Diagnostic accuracy of interferon-gamma in pericardial effusions for tuberculous pericarditis: a meta-analysis
Introduction
With the widespread application of cardiovascular imaging approaches, pericardial effusion is being increasingly recognized (1). Among the potential reasons for pericardial effusion, tuberculous pericarditis is one of the more frequent aetiologies, especially in developing countries (2). The mortality from tuberculous pericarditis ranges from 7% to 40% (2). Timely and accurate identification of tuberculous pericarditis is crucial because it is the basis for the selection of the anti-tuberculosis therapy approach. Currently, the diagnosis of tuberculous pericarditis is usually based on culture, histological examination and Ziehl-Neelsen staining (3). However, pericardial effusion culture is time-consuming and the sensitivity is not satisfactory. Histological examination and Ziehl-Neelsen staining have high specificity, but the sensitivity is greatly affected by the experience of the observers. In addition, sampling error is also a problem.
Interferon-gamma is a type of cytokine produced by Th1 cells in response to Mycobacterium tuberculosis (4). During the past few years, increasing numbers of studies have proved that interferon-gamma is a useful diagnostic marker for tuberculosis. For example, a meta-analysis showed that tests for interferon-gamma in pleural fluid has extremely high sensitivity and specificity for tuberculous pleurisy (5). In addition, interferon-gamma in cerebrospinal fluid (CSF) is also a useful biomarker for tuberculous meningitis (6). To date, several studies have investigated the diagnostic accuracy of pericardial effusion interferon-gamma for tuberculous pericarditis, but the results have varied. Here, we performed a meta-analysis to investigate the diagnostic accuracy of testing for interferon-gamma for tuberculous pericarditis in patients with pericardial effusion.
Methods
Database and literature search strategies
This study was performed in accordance with the Preferred Reporting Items for Systematic reviews and Meta-analyses (PRISMA) (7). The PubMed and EMBASE databases were searched to identify potential studies (last search time: March 25, 2017). The search algorithm in PubMed was as follows: [“Pericarditis, Tuberculous” (mesh) OR Pericarditis] AND [“Interferon-gamma” (nm) OR interferon OR IFN]. In EMBASE, the search algorithm was as follows: ‘pericarditis’/exp OR pericarditis AND (‘interferon’/exp OR interferon), and the publication type was restricted to articles and short surveys. A manual search of the references listed in the included articles was also performed.
Study selection and data extraction
Studies investigating the diagnostic accuracy of tests of interferon-gamma for tuberculous pericarditis in patients with pericardial effusion were included in this meta-analysis. The exclusion criteria of this meta-analysis were as follows: (I) non-English publications; (II) animal studies; (III) reviews; and (IV) unable to construct a 2-by-2 table from the reported data. Two reviewers independently reviewed the titles and abstracts of the retrieved studies and identified the potential eligible studies. Full-text review was performed if necessary.
Two reviewers independently extracted the following data from the included studies: first author’s name, year of publication, country of subjects, sample sizes, characteristics of the study population (age, sex, and HIV infection), test assays for interferon-gamma, type of data collection (prospective or retrospective), reference standards, thresholds of interferon-gamma and its corresponding sensitivity and specificity.
Quality assessment
The revised Quality Assessment of Diagnostic Accuracy Studies (QUADAS-2) was used to assess the quality of the eligible studies (8). The quality assessment was independently performed by two reviewers, and any disagreement was resolved by consensus.
Statistical analysis
The overall diagnostic sensitivity and specificity of the tests of interferon-gamma for tuberculous pericarditis were pooled by a bivariate model (9). Forest plots for sensitivity and specificity, as well as summary receiver operating characteristic (sROC) curves, were generated using RevMan 5.3. (Cochrane Library, London, UK). All analyses were performed in Stata 12.0 (Stata Corp LP, College Station, TX, USA), using the command midas. A P value less than 0.05 was defined as statistically significant.
Results
Summary of the included studies
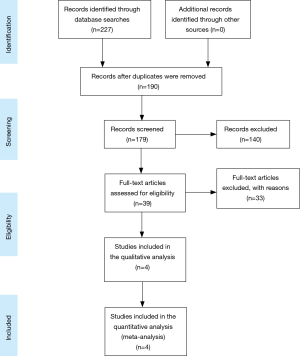
Figure 1 shows a flowchart of study selection. Five studies were included after literature screening. Two studies were from the same cohort (10,11), and only the one with a larger sample size was included. Therefore, four studies (11-14) were included in the present meta-analysis, and a summary of the included studies is listed in Table 1. Three of the four included studies were performed in South Africa (11-13), and one was performed in Iran (14). The sample sizes ranged from 38 to 233, with a total sample size of 488. The average prevalence of tuberculous pericarditis was 63%. All of the included studies were prospective in design, and the study populations were patients with pericardial effusion. The interferon-gamma test method in two studies (11,12) was an enzyme-linked immunosorbent assay (ELISA); one (13) used an InterGam ultrasensitive rapid immuno-suspension assay (IRISA), and one did not report the test method (14). Most of the studies used Ziehl-Neelsen staining, culture, histological examination and anti-tuberculous therapy response as the diagnostic reference for tuberculous pericarditis.

