared MAD to CPAP. Most have recruited patients with mild-moderate OSAHS, although more severe disease has also featured (25,29,32,33). Many of these papers have fed into meta-analyses, and a recent one examined the results of all trials comparing MAD to CPAP (34). All studies used AHI as the primary outcome of efficacy with multiple secondary outcomes including oxygen desaturation index (ODI) and arousal index. Results consistently demonstrate that CPAP is more effective than MADs at reducing sleep disordered breathing and achieving complete control of OSAHS (AHI <5) (34).
Despite the greater effect of CPAP on objective polysomnographic parameters, it does not appear to be more effective at achieving better health outcomes. It seems that the higher efficacy of CPAP is offset by greater MAD compliance. Phillips et al. (29) showed that CPAP and MAD achieved similar improvements in EDS and QoL. Average MAD compliance was 6.5 hours/night compared to 5.2 for CPAP (P<0.0001). These results are consistent with other studies (23,24,32), supporting the hypothesis that MAD and CPAP have similar clinical effectiveness due to greater MAD compliance achieving net similar AHI reduction (35,36).
Adherence also influences health economics. The cost effectiveness of MAD and CPAP in mild to moderate OSA was recently reviewed by investigators who included data from the TOMADO study. Sensitivity analysis found that MAD becomes more cost effective than CPAP when CPAP compliance drops below 90% of MAD usage. Therefore, it is important to determine factors influencing compliance and to employ a patient-centred approach when deciding which therapy to initiate (37). A focus group-based study interviewing CPAP and MAD users found that the four most important factors determining choice of treatment were device effectiveness, transportability, embarrassment and cost (38). This may explain the higher nightly MAD usage frequently reported in trials and why patients often prefer MAD to CPAP (39,40).
Design features influencing the efficacy of MAD
The design and sophistication of MAD vary greatly. Variables include adjustability, nature or extent of customisation and materials used; and they are not mutually exclusive. This complex heterogeneity undermines attempts to elucidate factors’ individual impacts on the effectiveness of specific appliances. The TOMADO study was a comprehensive RCT comparing three different non-adjustable MAD (18), but more work is needed in this area.
Non-adjustable, over-the-counter “boil and bite” appliances are the cheapest option available (Figure 2A). They are constructed of a thermoplastic material that becomes mouldable when warmed by immersion in hot water. The user takes a mould of their teeth by biting into the softened material that then sets on cooling. Customised devices are constructed in a lab using dental impressions. The TOMADO study found that thermoplastic MAD could reduce AHI. However, they were less effective because they were poorly tolerated and fell out easily, so adherence was lower (18).
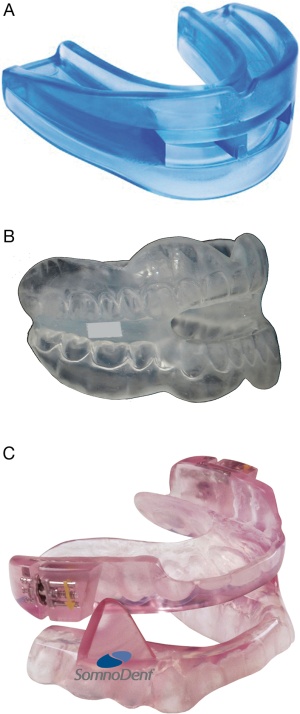
Custom made devices can either be a one-piece or an adjustable two-piece appliance. Upper and lower dental splints are fused in the one-piece device (monobloc), which is cheaper and easier to construct (Figure 2B). Although most of these appliances are a bespoke dentally produced device, “semi-bespoke” MAD, which require no specialist dental input, exist. The TOMADO study reported similar AHI reduction, tolerance and device retention with semi-bespoke MAD and dentally produced and fitted monoblocs. Semi-bespoke devices were found to be the most cost effective too, so the authors recommended that they be considered first choice when considering MAD therapy (41).
