Spread through air spaces—novel pattern of cancer progression
Despite the proliferation of antismoking campaigns and lung cancer screening by computed tomography, lung cancer remains the leading cause of cancer death worldwide. Because of the anatomical features of the lung, the growth patterns of lung malignancies differ from malignancies of other sites. The patterns of lung cancer progression are cancer spread via vascular, lymphatic, or alveolar spaces (1). These are related to the biological behavior of the lung tumor. Regarding lung cancer prognosis, histopathological findings that include grade of differentiation (2), pleural invasion (3,4), and lymphovascular invasion (5,6) have been reported to be prognostic factors. The spread of lung cancer to the alveolar spaces was recently reported as a novel pattern of cancer progression, and reports on lung adenocarcinoma have shown that cancer spread through the air spaces (STAS) is a significant risk factor for recurrence and a poor prognostic factor for overall survival (1,7-15) (Table 1). As an aggressive manifestation of lung cancer, STAS was introduced as a new concept for lung adenocarcinoma in the 2015 World Health Organization (WHO) classification (16). WHO classification defined STAS as “micropapillary clusters, solid nests, or single cells spreading within air spaces beyond the edge of the main tumor” (16).
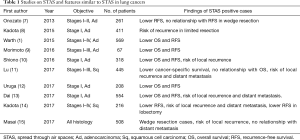
Full table
The 1995 Atlas of Tumor Pathology recognized aerogenous spread as the presence of isolated clusters of tumor cells in the alveolar space (17), but at that time, aerogenous spread was underrated and had not been well studied. In 2015, Kadota et al. revealed that STAS was a significant risk factor for recurrence in patients with ≤2-cm stage I lung adenocarcinoma who underwent limited resection, wedge resection, or segmentectomy (8). Interestingly, they also showed that STAS was not related to recurrence in patients who underwent lobectomy. Onozato et al. reported that patients with lung adenocarcinomas and tumor islands (alternative term for “STAS”), which are large clusters of tumor cells in alveolar spaces, had a significantly worse prognosis than patients with lung adenocarcinomas without tumor islands (7). They showed that adenocarcinomas with tumor islands were more likely to be found in smokers, to show predominant solid or micropapillary growth patterns, and tended to have KRAS mutations. Furthermore, Warth et al. evaluated 569 resected lung adenocarcinomas and found that 288 of them (50.6%) showed STAS. They found that STAS was detected at high rates in men and in patients with adenocarcinomas with wild-type epidermal growth factor receptors, lymph node metastasis, distant metastasis, and advanced-stage lung cancer (1). Morimoto et al. investigated adenocarcinomas with a micropapillary component and studied the relationship between free tumor cell clusters and outcome (9). Instead of the term “STAS”, they described “free tumor clusters (FTC)” and explained that FTC did not contain solid nests or single cells. Locoregional recurrence was frequently observed in patients with FTC and in those patients with shorter recurrence-free survival. They concluded that FTC had a negative impact on the postoperative outcome of patients with micropapillary-positive adenocarcinomas.
STAS is related to recurrence and survival in patients with squamous cell lung carcinoma. Lu et al. investigated 445 cases of surgically resected stages I to III squamous cell lung carcinoma and identified STAS in specimens from 30% of the patients (11). Although patients with STAS had higher rates of recurrence and cancer-specific death than patients without STAS, the difference in overall survival between patients with and without STAS was not significant. Kadota et al. investigated Japanese patients with squamous cell lung carcinoma and confirmed the results of Lu et al. (14).
With advances in the detection of small-sized lung cancers, the demands for surgical procedures such as limited resection, wedge resection, and segmentectomy have increased. In 1995, the Lung Cancer Study Group investigated small (≤3 cm) T1N0 lung cancers and found that limited resection was associated with a higher risk of recurrence than lobectomy (18), and that lobectomy provided superior outcomes compared with limited resection. Lobectomy has subsequently been regarded to be the standard surgical procedure for lung cancers.
Recurrence, especially locoregional recurrence, remains a serious concern with regard to the effectiveness of limited resection. An adequate margin and absence of residual tumor cells after surgery are mandatory for preventing locoregional recurrence. Yoshida et al. reported on three patients who developed recurrence at the surgical margins (19). These patients were participants in a trial of limited resection (20) for noninvasive type lung cancer with a good prognosis, but recurrent tumor developed at the surgical margins. To avoid recurrence at the surgical margin after wedge resection, the investigators washed the stapler cartridges used for the resection with 200 mL of saline solution, and the lavage fluid was examined cytologically (20). Examination of frozen sections of all the staple lines marking the surgical margin during surgery would not be realistic. Intraoperative cytological examination of lavage fluid is the only option for checking the surgical margin. The investigators suggested that cancer cells might spread along the airways or blood vessels (19). It is possible that, in the case with STAS, cancer cells might persist in surgical margin.
