Anesthesia and fast-track in video-assisted thoracic surgery (VATS): from evidence to practice
Introduction
Fast-track, or enhanced recovery after surgery (ERAS) is a concept of perioperative management that aims at shortening hospital stay in order to reduce patient morbidity and costs. It combines sophisticated, minimally invasive surgical techniques, preoperative patient optimization, and evidence-based clinical measures that minimize complications and fasten recovery. It was first introduced 20 years ago for colorectal surgery but has since been successfully applied to many other fields (hepatobiliary, vascular, urologic). The introduction of the video-assisted thoracoscopic surgery (VATS) has allowed development of such programmes in the thoracic setting. This has recently been linked to decreased in-hospital mortality (1).
Today, patients admitted for lobectomy are often discharged at home on the third postoperative day. To guarantee these results, many aspects of the perioperative management have been revised. Some of these, like preoperative carbohydrate loading, are often managed by surgeons and have been analyzed in other publications. Others, like prevention of postoperative nausea and vomiting (PONV) or intraoperative hypothermia, are shared with other surgical specialties and will not be discussed here. The ones that are unique to anesthesia in thoracic surgery will instead be reviewed in the following pages, according to the most recent scientific evidences and to our regular practice. This article will specifically focus on the goals of fast-track surgery, i.e., (I) reducing postoperative complications and (II) speeding recovery times.
Preoperative period
Careful preoperative risk assessment and optimization of home therapy are mandatory before lung surgery (2). These issues are out of the scope of this manuscript, but it is important to underline the necessity to elaborate a tailored strategy comprising both the intraoperative and postoperative anesthetic care ranging from premedication to analgesic therapy.
Premedication
Preoperative anxiety is fairly common and has a dramatic impact on the patient’s personal experience. Furthermore, evidence suggests a correlation with postoperative pain (3). Patient-doctor communication is paramount and should be actively pursued, with a special focus on the clinical path undertaken. Analgesics and sedatives can be prescribed during the preoperative evaluation.
In the operative room, anxiolytics or opioids are often administered to increase patient’s comfort while procedures such as vein cannulation or regional anesthesia are performed (4). Controversy arises in the choice of agents to be used, especially when focusing on ERAS goals. Long-acting drugs need to be avoided as they defer postoperative recovery (5). They have been linked to psychomotor disability, reduced mobilization, and late refeeding. Inability to take fluids or food per os is related to delays in full recovery (4). Short-acting drugs such as midazolam are therefore usually preferred. Despite its short-acting profile, even midazolam has shown residual effects during longer evaluation time frames (6), and clinically, it has been associated to late discharge from the post-anesthesia care unit (PACU) (7) and lower scores on psychomotor performance tests (8). Its routine use should be avoided, especially in the elderly (9), and reserved for selected cases. Protocols aimed at reducing the duration of post-anesthesia care are already implementing this idea (10). In general, all benzodiazepines should be withheld.
Intraoperative period
Management of general anesthesia
Intraoperative pharmacologic management should be tailored to the goals of fast-track surgery, i.e., rapid recovery times and minimal side effects. Both inhalatory agents and total intravenous anesthesia have been successfully used for thoracic surgery. In order to minimize PONV (11), propofol [induction: 1.5–2.5 mg/kg; maintenance: 4–12 mg/kg/h or 2–6 µg/mL Cpl in target-controlled infusion (TCI) (12)] is often preferred (13). Lately, however, its safety profile during pulmonary surgery has been questioned. One-lung ventilation (OLV) is known to be potentially harmful in terms of alveolar mechanical stress, resulting in proinflammatory cytokines release (14). Anesthetic drugs may have an impact on such response and have been evaluated comparatively: both propofol (15) and halogenated agents (16) have demonstrated immunomodulatory properties, but according to a recent meta-analysis, inhalatory anesthesia is associated to reductions in inflammatory mediators (17) and is therefore to be favored. Unfortunately, this difference has not translated into a survival benefit (18) and its meaning remains uncertain.
The intraoperative opioid should also be chosen both on duration of action and possible side effects. The continuous infusion of remifentanil [induction: 0.5–1 µg/kg in at least 90 sec (19); maintenance 0.05–2 µg/kg/min in association with propofol (20) or 2.5–7 ng/mL Cet in TCI] guarantees effective intraoperative analgesia and rapid extubation times. Some clinicians are reluctant to use it for the possible effects of tolerance and hyperalgesia, but these are unlikely when TCI systems are used (21).
Neuromuscular blocking agents (NMBAs)
NMBAs are used during anesthesia to optimize intubating conditions, mechanical ventilation, and the overall quality of the surgical field. The benefits of a deep blockade have not been demonstrated in thoracic surgery, but it is reasonably desirable, in order to enhance patient’s adaptation to the ventilator and avoid cough or hiccups.
Prevention of residual postoperative paralysis is imperative for all types of surgery and even more so in a fast-track setting, as it could delay recovery and increase the rate of complications. Neuromuscular monitoring with methods such as the train-of-four (TOF) is mandatory with this goal in mind. Evidence shows that patients extubated with a TOF ratio below 0.9 have a higher risk of desaturation, airway obstruction (22), muscular weakness (23), and respiratory complications (24), not to mention longer discharge times from the PACU (25). Residual paralysis is less frequent with drugs of intermediate duration of action and when a reversal drug is used (26). A reversal drug needs to be administered when pre-extubation TOF ratio is less than 0.9. Two options are available: acetylcholinesterase inhibitors and sugammadex. The former are less expensive, but have slower onset times, a ceiling effect (27), and they induce a profound vagal stimulation, or tachycardia when administered with atropine. Moreover, an unjustified use of neostigmine, i.e., its administration with no neuromuscular monitoring, has been associated with an increase in mortality for respiratory causes (28). Sugammadex, on the other hand, is safer, more rapid in blockade reversal, and with no ceiling effect, although it is definitely more expensive and can be used only with NMBAs of the aminosteroid family.
One-lung ventilation (OLV)
Management of OLV has to face two main issues. Intraoperative hypoxemia has always been recognized as a possible complication, due to ventilation/perfusion mismatch. Postoperative acute lung injury (ALI), instead, has become evident only more recently and occurs after 4–15% of lung resections. It afflicts both lungs and is probably the result of multiple factors such as mechanical ventilation, surgical manipulation, oxidative stress, and preoperative chemo- and radiotherapy (29). Strategies to prevent ALI definitely need to be part of any ERAS protocol.
A frequent cause of hypoxemia is the dislocation of the device used for lung separation (30); when desaturation appears, therefore, a fiberscopic verification of its correct placement is the first thing that must be done (31). Traditionally, solutions for prevention and treatment of hypoxemia were the use of high fractions of inspired oxygen (FiO2) and large tidal volumes but no positive end-expiratory pressure (PEEP) nor recruitment maneuvers (RM). This approach has proved to be dangerous, with a higher incidence of ALI. Unfortunately, while numerous studies have investigated the best ventilatory strategy during two-lung ventilation (TLV), there is less evidence to guide OLV. The primary goal is the prevention of the so-called volutrauma, atelectrauma, barotrauma, and the resulting biotrauma.