Adjustable two-piece devices come in separate upper and lower plates (Figure 2C). Construction requires additional specialist jaw articulation and is more expensive. Serially titrated mandibular protrusion is thought to increase treatment success by allowing gradual adaptation to optimal protrusion (42,43). The ability to titrate protrusion according to efficacy and tolerance is the key advantage of adjustable MAD (aMAD) and the main justification for their recommendation in clinical guidelines (10,44). However, there is a lack of supporting evidence. The degree of mandibular protrusion used in published studies has been highly variable, ranging from 50% to 80% of maximal protrusion (27,44). Existing studies that have compared so-called fixed MAD (fMAD) to aMAD have had methodological limitations and inconsistent findings (45-47). For example, one study comparing two devices set different protrusions for fMADs and aMADs, thus essentially comparing protrusions rather than devices. There is a need for a robust comparison of fMAD and aMADs.
Side effects of MAD
Most complications of MAD therapy are mild and temporary. They are nonetheless significant as they can limit device tolerance and effectiveness, so efforts are needed to mitigate this risk. Some authors have suggested that more side effects may be seen with greater levels of protrusion (48), but this has not been properly verified.
Short-term side effects usually occur during acclimatisation in the first few weeks of therapy. These include hypersalivation, dry mouth, dental pain, gingival irritation, myofascial pain and temporomandibular joint (TMJ) discomfort (49,50).
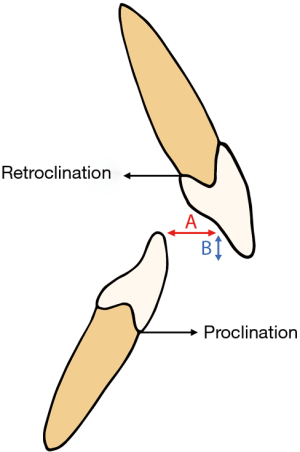
More information is needed on the incidence of long-term side effects but they seem to mostly involve dentofacial changes. MAD use the patient’s dentition and alveolar ridges for retention when advancing the mandible forward. This invariably exerts reciprocal forces on the dentofacial structures. Changes in facial height and jaw relationship have been noted as early as 6 months into MAD use (51). Dental changes mainly relate to decreases in overbite and overjet as well as proclination of the lower incisors and retroclination of upper incisors (Figure 3) (51-56). A more recent paper reported how some patients undergoing MAD therapy experience occlusal alterations to posterior teeth (57). Appropriate planning and monitoring may avoid these effects as there is some evidence that an orthodontic MAD can increase overjet in those patients at risk of developing dentoalveolar changes (58). Despite the concerns about long-term dental side effects, it seems increasingly accepted that they may be a price worth paying for successful treatment of OSAHS (59).
Many studies have reported TMJ disorders complicating MAD use (50,58,60,61). However, these effects are transient and any pain appears to decrease in intensity with continued MAD use (61). In those with more noticeable TMJ pain, mandibular exercises may allow perseverance with MAD therapy until the discomfort improves (62,63).
There are some contraindications to MAD therapy. These include severe periodontal disease, severe pre-existing TMJ disorders, lack of adequate retention (inadequate dentition or implants) and severe gag reflex. Poor dexterity and other factors limiting hand function may also be relevant if they compromise device handling (43).
Predictors of treatment success
The unpredictability of response to MAD therapy is a significant barrier to the wider consideration of this treatment option by clinicians. Numerous studies have explored for clinical and sleep study predictors of treatment success. Younger age, lower body mass index (BMI) and smaller neck circumference have been related to successful MAD treatment (64-68). Female gender has also been suggested as a potential indicator of treatment success (64). In addition, polysomnographic parameters such as low AHI (64,66) and position dependent OSAH (69-71) have been proposed as predictors. However, none of these factors are sufficiently discriminatory. For example, successful treatment of OSAHS with MAD can be achieved in overweight patients and those with more severe disease (72,73).
Lateral cephalometric radiographs have also been tested. A retrognathic mandible, shorter soft palate and low-set hyoid bone have all been associated with favourable outcomes (74). However, these associations are weak and again cannot be relied on for clinical decision making. MRI with computational manipulation of the scans has been investigated (75). Although the science is promising, the costs undermine feasibility for most healthcare settings. Similarly, drug-induced sleep endoscopy continues to be explored as a predictive tool (76). Although effective in research settings and a few specialist centres this relatively expensive and intrusive investigation seems unlikely to be widely applied to routine clinical practice.