STAS could be associated with local recurrence after limited resection. Other investigators whose work was described earlier in this article (7,8,15) found that lobectomy reduced the risk of locoregional recurrence in patients with STAS. Masai et al. performed multivariate analysis that revealed that STAS and width of the surgical margin were significant risk factors of recurrence (15). Furthermore, they concluded that STAS and a <1-cm width of the surgical margin are significant risk factors for local recurrence in patients with early-stage lung cancer undergoing limited resection. The choice of lobectomy over limited resection for lung cancer might be supported by the STAS phenomenon.
The mechanisms involved in the spread of cancer cells to air spaces are largely unknown. In terms of cell connections, a cell adhesion molecule such as epithelial (E)-cadherin or ICAM is thought to be associated with STAS. However, the decreased expression of epithelial (E)-cadherin has been reported to be unrelated to STAS (21). STAS might occur as a result of a surgical procedure or tumor biopsy, which leads to disruption of the resected tumor by manipulation. To examine this hypothesis, we determined the proportions of patients who developed STAS after different surgical procedures. We could not find differences in the rates of STAS between surgical procedures (10). However, it is speculated that preoperative biopsy procedures might lead to STAS.
There is a possibility that STAS can occur as an artifact during the processing of surgical specimens for histopathological evaluation. One report described the concept of “spreading through a knife surface (STAKS)” (22). STAKS is considered to be an artifact resulting from specimen processing. Since, in general, the steps in processing tissues and making slides are not standardized or recorded, verifying that STAKS can lead to observations of STAS is difficult. Despite the opinions that STAS is an artifact, many recent reports have confirmed the significant effects of STAS on the recurrence of lung cancer and survival. Kadota et al. described detailed methods for differentiating STAS from alveolar macrophages and artifacts (8,14). Dai et al. used the methods of Kadota and found similar results (13). I think that STAS is not artifact.
Dai et al. have reported that patients with adenocarcinomas ranging in size from <2 to 3 cm that showed STAS had an unfavorable outcome similar to the outcome of stage IB patients with or without STAS. The differences between overall survival and recurrence-free survival in patients with ≤2-cm adenocarcinomas with and without STAS were not significant (13). The authors suggested that STAS might be a factor to include in a staging system. While the TNM classification categorizes the tumor into stages based on the anatomical extent of tumor, histopathological factors such as lymphatic, venous, and perineural invasion are included in staging systems (23). In lung cancer, pleural invasion is only the histopathological factor that affects the T factor. However, pleural invasion is difficult to diagnose by hematoxylin and eosin staining, and instead should be evaluated on tissue preparations stained for elastic tissues. By contrast, STAS can be diagnosed on routine preparations stained by hematoxylin and eosin, indicating that diagnosing STAS should be easier than diagnosing pleural invasion.
How do we use the results of STAS in lung cancer surgery? In patients with small, i.e., 3 cm or less in size, lung cancers, STAS should be investigated to rule out the use of limited resection. Thus, the preoperative diagnosis of STAS is critical for selecting surgical procedures. If STAS can be identified or predicted before surgery, limited resection, which leads to higher risk of recurrence in patients with STAS, should be avoided. However, the preoperative identification of STAS is challenging. Moreover, STAS identification on intraoperative frozen sections is difficult. A biopsy specimen during surgery that contains normal lung parenchyma including the tumor should be a requirement. At this point, if the patients who underwent limited resection are found STAS, meticulous radiological follow-up of recurrence is needed.
In conclusion, Dai et al. showed that patients with stage IA adenocarcinomas ranging in size from <2 to 3 cm showing STAS had an unfavorable outcome similar to the outcome of stage IB patients with or without STAS. If limited resection is performed for stage IA lung cancer, thoracic surgeons should rule out STAS irrespective of the tumor size.
