Call for screening for primary aldosteronism: an underdiagnosed and treatable disease
Recent studies have raised the important issue of prevalence and underdiagnosed of primary aldosteronism (PA) in primary care setting. The crucial role of a correct diagnosis of PA is demonstrated by current studies that aldosterone over-secretion is not only resulted in cardiovascular and renal damage (1,2) but also associated with adverse metabolic complication, including insulin resistance, type 2 diabetes mellitus, and osteoporosis (3-5). Monticone et al. had addressed the issue that PA is a frequent cause of secondary hypertension even in the general hypertensive population and indicates that the majority of hypertensive patients should be screened for PA (6).
Most experts previously described PA to be less than 1% of patients with mild-to-moderate essential hypertension (3-5); however, mounting evidence has refuted these assumptions. A commonly accepted prevalence of PA is about 5–10% of patients with hypertension (3-5). There are several reasons of major underestimate of PA prevalence—most physicians were being taught that PA is a rare and relatively benign condition, and had assumed hypokalemia (only about one-third of the patients with PA presented with hypokalemia) was a prerequisite for diagnosis of PA; the cost-effectiveness to screen for PA patients and subsequent confirmation and lateralization of PA (7), and unawareness or ignoring the mounting evidence of prevalence and the consequences of substantially higher risk profile of untreated PA (3-5). The 2016 Endocrine Society’s Guideline for the management of PA (8) indicated that PA is a major public health issue requiring immediate recognition and coordinated action. The reasons are because of its underestimated prevalence, and patients with PA have higher cardiovascular morbidity and mortality than age-matched, sex-matched, and blood pressure-matched patients with essential hypertension (3-5). Furthermore, more and more evidence revealed that adrenalectomy of PA showed better survival benefits than just received medical treatment (9).
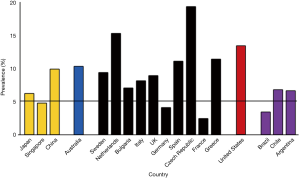
A recent extensive meta-analysis had investigated the prevalence of PA after introduction of the aldosterone-to-renin ratio (ARR) as a screening test for PA and have reported wide variations of 1% to 29.8% in 30 referral centers and 3.2% to 12.7% in 9 primary care settings (10). The heterogeneity of studies was too high to establish cross -sectional estimates of the prevalence of PA, and probably biased by the characteristics of the selected participants, various diagnostic criteria and variability of testing method. The majority of studies were conducted in tertiary referral centers and referral bias is likely to have affected the results. Only nine studies have been conducted on patients from primary care centers (10), which represent an apparently unselected hypertensive population. For this reason, the actual prevalence of PA among the general hypertensive population and the importance of extending the measurement of the ARR in most hypertensive patients, are still a matter of continuing debate. Figure 1 showed PA prevalence of 40 cohorts with confirmation test to verify the diagnosis of PA across different countries according to articles on the prevalence of PA published between January 1, 1990 and July, 2017. A wide variation of 2.3% to 19.2% across different countries was shown. In addition, Figure 2 demonstrated a world map graphs showing the percentage of prevalence with a wide variation of 5.3% to 13.3% over five world regions. Similarly, this might be explained by various characteristics of the study populations and setting, different diagnostic thresholds and variability of testing conditions and assays adopted in different countries.

It is plausible that prospective study with a pre-defined protocol and large cohort are more appropriate to estimate prevalence. Monticone et al. (6) demonstrated the prevalence of PA increased with the severity of hypertension, ranging from 3.9% in stage I [21% aldosterone-producing adenoma (APA)], 9.7% in stage II (30% APA) to 11.8% in stage III (40% APA), which is consistent with previous study (11).
The 2016 Endocrine Society’s Guideline for the management of PA (8) does not provide a gold standard confirmatory test for PA. Confirmatory testing is very important because it spares non-PA patients from undergoing costly and invasive lateralization procedures. Four testing procedures (oral sodium loading test, saline infusion test, fludrocortisone suppression test, and captopril test) are widespread adopted. Different confirmation tests were selected to utilize by different world regions. There is still lack of concrete and enough evidence to recommend one over all the others because no single confirmation test is most favorable in terms of sensitivity, specificity, and reliability. Cost, patient adherence, laboratory routine, and local expertise were the main factors generally affected the preference of confirmatory test (8).
Previous studies proposed that considerably less than 1% of the hypertensive patients are screened for PA each year, not to mention diagnosed and properly treated (3-5). Early diagnosis and targeted treatment of PA are crucial to increase the chance of improvement and even cure of hypertension, and for preventing cardiovascular complications (3-5). Progress will be greatly enhanced by recognition of the prevalence issue.
Acknowledgements
The authors thank Dr. I-Shiang Tzeng (Department of Research, Taipei Tzu Chi Hospital, Buddhist Tzu Chi Medical Foundation, New Taipei City) for his help in making figure.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Wu VC, Yang SY, Lin JW, et al. Kidney impairment in primary aldosteronism. Clin Chim Acta 2011;412:1319-25. [Crossref] [PubMed]
- Lin YH, Lin LY, Chen A, et al. Adrenalectomy improves increased carotid intima-media thickness and arterial stiffness in patients with aldosterone producing adenoma. Atherosclerosis 2012;221:154-9. [Crossref] [PubMed]
- Fallo F, Veglio F, Bertello C, et al. Prevalence and characteristics of the metabolic syndrome in primary aldosteronism. J Clin Endocrinol Metab 2006;91:454-9. [Crossref] [PubMed]
- Wu VC, Chueh SJ, Chen L, et al. Risk of new-onset diabetes mellitus in primary aldosteronism: a population study over 5 years. J Hypertens 2017;35:1698-708. [Crossref] [PubMed]
- Wu VC, Chang CH, Wang CY, et al. Risk of Fracture in Primary Aldosteronism: A Population-Based Cohort Study. J Bone Miner Res 2017;32:743-52. [Crossref] [PubMed]
- Monticone S, Burrello J, Tizzani D, et al. Prevalence and Clinical Manifestations of Primary Aldosteronism Encountered in Primary Care Practice. J Am Coll Cardiol 2017;69:1811-20. [Crossref] [PubMed]
- Lubitz CC, Economopoulos KP, Sy S, et al. Cost-Effectiveness of Screening for Primary Aldosteronism and Subtype Diagnosis in the Resistant Hypertensive Patients. Circ Cardiovasc Qual Outcomes 2015;8:621-30. [Crossref] [PubMed]
- Funder JW, Carey RM, Mantero F, et al. The Management of Primary Aldosteronism: Case Detection, Diagnosis, and Treatment: An Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab 2016;101:1889-916. [Crossref] [PubMed]
- Wu VC, Wang SM, Chang CH, et al. Long term outcome of Aldosteronism after target treatments. Sci Rep 2016;6:32103. [Crossref] [PubMed]
- Käyser SC, Dekkers T, Groenewoud HJ, et al. Study Heterogeneity and Estimation of Prevalence of Primary Aldosteronism: A Systematic Review and Meta-Regression Analysis. J Clin Endocrinol Metab 2016;101:2826-35. [Crossref] [PubMed]
- Rossi GP, Bernini G, Caliumi C, et al. A prospective study of the prevalence of primary aldosteronism in 1,125 hypertensive patients. J Am Coll Cardiol 2006;48:2293-300. [Crossref] [PubMed]