Perhaps a more promising method to predict treatment success is one in which mandibular advancement can be tested with a basic, cheap device before prescription of a more costly MAD. This has previously been explored with a thermoplastic MAD (17). Thermoplastic outcomes did not predict successful therapy with a customised MAD. However, the basic device was poorly tolerated and easily displaced. Furthermore, only around a third of patients were excessively sleepy at baseline and not all had significant OSA. More recent research has focused on titrating mandibular advancement during sleep studies in order to assess potential efficacy and determine optimal mandibular protrusion. Early prototypal studies have been promising (77,78), but again, these methods are resource expensive and seem unlikely to be widely adopted. Another recent innovation is adjustable thermoplastic MAD, which allow cheaper mandibular titration. A recent study showed these devices to be effective at reducing AHI in the short term (79). It remains to be seen whether they offer a long-term alternative to custom made adjustable MAD or whether they can be used to predict treatment response to the more expensive and longer lasting devices.
Current guidelines
Recommendations regarding the role of MAD therapy vary, but there are areas of agreement. Most clinical guidelines agree that MAD should be offered to patients with mild to moderate OSAHS and to those with more severe disease who do not want or cannot tolerate CPAP (7,9,10). They also state that MAD should be provided by qualified dentists who have had appropriate training in the field. Despite a lack of high level evidence, the ability to adjust protrusion according to efficacy and tolerance has meant that aMADs are increasingly recommended (10,43,80,81). Existing guidelines overlook semi-bespoke and thermoplastic adjustable devices. There is a need to update recommendations to reflect the latest evidence but continued research is also needed to address the uncertainties discussed in this article.
Conclusions
CPAP therapy is highly effective in OSAHS. However, this is often undermined by low adherence due to treatment intolerance. Cost effectiveness of CPAP is also less clear in milder disease. Historically, the heterogeneity of MAD therapy has contributed to uncertainty about its precise role. This continues but in recent years more evidence has emerged of the effectiveness of MAD therapy across the range of OSAHS severity. In milder disease, the data support MAD use as they are beneficial and cost-effective. In more severe cases, MAD should be considered for those who decline or cannot tolerate CPAP. High quality pragmatic research is needed to compare fixed to adjustable devices. More work is also needed to identify a simple and clinically feasible method of identifying patients likely to benefit from MAD therapy.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Marshall NS, Wong KK, Liu PY, et al. Sleep apnea as an independent risk factor for all-cause mortality: the Busselton Health Study. Sleep 2008;31:1079-85. [PubMed]
- Sleep Alliance. Sleep SOS Report: The Impact of Sleep on Society. 2004.
- Punjabi NM. The epidemiology of adult obstructive sleep apnea. Proc Am Thorac Soc 2008;5:136-43. [Crossref] [PubMed]
- Stradling JR, Barbour C, Glennon J, et al. Prevalence of sleepiness and its relation to autonomic evidence of arousals and increased inspiratory effort in a community based population of men and women. J Sleep Res 2000;9:381-8. [Crossref] [PubMed]
- Douglas NJ, George CFP. Treating sleep apnoea is cost effective. Thorax 2002;57:93. [Crossref] [PubMed]
- Eckert DJ, Malhotra A, Jordan AS. Mechanisms of Apnea. Prog Cardiovasc Dis 2009;51:313-23. [Crossref] [PubMed]
