Impact of 3D printing on the surgical management of tracheal stenosis associated to pulmonary sling: a case report
Introduction
Congenital tracheal stenosis (CTS) is rare malformation frequently associated with pulmonary sling (PS) and requiring surgical approach (1). Preoperative evaluation is made by different diagnostic studies in order to define the correct anatomy. Different surgical techniques have been described for the treatment of tracheal stenosis, but slide tracheoplasty (ST) has showed to improve the outcomes, especially in case of complex anatomy (2).
In the recent years, three-dimensional (3D) printing, producing 3D anatomical model from routinely radiologic exams was introduced in biomedical field and (3) currently is considered to be one the promising tool to understand the relationships of thoracic organs with their surrounding structures (4).
In this case report we describe the use of 3D printing technology after an unsuccessful surgical treatment of CTS associated to PS and how this technology could influence the surgical practice. For the best of our knowledge, 3D printing was never used before in a case of CTS.
Case presentation
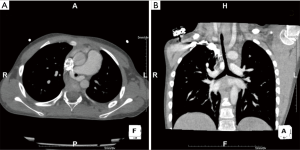
A 6-year-old boy was referred to our unit from a foreign country because diagnosed to have PS and CTS by chest computed tomography (CT). The anamnesis revealed dyspnoea and reduced exercise tolerance respect to the children of same age (from birth). No apparent life-threatening events were reported by the parents. Weight and height were 17.2 kilograms and 112 centimetres respectively. Oxygen saturation was 92%. Stridor was not present. CT scan showed the presence of left PS encircling the trachea. The trachea appeared stenotic from larynx to carina. Internal diameter at the narrowest point was measured to be 1.5 millimeters (mm) and this value was confirmed by preoperative rigid bronchoscopy. The length of the stenotic tract was measured to be 8 cm at CT scan (Figure 1). No bronchopulmonary associated malformations were present.
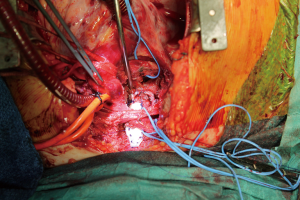
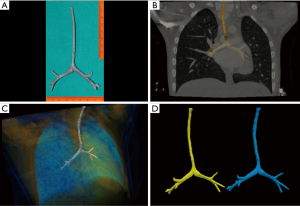
The tracheal team proposed surgical correction by ST and left pulmonary repositioning. Operation was made under general anesthesia and cardiopulmonary bypass. Ten complete tracheal rings were present. The left pulmonary artery was implanted on the pulmonary trunk by 6/0 polypropylene (Ethicon, USA) running suture. Afterward tracheal mobilisation (a “conditio sine qua non” to a successful ST) was difficult with risk of high anastomotic tension. Tracheal stenosis was hence approached by ST for the lower two tracheal third and enlargement with costal cartilage patch (Figure 2) for the upper segment. However postoperative anastomotic dehiscence occurred 2 weeks after surgery both in the upper and lower segment of the reconstructed tracheal, requiring multiple endoscopic re-interventions with stent placement. The child developed afterwards arteriovenous pulmonary malformations and died for severe haemoptysis after a prolonged in-hospital stay. A mortality and morbidity review was made to discuss this case. 3D printing technology was proposed to have a detailed definition of the patient’s anatomy. To build the 3D model, images analysis procedure was performed on the entire CT dataset as 3D data volume using a custom operator independent algorithm, able to perform airways segmentation and measurement (5). To extract the airways path geometry we applied the following three procedures: airways mask computation, computation of a hierarchical binary tree defining the airways segments, and computing lumen edge for all bronchial segments. To define the edge of trachea in a 3D rendered scene of the volume and provide 3D printable stereo lithography (STL) file format, we generated a polygonal mesh using a marching cubes algorithm. A one to one 3D model of the patient’s trachea was finally printed. The model (Figure 3) was showed to the surgeon to which was asked if, having it preoperatively, he would have changed the surgical strategy. Answer was that, considering the model, a complete enlargement with a patch would be more appropriate instead ST. Since that case, use of 3D printing for complex tracheal and cardiac cases are built at our institution and a clinical and research program involving 3D printing is currently in progress.
