Primary mediastinal leiomyoma: a rare case report and literature review
Introduction
Benign mesenchymal tumors of the mediastinum are rare, representing only 1% to 6% of all mediastinal masses. Moreover, leiomyomas have the least incidence of those tumors. Leiomyomas are benign smooth muscle tumors that are commonly encountered in the digestive or urogenital tract. Primary leiomyomas occurring in the mediastinum are extremely rare. They are usually slow-growing tumors and often detected incidentally on chest radiographs. Up to now, only about ten cases of primary mediastinal leiomyoma (PML) have been reported in English literature. In this case report, we describe a 3-year-old girl with a huge PML located in the anterior mediastinum with extension into the right hemi-thorax and left upper abdominal quadrant, who successfully underwent complete surgical tumor resection. To the best knowledge, this is the second case report of a PML in a child.
Case presentation
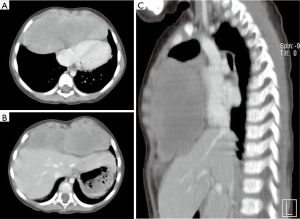
A 3-year-old girl presented with asymptomatic left upper quadrant abdominal mass was admitted to our institution. She had no history of perinatal or developmental problems. She was well-nourished, 90 cm in height, and 12.5 kg in weight. Physical examination revealed
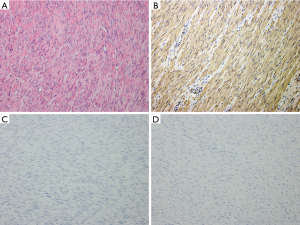
The mass was approached through a median sternotomy, which was found to be well encapsulated with no connection to the pericardium, lung, or diaphragm. No obvious feeding artery was found. Complete removal of the tumor was accomplished. Gross specimen examination revealed a 14 cm × 7 cm × 6 cm long mass with sporadic areas of cystic degeneration. Microscopic examination revealed a tumor composed of monomorphic spindle cells with neither nuclear atypia nor mitoses (Figure 2A). Immunohistochemical stains demonstrated the tumor to be strongly positive for smooth muscle actin (SMA), and negative for S-100 protein, as well as neuron specific enolase (NSE) (Figure 2B-D). The tumor was diagnosed as benign leiomyoma. Moreover, the patient underwent an uneventful recovery and was discharged on the 5th postoperative day. No evidence of tumor recurrence was observed during a 3-year follow-up.
Discussion
PML is extremely rare benign mesenchymal tumors, and up to the present has only been described in a few cases in the literature (1-10) (Table 1). According to some reports, most of PMLs were frequently found in middle-aged female patients (3,7). However, we found no gender differences in tumor onset through literature review. Although the onset ages ranges from child to adulthood, PML is not common in children. The pathogenesis of leiomyoma still remains obscure, estrogen and trauma theories have been suggested to play important roles (11). This child had no evidence of endocrine disturbance or trauma history, we argue that this tumor might be embryonic.
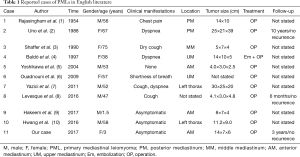
Full table
In this study, our case presented several diagnostic and managerial challenges. Preoperative enhanced CT imaging of the lesion indicated the following: (I) the solid tumor nature of the proliferation without obvious feeding artery; and (II) the atypical location in the anterior mediastinum with extension to the right hemithorax and left upper quadrant abdomen, together with irregular delimitation. A benign spindle cell neoplasm was diagnosed via fine-needle biopsy before surgery. Given the age of our patient, the diagnosis of neurilemmoma or solitary fibrous tumor was considered.
PML is generally quite large at the time of diagnosis owing to slow growth and relative lack of symptoms. The symptoms are mainly caused by compression of tumor on nearby vital structures, manifested as dyspnea, dysphagia, or superior vena cava syndrome (4). However, the patient we reported had no obvious symptoms with such a large tumor in the anterior mediastinum. The tumor had not been detected until the presentation of a left upper abdominal mass duo to the extension of the tumor was detected unexpectedly.
Surgical resection is still the most preferred and effective treatment for PMLs. Preoperative enhanced CT scan can reveal the size, location, blood supply and adjacent involvement of the tumor. For resection of giant mediastinal tumors, preliminary embolization of target vessels would be helpful in reducing the risk of catastrophic haemorrhage during operation (4). Although leiomyoma is often considered as benign tumor, strict follow-up was warranted because of the metastasis reported in the literature (12).
Conclusions
PML is extremely rare and has only been described in a few cases in the literature up to the present. Here, we report a rare case of PML occurring in a little girl, which serve as a supplement to the spectrum. Surgical resection would be a reasonable choice at the time of diagnosis. Despite its rarity, PML should be considered in the differential diagnosis of an unexplained mass in the mediastinum.
Acknowledgements
Funding: This work was supported by grants from National Natural Science Foundation of China to Dr. Lunxu Liu (No. 81372505).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient’s guardian for publication of this manuscript and any accompanying images.
References
- Rajasingham AS, Cooray GH. A large leiomyoma of the mediastinum. Br J Surg 1954;41:446-7. [Crossref] [PubMed]
- Uno A, Sakurai M, Onuma K, et al. A case of giant mediastinal leiomyoma with long-term survival. Tohoku J Exp Med 1988;156:1-6. [Crossref] [PubMed]
- Shaffer K, Pugatch RD, Sugarbaker DJ. Primary mediastinal leiomyoma. Ann Thorac Surg 1990;50:301-2. [Crossref] [PubMed]
- Baldó X, Sureda C, Gimferrer JM, et al. Primary mediastinal leiomyoma: an angiographic study and embolisation of the feeding vessels to improve the surgical approach. Eur J Cardiothorac Surg 1997;11:574-6. [Crossref] [PubMed]
- Yoshikawa S, Matsumura A, Okumura M, et al. A case of leiomyoma in the anterior mediastinum. J Jpn Assoc Chest Surg 2004;18:627-30. [Crossref]
- Ouadnouni Y, Achir A, Bekarsabein S, et al. Primary mediastinal leiomyoma: a case report. Cases J 2009;2:8555. [Crossref] [PubMed]
- Yazici U, Gülhan E, Yazici U, et al. A case of giant mediastinal leiomyoma. Turk J Gastroenterol 2011;22:656-7. [Crossref] [PubMed]
- Levesque MH, Aisagbonhi O, Digumarthy S, et al. Primary Paratracheal Leiomyoma: Increased Preoperative Diagnostic Specificity With Magnetic Resonance Imaging. Ann Thorac Surg 2016;102:e151-4. [Crossref] [PubMed]
- Hakeem ZA, Rathore SS, Wahid A. Rare mediastinal leiomyoma in a child. Gen Thorac Cardiovasc Surg 2017;65:415-7. [Crossref] [PubMed]
- Hwang YU, Kim SY, Lee BH, et al. Primary Mediastinal Leiomyoma Mimicking a Giant Mediastinal Cyst: A Case Report. J Korean Soc Radiol 2016;75:147-50. [Crossref]
- Matsuoka H, Nishio W, Sakamoto T, et al. Mediastinal angioleiomyoma. Ann Thorac Surg 2002;73:1653-4. [Crossref] [PubMed]
- Abramson S, Gilkeson RC, Goldstein JD, et al. Original report - Benign metastasizing leiomyoma: Clinical, imaging, and pathologic correlation. AJR Am J Roentgenol 2001;176:1409-13. [Crossref] [PubMed]