- National Institute for Health and Clinical Excellence. Continuous positive airway pressure for obstructive sleep apnoea/hypopnoea syndrome. 2008. Available online: https://www.nice.org.uk/guidance/ta139/resources/continuous-positive-airway-pressure-for-obstructive-sleep-apnoeahypopnoea-syndrome-pdf-374791501
- Weaver TE, Grunstein RR. Adherence to continuous positive airway pressure therapy: the challenge to effective treatment. Proc Am Thorac Soc 2008;5:173-8. [Crossref] [PubMed]
- Scottish Intercollegiate Guidelines Network. Management of Obstructive Sleep Apnoea/Hypopnoea Syndrome in Adults: A national clinical guideline. 2003. Available online: http://www.lothianrespiratorymcn.scot.nhs.uk/wp-content/uploads/2010/11/SIGN-73-Management-of-Obstructive-Sleep-Apnoea_Hypopnoea-Syndrome-in-Adults.pdf
- Ramar K, Dort LC, Katz SG, et al. Clinical Practice Guideline for the Treatment of Obstructive Sleep Apnea and Snoring with Oral Appliance Therapy: An Update for 2015. J Clin Sleep Med 2015;11:773-827. [PubMed]
- Chan AS, Sutherland K, Schwab RJ, et al. The effect of mandibular advancement on upper airway structure in obstructive sleep apnoea. Thorax 2010;65:726-32. [Crossref] [PubMed]
- Ryan CF, Love LL, Peat D, et al. Mandibular advancement oral appliance therapy for obstructive sleep apnoea: effect on awake calibre of the velopharynx. Thorax 1999;54:972-7. [Crossref] [PubMed]
- Brown EC, Cheng S, McKenzie DK, et al. Respiratory Movement of Upper Airway Tissue in Obstructive Sleep Apnea. Sleep 2013;36:1069-76. [Crossref] [PubMed]
- Andrén A, Hedberg P, Walker-Engstrom ML, et al. Effects of treatment with oral appliance on 24-h blood pressure in patients with obstructive sleep apnea and hypertension: a randomized clinical trial. Sleep Breath 2013;17:705-12. [Crossref] [PubMed]
- Blanco J, Zamarron C, Abeleira Pazos MT, et al. Prospective evaluation of an oral appliance in the treatment of obstructive sleep apnea syndrome. Sleep Breath 2005;9:20-5. [Crossref] [PubMed]
- Petri N, Svanholt P, Solow B, et al. Mandibular advancement appliance for obstructive sleep apnoea: results of a randomised placebo controlled trial using parallel group design. J Sleep Res 2008;17:221-9. [Crossref] [PubMed]
- Vanderveken OM, Devolder A, Marklund M, et al. Comparison of a custom-made and a thermoplastic oral appliance for the treatment of mild sleep apnea. Am J Respir Crit Care Med 2008;178:197-202. [Crossref] [PubMed]
- Quinnell TG, Bennett M, Jordan J, et al. A crossover randomised controlled trial of oral mandibular advancement devices for obstructive sleep apnoea-hypopnoea (TOMADO). Thorax 2014;69:938-45. [Crossref] [PubMed]
- Aarab G, Lobbezoo F, Heymans MW, et al. Long-term follow-up of a randomized controlled trial of oral appliance therapy in obstructive sleep apnea. Respiration 2011;82:162-8. [Crossref] [PubMed]
- Gotsopoulos H, Chen C, Qian J, et al. Oral appliance therapy improves symptoms in obstructive sleep apnea: A randomized, controlled trial. Am J Respir Crit Care Med 2002;166:743-8. [Crossref] [PubMed]
- Johnston CD, Gleadhill IC, Cinnamond MJ, et al. Mandibular advancement appliances and obstructive sleep apnoea: A randomized clinical trial. Eur J Orthod 2002;24:251-62. [Crossref] [PubMed]
- Mehta A, Qian J, Petocz P, et al. A randomized, controlled study of a mandibular advancement splint for obstructive sleep apnea. Am J Respir Crit Care Med 2001;163:1457-61. [Crossref] [PubMed]
- Barnes M, McEvoy RD, Banks S, et al. Efficacy of positive airway pressure and oral appliance in mild to moderate obstructive sleep apnea. Am J Respir Crit Care Med 2004;170:656-64. [Crossref] [PubMed]
- Gagnadoux F, Fleury B, Vielle B, et al. Titrated mandibular advancement versus positive airway pressure for sleep apnoea. Eur Respir J 2009;34:914-20. [Crossref] [PubMed]
- Lim J, Lasserson TJ, Fleetham J, et al. Oral appliances for obstructive sleep apnoea. Cochrane Database of Systematic Reviews 2006. Available online: http://doi.wiley.com/10.1002/14651858.CD004435.pub3