Fraction of inspired oxygen (FiO2)
It is reasonable to adopt the lowest possible FiO2, both before and during OLV to reduce resorption atelectasis in the ventilated lung (32) and during re-expansion to reduce the oxidative stress in the non-ventilated one (33). Animal studies have shown an increase in inflammatory mediators when 100% instead of 50% oxygen was used during OLV (34). A consensus on the lowest safe limit of peripheral oxygen saturation to keep during OLV has not been reached; most clinicians try to maintain it above or equal to 90%. Lower values may be accepted for short periods of time in patients without significant comorbidities; when instead limited organ reserves are present, it is prudent to aim at higher targets (35).
Tidal volume (TV)
Protective ventilatory strategies are associated with reduced pulmonary (14) and systemic inflammation (36), improved gas exchange (37), and fewer postoperative pulmonary complications (38,39). Regardless, the optimal TV to adopt is far from clear: 5–6 mL/kg IBW seems reasonable (32), but some authors suggest 4–5 mL/kg IBW (29), although not yet supported by evidence. We still ignore the specific role of low TV in the setting of protective ventilation, which is rather defined by the modulation and interaction of several parameters. The available studies have compared low TVs and high PEEP with high TVs and no PEEP, not allowing to discriminate the contribution of each component on the final result.
Hypercapnia
The use of low TVs often leads to hypercapnia, which seems to exert protective effects against ventilator-induced lung injury (40,41). In a recent study, a PaCO2 of 60–70 mmHg reached during OLV was not only well-tolerated, but linked to reduced post-thoracotomic lung and systemic inflammation (42). It appears reasonable to allow a certain degree of hypercapnia during OLV, except in patients with pulmonary or intracranial hypertension or major arrhythmias.
PEEP
Functional residual capacity ceases to exist with the surgical pneumothorax. The ventilated lung collapses toward the residual volume and its end-expiratory volume becomes dependent on the ventilatory parameters (29). CT scans have demonstrated 80% of atelectasis at end-expiration despite the application of 5 cmH2O of PEEP (43). OLV seems to occur below the closing capacity of the ventilated lung. Strategies to maintain a certain end-expiratory volume are to be preferred. PEEP titration based on dynamic compliance of the respiratory system (with an average result of 10±2 cmH2O) was shown to improve intraoperative oxygenation when compared with a fixed value of 5 cmH2O (44). Experimentally, the highest compliance is reached with a compromise between hyperinflation and recruitment (45,46); this could explain the aforementioned results. The individual contribution of PEEP to ventilator-induced lung injury has not been explored; yet in the absence of adequate PEEP, a low TV has recently been linked to increased postoperative respiratory complications (47), indirectly underlying its importance.
Recruitment maneuvers (RM)
The combined application of a RM during TLV and protective ventilation is associated with reduced cyclic alveolar recruitment-derecruitment and release of inflammatory cytokines (43). Cycling techniques seem to cause less lung stress than sustained pressure holds and vital capacity sighs (48). Better oxygenation, higher compliance, and decreased dead space have been obtained with cycling RM in OLV as well (49). Reasonably, the pressure necessary to recruit a healthy lung should not exceed 40 cmH2O, with a PEEP slowly increasing up to 20 cmH2O. The optimal number of RM to be performed during anesthesia is not clear. In most cases, a single initial RM is sufficient, provided that adequate PEEP is applied. Whether additional RM are to be employed routinely or just in case of desaturation is yet to be determined. A final RM after the re-expansion of the non-ventilated lung is recommended (50), and it should be performed at lower pressure levels in order to prevent damage to surgical staples (49,51).
Modes of ventilation
Studies comparing volume-controlled (VCV) with pressure-controlled ventilation (PCV) during OLV have led to equivocal results in terms of oxygenation (52,53). Some authors support the use of PCV when high airway pressures are reached (51). On the other hand, only VCV guarantees the delivery of the set TV. Furthermore, elevated peak airway pressures should not be a cause of concern, given the high tube-related resistance during OLV and the similarity of intrabronchial pressures observed with the two modalities (54). Plateau pressures should instead carefully be monitored.
Continuous positive airway pressure (CPAP)
The application of CPAP to the non-ventilated lung has proved useful as a rescue strategy after optimization of ventilatory parameters, to improve oxygenation and allow lower FiO2 (55). Significant results have been reached with levels of CPAP as low as 2 cmH2O (56). Such minimal values can be used even during VATS without affecting the view of the surgical field. Higher pressures would instead cause an insufficient collapse of the non-ventilated lung (57). In addition, a lower inflammatory response has been observed with CPAP (58), probably because of reduced atelectasis and diminished damage during re-expansion.
Locoregional anesthesia
Locoregional anesthesia has a fundamental role in maximizing all potential advantages of mini-invasive techniques like VATS. Thoracic epidural anesthesia (TEA) still represents the standard of reference for the thoracotomic approach (11), but other locoregional techniques have gained popularity in recent times. Due to lack of adequate evidence, a similar consensus on the best approach has not been reached for VATS, although the most recent literature advocates for the thoracic paravertebral block (PVB) (59).
Thoracic epidural anesthesia (TEA)
Epidural block with local anesthetics historically proved a reduced sympathetic response to the surgical stimulus, an improved coagulative profile and a positive influence on endocrine and immune functions (60). It is particularly beneficial in patients with preoperative cardiovascular and respiratory disease (61). Per contra, it features numerous potential complications, both local (epidural hematoma, dural puncture, catheter malposition or rupture, patchy anesthesia, abscess, radiculitis, chronic radicular pain, medullar ischemia, spinal trauma) and systemic (hypotension, respiratory depression, shivering, headache, nausea, urinary retention, intravenous spread of local anesthetic); some represent absolute contraindications limiting its use in specific categories of patients (e.g., coagulopathy).
Epidural anesthesia can be obtained with various local anesthetics, alone or associated with opioids (62). Bupivacaine and fentanyl are the most cited in the context of thoracic surgery (63). but the available studies all deal with thoracotomies and are not fast-track oriented. In this setting the association with a low-dose opioid is not recommended because of the higher incidence of adverse reactions. Bupivacaine is commonly used at the 0.25% concentration, with a bolus of 8–15 mL followed by 0.1 mL/kg/h infusion (64,65), yet the 0.125% concentration is also reported, with a 10 mL bolus and infusion at 8 mL/h (66). Levobupivacaine is comparable in terms of sensitive block, hemodynamic response and analgesia, while the safety profile is different (67). These dosages have been investigated for open, thoracotomic procedures. Mini-invasive approaches like VATS are de facto less traumatic thanks to smaller surgical incision and reduced intercostal nerve injury due to stretch by the rib spreader or entrapment during closure of the surgical field, and as such they entail a lower incidence of acute postoperative pain (68,69). Lower concentrations of local anesthetic can therefore be considered, although not yet supported by clinical studies (e.g., bupivacaine 0.125% 0.1 mL/kg bolus and 0.1% 7 mL/h infusion). The same can be said about ropivacaine: in previous reports it was used as 0.75% 5 mL bolus and 0.25% 5 mL infusion (70), more recently it has been effectively employed as 0.2% 5 mL bolus and 5 mL/h infusion at the same concentration (71). With the above considerations, we recommend the latter posology.