Full table
Major findings of the included studies
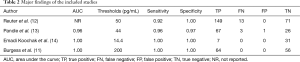
Table 2 lists the major findings of the included studies. Generally, the diagnostic accuracy of tests of interferon-gamma for tuberculous pericarditis is extremely high. Three studies (11,13,14) evaluated the diagnostic accuracy of interferon-gamma for tuberculous pericarditis using receiver operating characteristic (ROC) curve analysis, and the areas under the curve (AUCs) ranged from 0.96 to 1.00. Although the thresholds used in four studies ranged from 14.4 to 200 pg/mL, the sensitivities and specificity were homogeneous, ranging from 0.92 to 1.00 and 0.97 to 1.00, respectively.
Full table
Quality of the included studies
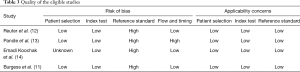
Table 3 lists the results of quality assessment of the included studies. All of the studies, except one (14), were prospective and consecutively enrolled the study cohort with uniform inclusion and exclusion criteria. Therefore, the patient selection domain in these studies was labelled low. The reference standard domain of all studies was labelled high because of differential or partial verification bias. The flow and timing domain in one study was labelled high because not all subjects were included in the analysis. All domains for applicability concerns were labelled low because they matched the review question well.
Full table
Diagnostic accuracy of interferon-gamma for tuberculous pericarditis
Figure 2 is a forest plot of sensitivity and specificity of tests of interferon-gamma for tuberculous pericarditis. The overall sensitivity and specificity of tests for interferon-gamma was 0.97 [95% confidence interval (CI): 0.87–0.99] and 0.99 (95% CI: 0.74–1.00), respectively. The positive likelihood ratio (PLR), negative likelihood ratio (NLR) and diagnostic odds ratio (DOR) were 187 (95% CI: 3–12,542), 0.03 (95% CI: 0.01–0.14) and 5,623 (95% CI: 56–569,288), respectively. I2 across all eligible studies was 0.00 (95% CI: 0–100).

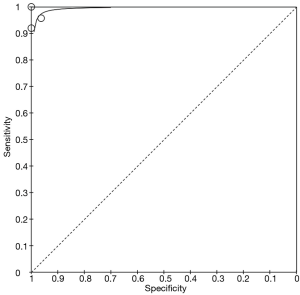
Figure 3 is a sROC for interferon-gamma, with an AUC of 1.00 (95% CI: 0.99–1.00).
Discussion
In this study, we found the following: (I) to date, four studies have investigated the diagnostic accuracy of tests of interferon-gamma for tuberculous pericarditis; (II) the quality of the included studies was generally high, and the major design weaknesses of included studies were differential or partial verification bias; and (III) the diagnostic accuracy of tests for interferon-gamma in pericardial effusion were extremely high, with an overall sensitivity and specificity of 0.97 and 0.99, respectively. To the best of our knowledge, this is the first meta-analysis investigating the diagnostic accuracy of interferon-gamma for tuberculous pericarditis. Notably, the study subjects in this meta-analysis were highly homogeneous, and all of the studies were prospective in design. Therefore, the results of the present studies are reliable.
Sensitivity, specificity and AUC under the sROC are three key characteristics reflecting the diagnostic accuracy of an index test; however, their interpretation is not straightforward. In contrast, NLR and PLR are more clinically meaningful. It is generally accepted that a PLR above 10 and an NLR below 0.1 are adequate to identifying and rule out target diseases, respectively (15). The present study found that the PLR and NLR for interferon-gamma were 187 and 0.03, indicating that tests for interferon-gamma, even when used alone, are adequate for identifying or ruling out tuberculous pericarditis. Therefore, we concluded that pericardial effusion interferon-gamma is a strong and reliable biomarker for tuberculous pericarditis diagnosis.
It is well recognized that the sensitivity and specificity of an index test are greatly affected by the threshold used for defining a target disease. The thresholds used in the included studies were variable (ranging from 14.4 to 200 pg/mL), but the sensitivity and specificity were homogeneous. These results may be attributed to the fact that the levels of interferon-gamma in tuberculous pericarditis and non-tuberculous pericarditis are dramatically different; there is no grey zone between these two groups. Indeed, in one of the included studies (12): the mean interferon-gamma level in cases of non-tuberculous pericarditis was 27 pg/mL, while in patients with tuberculous pericarditis, the mean level was approximately 700 pg/mL.
At present, several diagnostic biomarkers for tuberculous pericarditis have been identified. Among the available biomarkers, adenosine deaminase (ADA) in pericardial effusion seems to be the most promising one. A recently published meta-analysis indicated that the diagnostic sensitivity, specificity, PLR and NLR of ADA are 0.90, 0.86, 5.90 and 0.15, respectively (16). Therefore, it seems that the diagnostic accuracy of ADA is inferior to interferon-gamma. This hypothesis was supported by a recently published head-to-head comparison study (13). Because tests for interferon-gamma have extremely high diagnostic accuracy for tuberculous pericarditis, it seems that ADA has no capability to improve its diagnostic performance. The major limitation of testing for interferon-gamma is its high cost and lack of a broadly accepted discriminative threshold (17,18).