- Galic T, Bozic J, Pecotic R, et al. Improvement of Cognitive and Psychomotor Performance in Patients with Mild to Moderate Obstructive Sleep Apnea Treated with Mandibular Advancement Device: A Prospective 1-Year Study. J Clin Sleep Med 2016;12:177-86. [Crossref] [PubMed]
- Gotsopoulos H, Kelly JJ, Cistulli PA. Oral appliance therapy reduces blood pressure in obstructive sleep apnea: a randomized, controlled trial. Sleep 2004;27:934-41. [Crossref] [PubMed]
- Gauthier L, Almeida F, Arcache JP, et al. Position paper by Canadian dental sleep medicine professionals on the role of different health care professionals in managing obstructive sleep apnea and snoring with oral appliances. Can Respir J 2012;19:307-9. [Crossref] [PubMed]
- Phillips CL, Grunstein RR, Darendeliler MA, et al. Health outcomes of continuous positive airway pressure versus oral appliance treatment for obstructive sleep apnea: a randomized controlled trial. Am J Respir Crit Care Med 2013;187:879-87. [Crossref] [PubMed]
- Bratton DJ, Gaisl T, Wons AM, et al. CPAP vs Mandibular Advancement Devices and Blood Pressure in Patients With Obstructive Sleep Apnea: A Systematic Review and Meta-analysis. JAMA 2015;314:2280-93. [Crossref] [PubMed]
- Sawyer AM, Gooneratne NS, Marcus CL, et al. A systematic review of CPAP adherence across age groups: Clinical and empiric insights for developing CPAP adherence interventions. Sleep Med Rev 2011;15:343-56. [Crossref] [PubMed]
- Engleman HM, McDonald JP, Graham D, et al. Randomized crossover trial of two treatments for sleep apnea/hypopnea syndrome: Continuous positive airway pressure and mandibular repositioning splint. Am J Respir Crit Care Med 2002;166:855-9. [Crossref] [PubMed]
- Hoekema A, Stegenga B, Wijkstra PJ, et al. Obstructive sleep apnea therapy. J Dent Res 2008;87:882-7. [Crossref] [PubMed]
- Sharples LD, Clutterbuck-James AL, Glover MJ, et al. Meta-analysis of randomised controlled trials of oral mandibular advancement devices and continuous positive airway pressure for obstructive sleep apnoea-hypopnoea. Sleep Med Rev 2016;27:108-24. [Crossref] [PubMed]
- de Almeida FR. Complexity and efficacy of mandibular advancement splints: Understanding their mode of action. J Clin Sleep Med 2011;7:447-8. [PubMed]
- Vanderveken OM, Dieltjens M, Wouters K, et al. Objective measurement of compliance during oral appliance therapy for sleep-disordered breathing. Thorax 2013;68:91-6. [Crossref] [PubMed]
- Almeida FR, Bansback N. Long-term effectiveness of oral appliance versus CPAP therapy and the emerging importance of understanding patient preferences. Sleep 2013;36:1271-2. [Crossref] [PubMed]
- Almeida FR, Henrich N, Marra C, et al. Patient preferences and experiences of CPAP and oral appliances for the treatment of obstructive sleep apnea: a qualitative analysis. Sleep Breath 2013;17:659-66. [Crossref] [PubMed]
- Sutherland K, Vanderveken OM, Tsuda H, et al. Oral Appliance Treatment for Obstructive Sleep Apnea: An Update. J Clin Sleep Med 2014;10:215-27. [PubMed]
- White DP, Shafazand S. Mandibular advancement device vs. CPAP in the treatment of obstructive sleep apnea: are they equally effective in Short term health outcomes? J Clin Sleep Med 2013;9:971-2. [PubMed]
- Sharples L, Glover M, Clutterbuck-James A, et al. Clinical effectiveness and cost-effectiveness results from the randomised controlled Trial of Oral Mandibular Advancement Devices for Obstructive sleep apnoea-hypopnoea (TOMADO) and long-term economic analysis of oral devices and continuous positive airwa. Health Technol Assess 2014;18:1-296. [Crossref] [PubMed]
- Fleury B, Rakotonanahary D, Petelle B, et al. Mandibular advancement titration for obstructive sleep apnea: Optimization of the procedure by combining clinical and oximetric parameters. Chest 2004;125:1761-7. [Crossref] [PubMed]