Paravertebral block (PVB)
It consists in the infiltration of the local anesthetic in the cuneiform area localized laterally all along the vertebral column, affecting the spinal nerves immediately after their egress from the intervertebral foramina (72). It is often thought of as an “unilateral epidural”, owing to its selectivity, even though some degree of epidural diffusion is possible. Somatic and sympathetic nerves are also involved, but the hemodynamic response is less prominent (60). When compared to TEA, the PVB guarantees a similar level of analgesia, fewer complications, a safer profile and better outcomes (60,61,73,74).
PVBs can be performed preoperatively, blindly (with the loss of resistance technique) or with ultrasound guidance (73,75), or intraoperatively by the surgeon under direct view (76). Both single-shot infiltrations with a long-acting local anesthetic and catheter placements for subpleural continuous infusion are possible (72). Bupivacaine, levobupivacaine, and ropivacaine can all be employed with no evidence of superiority of one over the others (60,61). Bupivacaine and levobupivacaine are typically used at 0.25–0.5%, ropivacaine at 0.75%. The injected volumes are 5 mL for each paravertebral space, being careful not to exceed the systemic toxic dosage. Continuous infusion is used at the same concentrations (except for ropivacaine, where 0.2% is preferred), with a velocity tailored for each case (around 0.1 mL/kg/h, for a total of 2.5–10 mL/h) (74).
Intercostal nerve block (ICNB)
A thorough knowledge of anatomy is required for this type of block. As for PVB, it can be realized percutaneously (blindly or echo-guided), or “from the inside” by the surgeon, and it contemplates the insertion of a subpleural catheter for continuous infusion. The local anesthetic is normally injected at many levels due to the numerous anastomoses running between adjacent intercostal nerves. To avoid exceeding the safe plasmatic levels of the local anesthetic, the maximum dose is first calculated then adequately diluted to obtain the volumes necessary for the block. Low-dose epinephrine can be added to inhibit systemic absorption and prolong the anesthetic effect. No evidence exists about the local anesthetic of choice for the ICNB; in the available studies bupivacaine 0.5% has been used, with volumes of 1.5–3 mL depending on the number of spaces to be covered (77,78). When compared to TEA and PVB, this block seems to offer a poorer pain control, yet it can still be favored for the lower incidence of adverse events (77).
Serratus anterior plane block (SAPB)
With the recent development and spreading of US-guided peripheral blocks, other techniques involving infiltration of fascial planes infiltration are gaining popularity and are under scrutiny. The SAPB has been recently described by Blanco and colleagues (79). The resulting dermatomal sensory loss extends from T2 to T7 and lasts about 12 hours with the superficial injection and slightly less for deeper infiltration. The effective spreading to the lateral cutaneous branches of the intercostal nerves has been demonstrated using a dye solution (80). Initially suggested for breast surgery, the SAPB associated with catheter positioning for continuous infusion has been successfully used as an alternative to epidural analgesia for multiple rib fracture (81), and as a rescue strategy in case of epidural failure following esophagectomy (82). Its use as technique of choice for analgesia after thoracotomy (Levobupivacaine 0.25% 20 mL bolus, followed by 0.125% 5 mL/h infusion) seems to offer more hemodynamic stability and overall comparable efficacy when compared to TEA (83). For VATS, the single shot may be suitable (84), but further studies are required to draw definitive conclusions.
Intravenous lidocaine
Intraoperative intravenous administration of lidocaine has been qualifying as a powerful adjuvant for the control of postoperative pain, with favorable results on patients evaluation, opioid consumption, recovery of bowel function, duration of hospitalization, and rehabilitation times, with no evidence of toxicity (85,86).
Lidocaine is a local anesthetic of the amide family, whose principal mechanism of action involves the blockade of voltage-gated sodium channels (19). Other pharmacodynamic properties play a role in its analgesic profile: it presents inhibitory effects on G protein-coupled (87) and NMDA receptors (88), on neutrophil priming (89), and on TNFα signaling in endothelial cells (90). Intravenous infusion of lidocaine has been proposed for chronic pain, especially of the neuropathic type (91), and lately in the perioperative setting, where its adoption appears effective, safe, simple, economical, and widely accessible. Successful results have been reported in abdominal (86), spinal (92), and thoracic surgery (93). In regard to VATS, the only available investigation could not prove an advantage, yet the results may have been jeopardized by an overall low morphine consumption, a short infusion period, and a limited sample size (94). In any case, no adverse events have been reported in any of the mentioned studies, and measured blood concentrations after 1.5 mg/kg bolus followed by 2 mg/kg/h infusion are consistently below toxic levels (85). It appears reasonable to recommend such posology and to limit the postoperative infusion to the period of time in which the patients remain monitored and in a context (e.g., PACU, or intensive care unit) where adverse events would be promptly recognized and treated.
Fluid therapy
A careful management of intraoperative fluid therapy is paramount to optimize postoperative outcome, and even more so in the context of fast-track surgery. Yet it remains nowadays one of the most debated and controversial issues of patient care. To complicate the matter, scientific evidences on the subject concentrate on other surgical specialties, while those related to thoracic surgery are limited.
Intravascular volume directly affects cardiac output and consequently oxygen delivery. On one hand, excessive fluid administration may lead to overload in the interstitial space, with increased pulmonary complications, delayed recovery (95), and an overall negative impact (96). On the other, hypovolemia can compromise the integrity of surgical anastomoses and the perfusion of vital organs like the kidneys (97). The incidence of acute kidney injury (AKI) after thoracic surgery is 5.9–6.8% (98,99) but can be reduced by hemodynamic optimization with adequate fluid therapy and possibly vasopressor use (100). Urine output should not be used to guide fluid therapy. Intraoperative oliguria is not related to postoperative AKI (101).
The goal of perioperative fluid management should be a fluid balance approximate to zero (102). Perioperative requirements can be satisfied with 1–2 mL/kg/h of crystalloid infusion (103,104). Balanced electrolyte solutions have been proved to be superior to saline for electrolyte homeostasis (105). The hyperchloremic acidosis caused by saline solutions has been linked to a higher risk of renal injury, longer hospital stays and increased 30-day mortality (106). More recent studies have challenged these results, showing that balanced solutions do not guarantee a lower incidence of renal injury (107). Colloids are solutions with a distribution volume mostly limited to the intravascular compartment, with high molecular weight molecules in suspension. They increase the oncotic pressure of plasma and reduce the transcapillary passage of water. Their administration causes greater volemic expansion than crystalloids that instead diffuse freely in the interstitial space. Colloids are associated with a lower incidence of PONV (108). Based on the current data, there is no clear evidence that perioperative colloids promote the development of renal failure (109) and have to be considered equivalent to crystalloids for the intraoperative replenishment of intravascular volume.