Acknowledgements
None.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
References
- Warth A, Muley T, Kossakowski CA, et al. Prognostic impact of intra-alveolar tumor spread in pulmonary adenocarcinomas. Am J Surg Pathol 2015;39:793-801. [Crossref] [PubMed]
- Ichinose Y, Yano T, Asoh H, et al. Prognostic factors obtained by a pathologic examination in completely resected non-small-cell lung cancer. An analysis in each pathologic stage. J Thorac Cardiovasc Surg 1995;110:601-5. [Crossref] [PubMed]
- Manac’h D, Riquet M, Medioni J, et al. Visceral pleural invasion by non-small cell lung cancer: an underrated bad prognostic factor. Ann Thorac Surg 2001;71:1088-93. [Crossref] [PubMed]
- Shimizu K, Yoshida J, Nagai K, et al. Visceral pleural invasion is an invasive and aggressive indicator of non-small cell lung cancer. J Thorac Cardiovasc Surg 2005;130:160-5. [Crossref] [PubMed]
- Bodendorf MO, Haas V, Laberke HG, et al. Prognostic value and therapeutic consequences of vascular invasion in non-small cell lung carcinoma. Lung Cancer 2009;64:71-8. [Crossref] [PubMed]
- Shoji F, Haro A, Yoshida T, et al. Prognostic significance of intratumoral blood vessel invasion in pathologic stage IA non-small cell lung cancer. Ann Thorac Surg 2010;89:864-9. [Crossref] [PubMed]
- Onozato ML, Kovach AE, Yeap BY, et al. Tumor islands in resected early stage lung adenocarcinomas are associated with unique clinicopathological and molecular characteristics and worse prognosis. Am J Surg Pathol 2013;37:287-94. [Crossref] [PubMed]
- Kadota K, Nitadori J, Sima CS, et al. Tumor spread through air spaces is an important pattern of invasion and impacts the frequency and location of recurrences after limited resection for small stage I lung adenocarcinomas. J Thorac Oncol 2015;10:806-14. [Crossref] [PubMed]
- Morimoto J, Nakajima T, Suzuki H, et al. Impact of free tumor clusters on prognosis after resection of pulmonary adenocarcinoma. J Thorac Cardiovasc Surg 2016;152:64-72.e1. [Crossref] [PubMed]
- Shiono S, Yanagawa N. Spread through air spaces is a predictive factor of recurrence and a prognostic factor in stage I adenocarcinoma. Interact Cardiovasc Thorac Surg 2016;23:567-72. [Crossref] [PubMed]
- Lu S, Tan KS, Kadota K, et al. Spread through air spaces (STAS) is an independent predictor of recurrence and lung cancer–specific death in squamous cell carcinoma. J Thorac Oncol 2017;12:223-34. [Crossref] [PubMed]
- Uruga H, Fujii T, Fujimori S, et al. Semiquantitative assessment of tumor spread through air spaces (STAS) in early-stage lung adenocarcinomas. J Thorac Oncol 2017;12:1046-51. [Crossref] [PubMed]
- Dai C, Xie H, Su H, et al. Tumor spread through air spaces affects the recurrence and overall survival in patients with lung adenocarcinoma >2 to 3 cm. J Thorac Oncol 2017;12:1052-60. [Crossref] [PubMed]
- Kadota K, Kushida Y, Katsuki N, et al. Tumor spread through air spaces is an independent predictor of recurrence-free survival in patients with resected lung squamous cell carcinoma. Am J Surg Pathol 2017;41:1077-86. [Crossref] [PubMed]
- Masai K, Sakurai H, Sukeda A, et al. Prognostic impact of margin distance and tumor spread through air spaces in limited resection for primary lung cancer. J Thorac Oncol 2017;12:1788-97. [Crossref] [PubMed]
- Travis WD, Brambilla E, Nicholson AG, et al. The 2015 World health organization classification of lung tumors: Impact of genetic, clinical and radiologic advances since the 2004 classification. J Thorac Oncol 2015;10:1243-60. [Crossref] [PubMed]
- Colby TV, Koss MN, Travis WD. Tumors of the lower respiratory tract. In: Rosai J, editor. Atlas of tumor pathology. Washington, DC: Armed Forces Institute of Pathology, 1995:112-6.
- Ginsberg RJ, Rubinstein LV. Randomized trial of lobectomy versus limited resection for T1 N0 non-small cell lung cancer. Lung Cancer Study Group. Ann Thorac Surg 1995;60:615-22; discussion 622-3. [Crossref] [PubMed]
- Yoshida J, Ishii G, Yokose T, et al. Possible delayed cut-end recurrence after limited resection for ground-glass opacity adenocarcinoma, intraoperatively diagnosed as Noguchi type B, in three patients. J Thorac Oncol 2010;5:546-50. [Crossref] [PubMed]
- Yoshida J, Nagai K, Yokose T, et al. Limited resection trial for pulmonary ground-glass opacity nodules: fifty-case experience. J Thorac Cardiovasc Surg 2005;129:991-6. [Crossref] [PubMed]
- Jin Y, Sun PL, Park SY, et al. Frequent aerogenous spread with decreased E-cadherin expression of ROS1-rearranged lung cancer predicts poor disease-free survival. Lung Cancer 2015;89:343-9. [Crossref] [PubMed]
- Blaauwgeers H, Flieder D, Warth A, et al. A prospective study of loose tissue fragments in non–small cell lung cancer resection specimens. An alternative view to “Spread Through Air Spaces”. Am J Surg Pathol 2017;41:1226-30. [Crossref] [PubMed]
- Brierley JD, Gospodarowicz MK, Wittekind C. TNM classification of malignant tumours. 8th ed. New York: John Wiley & Sons, 2017:1-15.