- Ngiam J, Balasubramaniam R, Darendeliler MA, et al. Clinical guidelines for oral appliance therapy in the treatment of snoring and obstructive sleep apnoea. Aust Dent J 2013;58:408-19. [Crossref] [PubMed]
- Gindre L, Gagnadoux F, Meslier N, et al. Mandibular advancement for obstructive sleep apnea: dose effect on apnea, long-term use and tolerance. Respiration 2008;76:386-92. [Crossref] [PubMed]
- Lawton HM, Battagel JM, Kotecha B. A comparison of the Twin Block and Herbst mandibular advancement splints in the treatment of patients with obstructive sleep apnoea: A prospective study. Eur J Orthod 2005;27:82-90. [Crossref] [PubMed]
- Bloch KE, Iseli A, Zhang JN, et al. A randomized, controlled crossover trial of two oral appliances for sleep apnea treatment. Am J Respir Crit Care Med 2000;162:246-51. [Crossref] [PubMed]
- Lettieri CJ, Paolino N, Eliasson AH, et al. Comparison of adjustable and fixed oral appliances for the treatment of obstructive sleep apnea. J Clin Sleep Med 2011;7:439-45. [PubMed]
- Aarab G, Lobbezoo F, Hamburger HL, et al. Effects of an oral appliance with different mandibular protrusion positions at a constant vertical dimension on obstructive sleep apnea. Clin Oral Investig 2010;14:339-45. [Crossref] [PubMed]
- Sutherland K, Cistulli P. Mandibular advancement splints for the treatment of sleep apnea syndrome. Swiss Med Wkly 2011;141:w13276. [PubMed]
- Hoffstein V. Review of oral appliances for treatment of sleep-disordered breathing. Sleep Breath 2007;11:1-22. [Crossref] [PubMed]
- Robertson C, Herbison P, Harkness M. Dental and occlusal changes during mandibular advancement splint therapy in sleep disordered patients. Eur J Orthod 2003;25:371-6. [Crossref] [PubMed]
- Hammond RJ, Gotsopoulos H, Shen G, et al. A follow-up study of dental and skeletal changes associated with mandibular advancement splint use in obstructive sleep apnea. Am J Orthod Dentofacial Orthop 2007;132:806-14. [Crossref] [PubMed]
- Martínez-Gomis J, Willaert E, Nogues L, et al. Five years of sleep apnea treatment with a mandibular advancement device. Side effects and technical complications. Angle Orthod 2010;80:30-6. [Crossref] [PubMed]
- Doff MHJ, Hoekema A, Pruim GJ, et al. Long-term oral-appliance therapy in obstructive sleep apnea: a cephalometric study of craniofacial changes. J Dent 2010;38:1010-8. [Crossref] [PubMed]
- Doff MH, Finnema KJ, Hoekema A, et al. Long-term oral appliance therapy in obstructive sleep apnea syndrome: a controlled study on dental side effects. Clin Oral Investig 2013;17:475-82. [Crossref] [PubMed]
- Almeida FR, Lowe AA, Otsuka R, et al. Long-term sequellae of oral appliance therapy in obstructive sleep apnea patients: Part 2. Study-model analysis. Am J Orthod Dentofacial Orthop 2006;129:205-13. [Crossref] [PubMed]
- Perez CV, de Leeuw R, Okeson JP, et al. The incidence and prevalence of temporomandibular disorders and posterior open bite in patients receiving mandibular advancement device therapy for obstructive sleep apnea. Sleep Breath 2013;17:323-32. [Crossref] [PubMed]
- Marklund M, Legrell PE. An orthodontic oral appliance. Angle Orthod 2010;80:1116-21. [Crossref] [PubMed]
- Almeida F. Long term side effects of mas-does it matter? Sleep Biol Rhythms 2013;11:6.
- Gao X, Otsuka R, Ono T, et al. Effect of titrated mandibular advancement and jaw opening on the upper airway in nonapneic men: A magnetic resonance imaging and cephalometric study. Am J Orthod Dentofacial Orthop 2004;125:191-9. [Crossref] [PubMed]
- Giannasi LC, Almeida FR, Magini M, et al. Systematic assessment of the impact of oral appliance therapy on the temporomandibular joint during treatment of obstructive sleep apnea: long-term evaluation. Sleep Breath 2009;13:375-81. [Crossref] [PubMed]
- Ueda H, Almeida FR, Chen H, et al. Effect of 2 jaw exercises on occlusal function in patients with obstructive sleep apnea during oral appliance therapy: a randomized controlled trial. Am J Orthod Dentofacial Orthop 2009;135:430.e1-7; discussion 430-1.