Perioperative fluid therapy should be guided by objective measurements of hypovolemia. The so-called goal-directed fluid therapy (110) consists in a rational approach of intravenous fluid administration based on hemodynamic parameters able to predict a positive response (in terms of cardiac output) after volume expansion, avoiding unnecessary loads. Transesophageal Doppler and systems such as VigileoTM and PiCCOTM have been evaluated during thoracic surgery (111,112). Dynamic indices like stroke volume variation and pulse pressure variation, derived from the pulse contour analysis of mechanically ventilated patients (113), have been investigated as possible predictors of fluid-responsiveness during OLV. Affirmative results have been observed when TV was set at 8 mL/kg or more (114), which is no longer acceptable in the era of protective ventilation; their predictive value was instead lost when TV was lowered to 6 mL/kg (111). In conclusion, with the open thorax and during protective OLV, invasive arterial pressure monitoring is still recommended, but the reliability of more advanced parameters is poor (115). Thus, it seems reasonable to evaluate the patient’s hemodynamics by analyzing the adequacy of oxygen delivery, using indirect variables like blood lactates and central venous oxygen saturation, and to consider vasopressors for the correction of hypotension (116) when it is likely the result of relative drug-induced hypovolemia rather than a real volume deficit. Inotropes should be reserved to patients with an objective assessment of cardiac dysfunction, e.g., as demonstrated by transesophageal echocardiography (117).
In summary, the most relevant evidence-based points (118,119) regarding a correct fluid management are:
- Maintain total intravenous fluids during the first 24 hours under 20 mL/kg;
- Avoid aggressive fluid administration (under 2 mL/kg/h intraoperatively and 1.5 mL/kg/h in the first 12 hours) and discontinue infusion after resumption of adequate oral intake;
- Consider colloids only in case of intraoperative hemorrhage not requiring immediate transfusion of blood products; in any case, a maximum dose of 1 L;
- Urine output greater than 0.5 mL/kg/h is not required in the immediate postoperative period, except for patients with preexisting risk factors for development of AKI.
New insights: non-intubated VATS (NI-VATS)
OLV has classically been considered necessary for most thoracic surgical procedures. Recently, advances in VATS have allowed experimentation in non-intubated patients, first for minor interventions (120), then even for major procedures like pneumonectomy (121). With this approach, a recent meta-analysis reported a lower risk of postoperative complications and a shorter mean hospital stay, both in randomized controlled trials and in observational studies (122). At the moment, only one study evaluated the patients’ follow-up, with no evidence of a higher rate of tumor recurrence (123). Overall numbers are scant: in Europe the technique is limited to small operations: 98% of surgeons tried it during surgical evacuation of pleural effusion, while just 26% during decortications for empyema or pulmonary biopsies, and only 2% for lobectomies (124).
NI-VATS, performed with the patient in spontaneous ventilation, requires an increased anesthesiological effort, the understanding of some peculiar pathophysiological aspects, accurate patient selection, mastery of locoregional techniques, judicious sedation, and rigorous planning of airway management in the event that a switch to general anesthesia and lung separation becomes necessary. Among the advantages of keeping the patient in spontaneous ventilation is the preservation of diaphragmatic activity (125). Lung separation is obtained with the induction of a surgical pneumothorax, although emphysema and pleural adhesions can slow down the resulting lung collapse (126). Lastly, a diminished recourse to anesthetic drugs may help the preservation of hypoxic pulmonary vasoconstriction (126). On the downside, paradoxical breathing (so called pendelluft effect) can develop between the two lungs (125), increasing the risk of hypoxemia and hypercapnia, sometimes so evident to require a switch to general anesthesia, in 1% of patients (127). In most cases, hypercapnia resolves spontaneously, and postoperative PaCO2 is actually lower than after conventional anesthesia (128). Moreover, permissive hypercapnia can have positive results on the general outcome (129). Hypotension, due to the mediastinal shift that occurs during pneumothorax, is a potential issue, but it does not appear to be more relevant than under general anesthesia (130).
Predicted surgical difficulties can be prevailing in patient selection: expected pleural adhesions, extensive resections or interstitial disease advise against the use of NI-VATS (129) while patients of small build and requiring a simple anatomic access are to be favored, at least initially (131). From an anesthesiologist’s perspective, ASA class greater than 3 and contraindications to locoregional techniques represent other exclusion criteria (132). Most trials only include patients with optimal pulmonary function tests, yet minor procedures have been brought to completion even in patients with severe respiratory dysfunction (133).
A thorough examination of the technique is beyond the scope of this review. In general, NI-VATS appears a feasible option but it requires a considerable amount of expertise both by surgeon and anesthesiologist, not to mention the whole operating room staff. The observed advantages need to be interpreted in the light of the limited numbers (although in rapid expansion) and of its practicability in one’s own clinical context.
Conclusions
Anesthesia in the fast-track era is a rapidly evolving subject that requires exceptional attention and continuous update, especially in a delicate setting such as thoracic surgery. Translating scientific evidence into daily practice can be particularly wearying. Moreover, many questions remain open. Fundamental aspects of intraoperative management such as OLV, locoregional anesthesia or fluid therapy are still controversial, although considerable insight has been gained in just a few years and today some light can be shed (Table 1). Further research is definitely warranted. Yet many positive results have been accomplished with undeniable satisfaction. We hope this review will be of help to fellow clinicians working every day to enhance their patients’ recovery after thoracic surgery.
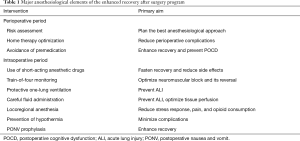
Full table
Acknowledgements