The present study has some limitations. First, the number of studies included in the present meta-analysis is only four, and three of the four included studies were performed in South Africa, a country with a high prevalence of tuberculosis (19). As the disease spectrum in patients with pericardial effusion may be affected by the prevalence of tuberculosis, the conclusions of the present study may not be generalizable to other areas. Second, due to the small number of included studies, subgroup and publication bias analyses were not performed.
Taken together, the current evidence strongly supports a potential role of interferon-gamma for tuberculous pericarditis diagnosis. However, because the total sample size in the present work is small, and most of the subjects were from South Africa, further studies with large sample sizes and a greater variety of subjects are needed to evaluate the diagnostic accuracy of tests of interferon-gamma for tuberculous pericarditis.
Acknowledgements
We thank Dr. Tian-Song Zhang for his statistical assistance.
Funding: This work was supported by a grant from the Foundation of General Hospital of Ji’nan Military Region (2016BS02).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Vakamudi S, Ho N, Cremer PC. Pericardial Effusions: Causes, Diagnosis, and Management. Prog Cardiovasc Dis 2017;59:380-8. [Crossref] [PubMed]
- Mayosi BM, Wiysonge CS, Ntsekhe M, et al. Mortality in patients treated for tuberculous pericarditis in sub-Saharan Africa. S Afr Med J 2008;98:36-40. [PubMed]
- Syed FF, Mayosi BM. A modern approach to tuberculous pericarditis. Prog Cardiovasc Dis 2007;50:218-36. [Crossref] [PubMed]
- Cooper AM, Dalton DK, Stewart TA, et al. Disseminated tuberculosis in interferon gamma gene-disrupted mice. J Exp Med 1993;178:2243-7. [Crossref] [PubMed]
- Jiang J, Shi HZ, Liang QL, et al. Diagnostic value of interferon-gamma in tuberculous pleurisy: a metaanalysis. Chest 2007;131:1133-41. [Crossref] [PubMed]
- Juan RS, Sanchez-Suarez C, Rebollo MJ, et al. Interferon gamma quantification in cerebrospinal fluid compared with PCR for the diagnosis of tuberculous meningitis. J Neurol 2006;253:1323-30. [Crossref] [PubMed]
- Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg 2010;8:336-41. [Crossref] [PubMed]
- Whiting PF, Rutjes AW, Westwood ME, et al. QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med 2011;155:529-36. [Crossref] [PubMed]
- Reitsma JB, Glas AS, Rutjes AW, et al. Bivariate analysis of sensitivity and specificity produces informative summary measures in diagnostic reviews. J Clin Epidemiol 2005;58:982-90. [Crossref] [PubMed]
- Burgess LJ, Reuter H, Carstens ME, et al. Cytokine production in patients with tuberculous pericarditis. Int J Tuberc Lung Dis 2002;6:439-46. [PubMed]
- Burgess LJ, Reuter H, Carstens ME, et al. The use of adenosine deaminase and interferon-gamma as diagnostic tools for tuberculous pericarditis. Chest 2002;122:900-5. [Crossref] [PubMed]
- Reuter H, Burgess L, van Vuuren W, et al. Diagnosing tuberculous pericarditis. QJM 2006;99:827-39. [Crossref] [PubMed]
- Pandie S, Peter JG, Kerbelker ZS, et al. Diagnostic accuracy of quantitative PCR (Xpert MTB/RIF) for tuberculous pericarditis compared to adenosine deaminase and unstimulated interferon-gamma in a high burden setting: a prospective study. BMC Med 2014;12:101. [Crossref] [PubMed]
- Emadi Koochak H, Davoudi S, Salehi Omran A, et al. Diagnostic value of interferon-gamma assay in tuberculosis pericardial effusions: study on a cohort of Iranian patients. Acta Med Iran 2013;51:449-53. [PubMed]
- Deeks JJ, Altman DG. Diagnostic tests 4: likelihood ratios. BMJ 2004;329:168-9. [Crossref] [PubMed]
- Xie DL, Cheng B, Sheng Y, et al. Diagnostic accuracy of adenosine deaminase for tuberculous pericarditis: a meta-analysis. Eur Rev Med Pharmacol Sci 2015;19:4411-8. [PubMed]
- Porcel JM. Advances in the diagnosis of tuberculous pleuritis. Ann Transl Med 2016;4:282. [Crossref] [PubMed]
- Mutyaba AK, Ntsekhe M. Tuberculosis and the Heart. Cardiol Clin 2017;35:135-44. [Crossref] [PubMed]
- Glaziou P, Sismanidis C, Floyd K, et al. Global epidemiology of tuberculosis. Cold Spring Harb Perspect Med 2014;5:a017798. [Crossref] [PubMed]