Comments
CTS is rare lesions considered to increase mortality risk of PS. The complexity is due to the dimension of the children’s trachea that can be very small especially in the neonates (1-8). Management by a dedicated tracheal team and ST have been considered a breakthrough in the improvement of the outcomes (2). However, as other authors have stated (6), “one slide cannot fit all”, the different anatomical patterns of tracheal stenosis make standardization of the surgical techniques difficult. The use of 3D printing has been demonstrated to be beneficial instead a bidimensional conventional exams, even when reconstructed three-dimensionally on the computer screen (4,5). The advantage of 3D printing lies precisely in the possibility to see and touch the model miming what will appear on operative field, manipulate it or simulating the surgical technique. In our case, at patient’s admission we did not have the time for preoperative construction of the model (the models are currently built by a non-institutional service requiring at least 3 weeks for their production) and we based our evaluation on the conventional bi-dimensional images of the CT scan that showed a pattern of severe long segmental tracheal stenosis, confirmed subsequently by the bronchoscopic control.
At surgery, the difficulties in the tracheal mobilisation do not permitted us to perform a full-length ST, hence we used it for the tracheal lower two-third enlarging the upper one with a costal cartilage patch. This choice, we believe, gave to the patient the cumulative risk of two surgical techniques, with dehiscence as the most dangerous one and the dramatic postoperative course confirmed our hypothesis. In order to improve subsequent outcomes, the case was discussed by the multidisciplinary tracheal team, and the use 3D printing was suggested on the base of the encouraging result described in the literature with its use (4,5,7). The necessity of a more specific knowledge of the anatomical pattern of the cases considered to be complex and the better technique to approach those cases, rise in our practice from the growing number of reports about favourable result by conservative management of CTS associate to PS (8). We are fully aware that is impossible by our experience, to demonstrate that having 3D technology there will be surely an improvement of the result in this case, nor we have at this time scientific data to compare this result with another one. Our experience permits to “speculate” that the most complicated the cases are, the most innovative diagnostic tools are required to define surgical strategy and hence improve the result. Considering the high cost of the technology, several refinements are still required to justify the routinely use of 3D printing (i.e., the best materials that “mime” the tissues) but at the moment 3D printing can be surely considered an important tool to improve surgical decision-making, surgical learning curve or development of new surgical techniques.
In conclusion, we confirm the use utility of 3D printing in the management of congenital thoracic malformations and in our case in CTS associate to PS.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the parents to publish this manuscript and any accompanying images.
References
- Manning PB, Rutter MJ, Lisec A, et al. One slide fits all: the versatility of slide tracheoplasty with cardiopulmonary bypass support for airway reconstruction in children. J Thorac Cardiovasc Surg 2011;141:155-61. [Crossref] [PubMed]
- Kocyildirim E, Kanani M, Roebuck D, et al. Long-segment tracheal stenosis: slide tracheoplasty and a multidisciplinary approach improve outcomes and reduce costs. J Thorac Cardiovasc Surg 2004;128:876-82. [Crossref] [PubMed]
- Kurenov SN, Ionita C, Sammons D, et al. Three-dimensional printing to facilitate anatomic study, device development, simulation, and planning in thoracic surgery. J Thorac Cardiovasc Surg 2015;149:973-9.e1. [Crossref] [PubMed]
- Schmauss D, Haeberle S, Hagl C, et al. Three-dimensional printing in cardiac surgery and interventional cardiology: a single-centre experience. Eur J Cardiothorac Surg 2015;47:1044-52. [Crossref] [PubMed]
- Bernardeschi I, Della Latta D, Di Girolamo GL, et al. An Operator Independent Method for Bronchial Tree Analysis from Trachea to the Small Airways Using Volumetric Multi-Detector Computed Tomography. J Med Imaging Health Inform 2016;6:170-6. [Crossref]
- Speggiorin S, Elliott MJ. Is slide tracheoplasty alone enough to improve the surgical outcome? J Thorac Cardiovasc Surg 2011;142:475. [Crossref] [PubMed]
- Son KH, Kim KW, Ahn CB, et al. Surgical Planning by 3D Printing for Primary Cardiac Schwannoma Resection. Yonsei Med J 2015;56:1735-7. [Crossref] [PubMed]
- Huang SC, Wu ET, Wang CC, et al. Surgical management of pulmonary artery sling: trachea diameter and outcomes with or without tracheoplasty. Pediatr Pulmonol 2012;47:903-8. [Crossref] [PubMed]