We thank Trieste’s ACTO study group who provided help and insight during the writing of the manuscript. We also thank Dr. Alberto Peratoner for the general supervision and Dr. Diego Morri for the linguistic assistance. Lastly, Dr. Andrea Droghetti for the invitation to collaborate and the administrative support.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Desai H, Natt B, Kim S, et al. Decreased in-hospital mortality after lobectomy using video-assisted thoracoscopic surgery compared with open thoracotomy. Ann Am Thorac Soc 2017;14:262-6. [PubMed]
- Della Rocca G, Vetrugno L, Coccia C, et al. Preoperative evaluation of patients undergoing lung resection surgery: defining the role of the anesthesiologist on a multidisciplinary team. J Cardiothorac Vasc Anesth 2016;30:530-8. [Crossref] [PubMed]
- Thompson T, Trevor T, Edmund K, et al. Anxiety sensitivity and pain: Generalisability across noxious stimuli. Pain 2008;134:187-96. [Crossref] [PubMed]
- Walker KJ, Smith AF. Premedication for anxiety in adult day surgery. Cochrane Database Syst Rev 2009.CD002192. [PubMed]
- Ip HYV, Amir A, Peng PWH, et al. Predictors of postoperative pain and analgesic consumption. Anesthesiology 2009;111:657-77. [Crossref] [PubMed]
- Vermeeren A. Residual effects of hypnotics: epidemiology and clinical implications. CNS Drugs 2004;18:297-328. [Crossref] [PubMed]
- Fredman B, Lahav M, Zohar E, et al. The effect of midazolam premedication on mental and psychomotor recovery in geriatric patients undergoing brief surgical procedures. Anesth Analg 1999;89:1161-6. [Crossref] [PubMed]
- Richardson MG, Wu CL, Hussain A. Midazolam premedication increases sedation but does not prolong discharge times after brief outpatient general anesthesia for laparoscopic tubal sterilization. Anesth Analg 1997;85:301-5. [PubMed]
- Lepousé C, Lautner CA, Liu L, et al. Emergence delirium in adults in the post-anaesthesia care unit. Br J Anaesth 2006;96:747-53. [Crossref] [PubMed]
- Weingarten TN, Bergan TS, Narr BJ, et al. Effects of changes in intraoperative management on recovery from anesthesia: a review of practice improvement initiative. BMC Anesthesiol. 2015;15:54. [Crossref] [PubMed]
- Loop T. Fast track in thoracic surgery and anaesthesia: update of concepts. Curr Opin Anaesthesiol 2016;29:20-5. [Crossref] [PubMed]
- Smith I, White PF, Nathanson M, et al. Propofol. An update on its clinical use. Anesthesiology 1994;81:1005-43. [Crossref] [PubMed]
- Lee WK, Kim MS, Kang SW, et al. Type of anaesthesia and patient quality of recovery: a randomized trial comparing propofol-remifentanil total i.v. anaesthesia with desflurane anaesthesia. Br J Anaesth 2015;114:663-8. [Crossref] [PubMed]
- Schilling T, Kozian A, Huth C, et al. The pulmonary immune effects of mechanical ventilation in patients undergoing thoracic surgery. Anesth Analg 2005;101:957-65. [Crossref] [PubMed]
- Takao Y, Mikawa K, Nishina K, et al. Attenuation of acute lung injury with propofol in endotoxemia. Anesth Analg 2005;100:810-6. [Crossref] [PubMed]
- De Conno E, Steurer MP, Wittlinger M, et al. Anesthetic-induced improvement of the inflammatory response to one-lung ventilation. Anesthesiology 2009;110:1316-26. [Crossref] [PubMed]
- Sun B, Wang J, Bo L, et al. Effects of volatile vs. propofol-based intravenous anesthetics on the alveolar inflammatory responses to one-lung ventilation: a meta-analysis of randomized controlled trials. J Anesth 2015;29:570-9. [Crossref] [PubMed]
- Módolo NSP, Módolo MP, Marton MA, et al. Intravenous versus inhalation anaesthesia for one-lung ventilation. Cochrane Database Syst Rev 2013.CD006313. [PubMed]
- Flood P, Rathmell JP, Shafer S. Stoelting’s pharmacology and physiology in anesthetic practice. Lippincott Williams & Wilkins, 2015: 960.
- Hogue CW Jr, Bowdle TA, O’Leary C, et al. A multicenter evaluation of total intravenous anesthesia with remifentanil and propofol for elective inpatient surgery. Anesth Analg 1996;83:279-85. [Crossref] [PubMed]
- Yu EHY, Tran DHD, Lam SW, et al. Remifentanil tolerance and hyperalgesia: short-term gain, long-term pain? Anaesthesia 2016;71:1347-62. [Crossref] [PubMed]
- Murphy GS, Szokol JW, Marymont JH, et al. Intraoperative acceleromyographic monitoring reduces the risk of residual neuromuscular blockade and adverse respiratory events in the postanesthesia care unit. Anesthesiology 2008;109:389-98. [Crossref] [PubMed]
- Murphy GS, Szokol JW, Avram MJ, et al. Intraoperative acceleromyography monitoring reduces symptoms of muscle weakness and improves quality of recovery in the early postoperative period. Anesthesiology 2011;115:946-54. [Crossref] [PubMed]
- Berg H, Roed J, Viby-Mogensen J, et al. Residual neuromuscular block is a risk factor for postoperative pulmonary complications A prospective, randomised, and blinded study of postoperative pulmonary complications after atracurium, vecuronium and pancuronium. Acta Anaesthesiol Scand 1997;41:1095-103. [Crossref] [PubMed]
- Butterly A, Bittner EA, George E, et al. Postoperative residual curarization from intermediate-acting neuromuscular blocking agents delays recovery room discharge. Br J Anaesth. 2010;105:304-9. [Crossref] [PubMed]
- Naguib M, Kopman AF, Ensor JE. Neuromuscular monitoring and postoperative residual curarisation: a meta-analysis. Br J Anaesth 2007;98:302-16. [Crossref] [PubMed]
- McCourt KC, Mirakhur RK, Kerr CM. Dosage of neostigmine for reversal of rocuronium block from two levels of spontaneous recovery. Anaesthesia 1999;54:651-5. [Crossref] [PubMed]
- Sasaki N, Meyer MJ, Malviya SA, et al. Effects of neostigmine reversal of nondepolarizing neuromuscular blocking agents on postoperative respiratory outcomes: a prospective study. Anesthesiology 2014;121:959-68. [Crossref] [PubMed]
- Lohser J, Slinger P. Lung injury after one-lung ventilation: a review of the pathophysiologic mechanisms affecting the ventilated and the collapsed lung. Anesth Analg 2015;121:302-18. [Crossref] [PubMed]
- Campos JH, Hallam EA, Van Natta T, et al. Devices for Lung Isolation Used by Anesthesiologists with Limited Thoracic Experience. Anesthesiology 2006;104:261-6. [Crossref] [PubMed]
- Varma S, Sandeep V, Zoe B, et al. Intraoperative bronchoscopy prevents hypoxaemia during one-lung ventilation for second-stage oesophagectomy: a prospective cohort study. Eur J Anaesthesiol 2010;27:919-21. [Crossref] [PubMed]
- Şentürk M, Slinger P, Cohen E. Intraoperative mechanical ventilation strategies for one-lung ventilation. Best Pract Res Clin Anaesthesiol 2015;29:357-69. [Crossref] [PubMed]
- Misthos P, Katsaragakis S, Theodorou D, et al. The degree of oxidative stress is associated with major adverse effects after lung resection: a prospective study. Eur J Cardiothorac Surg 2006;29:591-5. [Crossref] [PubMed]
- Olivant Fisher A, Fisher AO, Husain K, et al. Hyperoxia during one lung ventilation: Inflammatory and oxidative responses. Pediatr Pulmonol 2012;47:979-86. [Crossref] [PubMed]
- Slinger PD, Campos JH. Anesthesia for thoracic surgery. In: Miller RD, Eriksson LI, Fleisher LA, Wiener-Kronish JP, Young WL, editors. Miller’s anesthesia. 7th ed. Amsterdam: Elsevier;2009:1856.