- Cunali PA, Almeida FR, Santos CD, et al. Mandibular exercises improve mandibular advancement device therapy for obstructive sleep apnea. Sleep Breath 2011;15:717-27. [Crossref] [PubMed]
- Marklund M, Stenlund H, Franklin KA. Mandibular advancement devices in 630 men and women with obstructive sleep apnea and snoring: Tolerability and predictors of treatment success. Chest 2004;125:1270-8. [Crossref] [PubMed]
- Milano F, Billi MC, Marra F, et al. Factors associated with the efficacy of mandibular advancing device treatment in adult OSA patients. Int Orthod 2013;11:278-89. [PubMed]
- Hoekema A, Doff MH, de Bont LG, et al. Predictors of obstructive sleep apnea-hypopnea treatment outcome. J Dent Res 2007;86:1181-6. [Crossref] [PubMed]
- Liu Y, Lowe AA, Orthodont D, et al. Cephalometric and physiologic predictors of the efficacy of an adjustable oral appliance for treating obstructive sleep apnea. Am J Orthod Dentofacial Orthop 2001;120:639-47. [Crossref] [PubMed]
- Suzuki K, Nakata S, Tagaya M, et al. Prediction of oral appliance treatment outcome in obstructive sleep apnoea syndrome: a preliminary study. B-ENT 2014;10:185-91. [PubMed]
- Yoshida K. Influence of sleep posture on response to oral appliance therapy for sleep apnea syndrome. Sleep 2001;24:538-44. [Crossref] [PubMed]
- Chung JW, Enciso R, Levendowski DJ, et al. Treatment outcomes of mandibular advancement devices in positional and nonpositional OSA patients. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2010;109:724-31. [Crossref] [PubMed]
- Lee CH, Jung HJ, Lee WH, et al. The effect of positional dependency on outcomes of treatment with a mandibular advancement device. Arch Otolaryngol Head Neck Surg 2012;138:479-83. [Crossref] [PubMed]
- Randerath WJ, Heise M, Hinz R, et al. An individually adjustable oral appliance vs continuous positive airway pressure in mild-to-moderate obstructive sleep apnea syndrome. Chest 2002;122:569-75. [Crossref] [PubMed]
- Walker-Engström ML, Ringqvist I, Vestling O, et al. A prospective randomized study comparing two different degrees of mandibular advancement with a dental appliance in treatment of severe obstructive sleep apnea. Sleep Breath 2003;7:119-30. [Crossref] [PubMed]
- Ng AT, Darendeliler MA, Petocz P, et al. Cephalometry and prediction of oral appliance treatment outcome. Sleep Breath 2012;16:47-58. [Crossref] [PubMed]
- Zhao M, Barber T, Cistulli P, et al. Computational fluid dynamics for the assessment of upper airway response to oral appliance treatment in obstructive sleep apnea. J Biomech 2013;46:142-50. [Crossref] [PubMed]
- Vroegop AV, Vanderveken OM, Dieltjens M, et al. Sleep endoscopy with simulation bite for prediction of oral appliance treatment outcome. J Sleep Res 2013;22:348-55. [Crossref] [PubMed]
- Pételle B, Vincent G, Gagnadoux F, et al. One-night mandibular advancement titration for obstructive sleep apnea syndrome: A pilot study. Am J Respir Crit Care Med 2002;165:1150-3. [Crossref] [PubMed]
- Dort LC, Hadjuk E, Remmers JE. Mandibular advancement and obstructive sleep apnoea: A method for determining effective mandibular protrusion. Eur Respir J 2006;27:1003-9. [Crossref] [PubMed]
- Banhiran W, Assanasen P, Nopmaneejumrudlers C, et al. Adjustable thermoplastic oral appliance versus positive airway pressure for obstructive sleep apnea. Laryngoscope 2018;128:516-22. [Crossref] [PubMed]
- Schmidt-Nowara W. Recent Developments in Oral Appliance Therapy of Sleep Disordered Breathing. Sleep Breath 1999;3:103-6. [Crossref] [PubMed]
- de Almeida FR, Bittencourt LR, de Almeida CI, et al. Effects of mandibular posture on obstructive sleep apnea severity and the temporomandibular joint in patients fitted with an oral appliance. Sleep 2002;25:507-13. [Crossref] [PubMed]