- Michelet P, D’Journo X-B, Roch A, et al. Protective ventilation influences systemic inflammation after esophagectomy: a randomized controlled study. Anesthesiology 2006;105:911-9. [Crossref] [PubMed]
- Yang M, Mikyung Y, Ahn HJ, et al. Does a protective ventilation strategy reduce the risk of pulmonary complications after lung cancer surgery? Chest 2011;139:530-7. [Crossref] [PubMed]
- Licker M, Diaper J, Villiger Y, et al. Impact of intraoperative lung-protective interventions in patients undergoing lung cancer surgery. Crit Care 2009;13:R41. [Crossref] [PubMed]
- Fernández-Pérez ER, Keegan MT, Brown DR, et al. Intraoperative tidal volume as a risk factor for respiratory failure after pneumonectomy. Anesthesiology. 2006;105:14-8. [Crossref] [PubMed]
- Kregenow DA, Rubenfeld GD, Hudson LD, et al. Hypercapnic acidosis and mortality in acute lung injury. Crit Care Med 2006;34:1-7. [Crossref] [PubMed]
- Costello J, Higgins B, Contreras M, et al. Hypercapnic acidosis attenuates shock and lung injury in early and prolonged systemic sepsis. Crit Care Med 2009;37:2412-20. [Crossref] [PubMed]
- Gao W, Liu D, Li D, et al. Effects of hypercapnia on T cells in lung ischemia/reperfusion injury after lung transplantation. Exp Biol Med (Maywood) 2014;239:1597-605. [Crossref] [PubMed]
- Kozian A, Schilling T, Schütze H, et al. Ventilatory protective strategies during thoracic surgery: effects of alveolar recruitment maneuver and low-tidal volume ventilation on lung density distribution. Anesthesiology 2011;114:1025-35. [Crossref] [PubMed]
- Ferrando C, Carlos F, Ana M, et al. Setting individualized positive end-expiratory pressure level with a positive end-expiratory pressure decrement trial after a recruitment maneuver improves oxygenation and lung mechanics during one-lung ventilation. Anesthesia & Analgesia 2014;118:657-65. [Crossref] [PubMed]
- Carvalho AR, Spieth PM, Paolo P, et al. Ability of dynamic airway pressure curve profile and elastance for positive end-expiratory pressure titration. Intensive Care Med 2008;34:2291-9. [Crossref] [PubMed]
- Carvalho AR, Jandre FC, Pino AV, et al. Effects of descending positive end-expiratory pressure on lung mechanics and aeration in healthy anaesthetized piglets. Crit Care 2006;10:R122. [Crossref] [PubMed]
- Blank RS, Colquhoun DA, Durieux ME, et al. Management of one-lung ventilation. Anesthesiology 2016;124:1286-95. [Crossref] [PubMed]
- Silva PL, Moraes L, Santos RS, et al. Recruitment maneuvers modulate epithelial and endothelial cell response according to acute lung injury etiology. Crit Care Med 2013;41:e256-65. [Crossref] [PubMed]
- Tusman G, Böhm SH, Sipmann FS, et al. Lung recruitment improves the efficiency of ventilation and gas exchange during one-lung ventilation anesthesia. Anesth Analg 2004;98:1604-9. [Crossref] [PubMed]
- Tusman G, Bohm SH, Suarez-Sipmann F. Alveolar recruitment maneuvers for one-lung ventilation during thoracic anesthesia. Curr Anesthesiol Rep 2014;4:160-9. [Crossref]
- Della Rocca G, Coccia C. Acute lung injury in thoracic surgery. Curr Opin Anaesthesiol. 2013;26:40-6. [Crossref] [PubMed]
- Tuğrul M, Camci E, Karadeniz H, et al. Comparison of volume controlled with pressure controlled ventilation during one-lung anaesthesia. Br J Anaesth 1997;79:306-10. [Crossref] [PubMed]
- Unzueta MC, Casas JI, Moral MV. Pressure-controlled versus volume-controlled ventilation during one-lung ventilation for thoracic surgery. Anesth Analg 2007;104:1029-33. [Crossref] [PubMed]
- Rozé H, Lafargue M, Batoz H, et al. Pressure-controlled ventilation and intrabronchial pressure during one-lung ventilation. Br J Anaesth 2010;105:377-81. [PubMed]
- Capan LM, Herman T, Chandrakant P, Sivam R, et al. Optimization of arterial oxygenation during one-lung anesthesia. Anesthesia & Analgesia 1980;59:847-51. [Crossref] [PubMed]
- El-Tahan MR, El Ghoneimy YF, Regal MA, et al. Comparative study of the non-dependent continuous positive pressure ventilation and high-frequency positive-pressure ventilation during one-lung ventilation for video-assisted thoracoscopic surgery. Interact Cardiovasc Thorac Surg 2011;12:899-902. [Crossref] [PubMed]
- Bailey J, John B, Maged M, et al. Problems with CPAP during one-lung ventilation in thoracoscopic surgery. J Cardiothorac Vasc Anesth 1998;12:239. [Crossref] [PubMed]
- Verhage RJJ, Boone J, Rijkers GT, et al. Reduced local immune response with continuous positive airway pressure during one-lung ventilation for oesophagectomy. Br J Anaesth. 2014;112:920-8. [Crossref] [PubMed]
- Steinthorsdottir KJ, Wildgaard L, Hansen HJ, et al. Regional analgesia for video-assisted thoracic surgery: a systematic review. Eur J Cardiothorac Surg 2014;45:959-66. [Crossref] [PubMed]
- Baidya DK, Khanna P, Maitra S. Analgesic efficacy and safety of thoracic paravertebral and epidural analgesia for thoracic surgery: a systematic review and meta-analysis. Interact Cardiovasc Thorac Surg 2014;18:626-35. [Crossref] [PubMed]
- Davies RG. A comparison of the analgesic efficacy and side-effects of paravertebral vs epidural blockade for thoracotomy--a systematic review and meta-analysis of randomized trials. Br J Anaesth 2006;96:418-26. [Crossref] [PubMed]
- Manion SC, Brennan TJ. Thoracic epidural analgesia and acute pain management. Anesthesiology 2011;115:181-8. [Crossref] [PubMed]
- Powell ES, Cook D, Pearce AC, et al. A prospective, multicentre, observational cohort study of analgesia and outcome after pneumonectomy. Br J Anaesth 2011;106:364-70. [Crossref] [PubMed]
- Perttunen K, Nilsson E, Heinonen J, et al. Extradural, paravertebral and intercostal nerve blocks for post-thoracotomy pain. Br J Anaesth 1995;75:541-7. [Crossref] [PubMed]
- Richardson J, Sabanathan S, Jones J, et al. A prospective, randomized comparison of preoperative and continuous balanced epidural or paravertebral bupivacaine on post-thoracotomy pain, pulmonary function and stress responses. Br J Anaesth 1999;83:387-92. [Crossref] [PubMed]
- Kanazi GE, Ayoub CM, Aouad M, et al. Subpleural block is less effective than thoracic epidural analgesia for post-thoracotomy pain: a randomised controlled study. Eur J Anaesthesiol 2012;29:186-91. [Crossref] [PubMed]
- Cok YO, Eker HE, Turkoz A, et al. Effects of thoracic epidural anaesthesia on intraoperative haemodynamics and postoperative analgesia for thoracic surgery: levobupivacaine versus bupivacaine. Reg Anesth Pain Med 2008;33:e39.
- Maxwell C, Cory M, Alina N. New developments in the treatment of acute pain after thoracic surgery. Curr Opin Anaesthesiol 2014;27:6-11. [Crossref] [PubMed]
- García-Tirado J, Javier GT, Cristina RR. Suture techniques of the intercostal space in thoracotomy and their relationship with post-thoracotomy pain: a systematic review. Arch Bronconeumol 2012;48:22-8. [Crossref] [PubMed]
- Casati A, Alessandrini P, Nuzzi M, et al. A prospective, randomized, blinded comparison between continuous thoracic paravertebral and epidural infusion of 0.2% ropivacaine after lung resection surgery. Eur J Anaesthesiol 2006;23:999-1004. [Crossref] [PubMed]
- Kobayashi R, Mori S, Wakai K, et al. Paravertebral block via the surgical field versus epidural block for patients undergoing thoracotomy: a randomized clinical trial. Surg Today 2013;43:963-9. [Crossref] [PubMed]
- Piraccini E, Pretto EA Jr, Corso RM, et al. Analgesia for thoracic surgery: the role of paravertebral block. HSR Proc Intensive Care Cardiovasc Anesth 2011;3:157-60. [PubMed]
- Amlong C, Guy M, Schroeder KM, et al. Out-of-plane ultrasound-guided paravertebral blocks improve analgesic outcomes in patients undergoing video-assisted thoracoscopic surgery. Local Reg Anesth 2015;8:123-8. [PubMed]
- Ding X, Jin S, Niu X, et al. A comparison of the analgesia efficacy and side effects of paravertebral compared with epidural blockade for thoracotomy: an updated meta-analysis. PLoS One 2014;9:e96233. [Crossref] [PubMed]
- Marhofer P, Kettner SC, Hajbok L, et al. Lateral ultrasound-guided paravertebral blockade: an anatomical-based description of a new technique. Br J Anaesth 2010;105:526-32. [Crossref] [PubMed]
- Helms O, Mariano J, Hentz JG, et al. Intra-operative paravertebral block for postoperative analgesia in thoracotomy patients: a randomized, double-blind, placebo-controlled study. Eur J Cardiothorac Surg 2011;40:902-6. [PubMed]
- Wurnig PN, Lackner H, Teiner C, et al. Is intercostal block for pain management in thoracic surgery more successful than epidural anaesthesia? Eur J Cardiothorac Surg 2002;21:1115-9. [Crossref] [PubMed]
- Bolotin G, Lazarovici H, Uretzky G, et al. The efficacy of intraoperative internal intercostal nerve block during video-assisted thoracic surgery on postoperative pain. Ann Thorac Surg 2000;70:1872-5. [Crossref] [PubMed]
- Blanco R, Parras T, McDonnell JG, et al. Serratus plane block: a novel ultrasound-guided thoracic wall nerve block. Anaesthesia 2013;68:1107-13. [Crossref] [PubMed]
- Mayes J, Davison E, Panahi P, et al. An anatomical evaluation of the serratus anterior plane block. Anaesthesia 2016;71:1064-9. [Crossref] [PubMed]
- Kunhabdulla NP, Agarwal A, Gaur A, et al. Serratus anterior plane block for multiple rib fractures. Pain Physician 2014;17:E553-5. [PubMed]
- Madabushi R, Tewari S, Gautam SK, et al. Serratus anterior plane block: a new analgesic technique for post-thoracotomy pain. Pain Physician 2015;18:E421-4. [PubMed]
- Khalil AE, Abdallah NM, Bashandy GM, et al. Ultrasound-guided serratus anterior plane block versus thoracic epidural analgesia for thoracotomy pain. J Cardiothorac Vasc Anesth 2017;31:152-8. [Crossref] [PubMed]
- Ökmen K, Ökmen BM. The efficacy of serratus anterior plane block in analgesia for thoracotomy: a retrospective study. J Anesth 2017;31:579-85. [Crossref] [PubMed]
- Kaba A, Laurent SR, Detroz BJ, et al. Intravenous lidocaine infusion facilitates acute rehabilitation after laparoscopic colectomy. Anesthesiology 2007;106:11-8. [Crossref] [PubMed]
- Marret E, Rolin M, Beaussier M, et al. Meta-analysis of intravenous lidocaine and postoperative recovery after abdominal surgery. Br J Surg 2008;95:1331-8. [Crossref] [PubMed]
- Hollmann MW, Strumper D, Herroeder S, et al. Receptors, g proteins, and their interactions. Anesthesiology 2005;103:1066-78. [Crossref] [PubMed]
- Sugimoto M, Masahiro S, Ichiro U, et al. Local anaesthetics have different mechanisms and sites of action at the recombinant N-methyl-D-aspartate (NMDA) receptors. Br J Pharmacol 2003;138:876-82. [Crossref] [PubMed]
- Hollmann MW, Gross A, Jelacin N, et al. Local anesthetic effects on priming and activation of human neutrophils. Anesthesiology 2001;95:113-22. [Crossref] [PubMed]
- Piegeler T, Votta-Velis EG, Bakhshi FR, et al. Endothelial barrier protection by local anesthetics: ropivacaine and lidocaine block tumor necrosis factor-α-induced endothelial cell Src activation. Anesthesiology 2014;120:1414-28. [Crossref] [PubMed]
- Tremont-Lukats IW, Hutson PR, Backonja MM. A randomized, double-masked, placebo-controlled pilot trial of extended IV lidocaine infusion for relief of ongoing neuropathic pain. Clin J Pain 2006;22:266-71. [Crossref] [PubMed]
- Farag E, Ghobrial M, Sessler DI, et al. Effect of perioperative intravenous lidocaine administration on pain, opioid consumption, and quality of life after complex spine surgery. Anesthesiology 2013;119:932-40. [Crossref] [PubMed]
- Cui W, Weihua C, Yanping L, et al. Systemic administration of lidocaine reduces morphine requirements and postoperative pain of patients undergoing thoracic surgery after propofol–remifentanil-based anaesthesia. Eur J Anaesthesiol 2010;27:41-6. [Crossref] [PubMed]
- Slovack M, Taylor B, Bryce R, et al. Does intravenous lidocaine infusion during video-assisted thoracoscopic surgery reduce postoperative analgesia? A randomized controlled study. Can J Anaesth 2015;62:676-7. [Crossref] [PubMed]
- Gustafsson UO, Hausel J, Thorell A, et al. Adherence to the enhanced recovery after surgery protocol and outcomes after colorectal cancer surgery. Arch Surg 2011;146:571-7. [Crossref] [PubMed]
- Varadhan KK, Lobo DN. A meta-analysis of randomised controlled trials of intravenous fluid therapy in major elective open abdominal surgery: getting the balance right. Proc Nutr Soc 2010;69:488-98. [Crossref] [PubMed]
- Ahn HJ, Kim JA, Lee AR, et al. The risk of acute kidney injury from fluid restriction and hydroxyethyl starch in thoracic surgery. Anesth Analg 2016;122:186-93. [Crossref] [PubMed]
- Ishikawa S, Griesdale DEG, Lohser J. Acute kidney injury after lung resection surgery: incidence and perioperative risk factors. Anesth Analg 2012;114:1256-62. [Crossref] [PubMed]
- Licker M, Cartier V, Robert J, et al. Risk factors of acute kidney injury according to RIFLE criteria after lung cancer surgery. Ann Thorac Surg 2011;91:844-50. [Crossref] [PubMed]
- Brienza N, Giglio MT, Marucci M, et al. Does perioperative hemodynamic optimization protect renal function in surgical patients? A meta-analytic study. Crit Care Med 2009;37:2079-90. [Crossref] [PubMed]
- Kheterpal S, Tremper KK, Englesbe MJ, et al. Predictors of postoperative acute renal failure after noncardiac surgery in patients with previously normal renal function. Anesthesiology 2007;107:892-902. [Crossref] [PubMed]
- Brandstrup B, Svendsen PE, Rasmussen M, et al. Which goal for fluid therapy during colorectal surgery is followed by the best outcome: near-maximal stroke volume or zero fluid balance? Br J Anaesth 2012;109:191-9. [Crossref] [PubMed]
- Brandstrup B, Tønnesen H, Beier-Holgersen R, et al. Effects of intravenous fluid restriction on postoperative complications: comparison of two perioperative fluid regimens: a randomized assessor-blinded multicenter trial. Ann Surg 2003;238:641-8. [Crossref] [PubMed]
- Evans RG, Naidu B. Does a conservative fluid management strategy in the perioperative management of lung resection patients reduce the risk of acute lung injury? Interact Cardiovasc Thorac Surg 2012;15:498-504. [Crossref] [PubMed]
- Soni N. British consensus guidelines on intravenous fluid therapy for adult surgical patients (GIFTASUP): Cassandra’s view. Anaesthesia 2009;64:235-8. [Crossref] [PubMed]
- McCluskey SA, Karkouti K, Wijeysundera D, et al. Hyperchloremia after noncardiac surgery is independently associated with increased morbidity and mortality: a propensity-matched cohort study. Anesth Analg 2013;117:412-21. [Crossref] [PubMed]
- Young P, Bailey M, Beasley R, et al. Effect of a buffered crystalloid solution vs saline on acute kidney injury among patients in the intensive care unit: the SPLIT randomized clinical trial. JAMA 2015;314:1701-10. [Crossref] [PubMed]
- Moretti EW, Robertson KM, El-Moalem H, et al. Intraoperative colloid administration reduces postoperative nausea and vomiting and improves postoperative outcomes compared with crystalloid administration. Anesth Analg 2003;96:611-7. [PubMed]
- Martin C, Jacob M, Vicaut E, et al. Effect of waxy maize-derived hydroxyethyl starch 130/0.4 on renal function in surgical patients. Anesthesiology 2013;118:387-94. [Crossref] [PubMed]
- Gutierrez MC, Moore PG, Liu H. Goal-directed therapy in intraoperative fluid and hemodynamic management. J Biomed Res 2013;27:357-65. [PubMed]
- Suehiro K, Okutani R. Influence of tidal volume for stroke volume variation to predict fluid responsiveness in patients undergoing one-lung ventilation. J Anesth 2011;25:777-80. [Crossref] [PubMed]
- Diaper J, Ellenberger C, Villiger Y, et al. Transoesophageal Doppler monitoring for fluid and hemodynamic treatment during lung surgery. J Clin Monit Comput 2008;22:367-74. [Crossref] [PubMed]
- Marik PE, Cavallazzi R, Vasu T, et al. Dynamic changes in arterial waveform derived variables and fluid responsiveness in mechanically ventilated patients: a systematic review of the literature. Crit Care Med 2009;37:2642-7. [Crossref] [PubMed]
- Suehiro K, Okutani R. Stroke volume variation as a predictor of fluid responsiveness in patients undergoing one-lung ventilation. J Cardiothorac Vasc Anesth 2010;24:772-5. [Crossref] [PubMed]
- Piccioni F, Bernasconi F, Tramontano GT, et al. A systematic review of pulse pressure variation and stroke volume variation to predict fluid responsiveness during cardiac and thoracic surgery. J Clin Monit Comput 2017;31:677-84. [Crossref] [PubMed]
- Bjerregaard LS, Møller-Sørensen H, Hansen KL, et al. Using clinical parameters to guide fluid therapy in high-risk thoracic surgery. A retrospective, observational study. BMC Anesthesiol 2015;15:91. [Crossref] [PubMed]
- Feldheiser A, Conroy P, Bonomo T, et al. Development and feasibility study of an algorithm for intraoperative goaldirected haemodynamic management in noncardiac surgery. J Int Med Res 2012;40:1227-41. [Crossref] [PubMed]
- Chau EH, Slinger P. Perioperative fluid management for pulmonary resection surgery and esophagectomy. Semin Cardiothorac Vasc Anesth 2014;18:36-44. [Crossref] [PubMed]
- Giménez-Milà M, Klein AA, Martinez G. Design and implementation of an enhanced recovery program in thoracic surgery. J Thorac Dis 2016;8:S37-45. [PubMed]
- Katlic MR. Video-assisted thoracic surgery utilizing local anesthesia and sedation. Eur J Cardiothorac Surg 2006;30:529-32. [Crossref] [PubMed]
- Al-Abdullatief M, Wahood A, Al-Shirawi N, et al. Awake anaesthesia for major thoracic surgical procedures: an observational study. Eur J Cardiothorac Surg 2007;32:346-50. [Crossref] [PubMed]
- Deng HY, Zhu ZJ, Wang YC, et al. Non-intubated video-assisted thoracoscopic surgery under loco-regional anaesthesia for thoracic surgery: a meta-analysis. Interact Cardiovasc Thorac Surg 2016;23:31-40. [Crossref] [PubMed]
- Guo Z, Shao W, Yin W, et al. Analysis of feasibility and safety of complete video-assisted thoracoscopic resection of anatomic pulmonary segments under non-intubated anesthesia. J Thorac Dis 2014;6:37-44. [PubMed]
- Pompeo E, Sorge R, Akopov A, et al. Non-intubated thoracic surgery working group. non-intubated thoracic surgery-a survey from the european society of thoracic surgeons. Ann Transl Med 2015;3:37. [PubMed]
- Kao MC, Lan CH, Huang CJ. Anesthesia for awake video-assisted thoracic surgery. Acta Anaesthesiol Taiwan 2012;50:126-30. [Crossref] [PubMed]
- Pompeo E. Awake thoracic surgery--is it worth the trouble? Semin Thorac Cardiovasc Surg 2012;24:106-14. [Crossref] [PubMed]
- Liu J, Cui F, Li S, et al. Nonintubated video-assisted thoracoscopic surgery under epidural anesthesia compared with conventional anesthetic option: a randomized control study. Surg Innov 2015;22:123-30. [Crossref] [PubMed]
- Pompeo E, Tacconi F, Mineo D, et al. The role of awake video-assisted thoracoscopic surgery in spontaneous pneumothorax. J Thorac Cardiovasc Surg 2007;133:786-90. [Crossref] [PubMed]
- Pompeo E, Mineo TC. Awake operative videothoracoscopic pulmonary resections. Thorac Surg Clin 2008;18:311-20. [Crossref] [PubMed]
- Tacconi F, Pompeo E, Sellitri F, et al. Surgical stress hormones response is reduced after awake videothoracoscopy. Interact Cardiovasc Thorac Surg 2010;10:666-71. [Crossref] [PubMed]
- Chen JS, Cheng YJ, Hung MH, et al. Nonintubated thoracoscopic lobectomy for lung cancer. Ann Surg 2011;254:1038-43. [Crossref] [PubMed]
- Pompeo E. Nonintubated video-assisted thoracic surgery under epidural anesthesia-encouraging early results encourage randomized trials. Chin J Cancer Res 2014;26:364-7. [PubMed]
- Piccioni F, Langer M, Fumagalli L, et al. Thoracic paravertebral anaesthesia for awake video-assisted thoracoscopic surgery daily. Anaesthesia 2010;65:1221-4. [Crossref] [PubMed]


