Early diagnosis of solitary pulmonary nodules
With the development of equipment and technology, solitary pulmonary nodules (SPNs) are being increasingly detected year by year. The reported detection rate of SPNs is about 8-51% (1). The differentiation between benign and malignant nodules, and the management thereof, has thus become the main focus of interest and challenge in clinical research nowadays. The goal is to rapidly identify the nature of a pulmonary nodule, making early detection and treatment possible, and in turn avoid unnecessary invasive examination or open-chest surgery for benign lesions. Based on the clinical experience regarding the diagnosis and treatment of SPNs in the past decade in our department, we presented the techniques and advancement in the early diagnosis of SPNs in recent years in this study, as follows.
Overview of the early diagnosis
Definition and etiology of SPNs
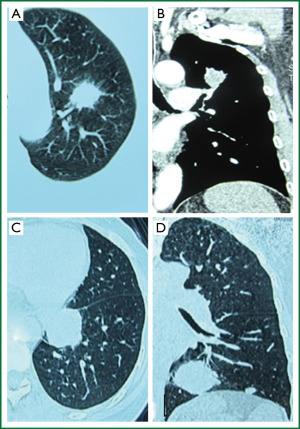
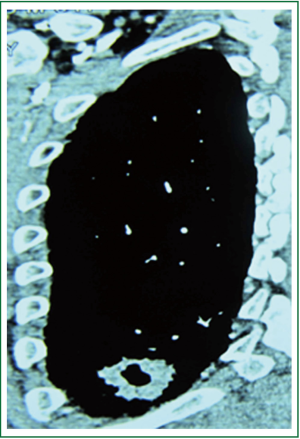
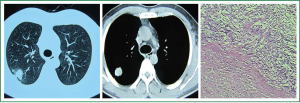
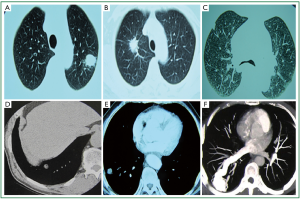
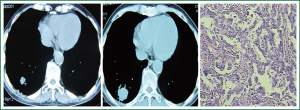
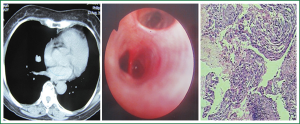
A SPN is an isolated, single lesion in a round or oval shape with a diameter of ≤3 cm in lung parenchyma, surrounded entirely by gas-containing lung tissue. Such lesions are not accompanied by lung atelectasis, hilar enlargement or pleural effusion (2,3) (Figure 1). Despite a variety of causes, SPNs are common in granulomatous diseases and lung cancer, and not often seen in carcinoid tumors or a single lung metastasis of other tumors. It is rare in hamartomas and pulmonary arteriovenous malformations (Figure 2).
Risk factors of lung cancer in SPNs
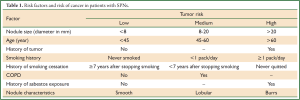
When a pulmonary nodule is detected, the probability of malignancy should be evaluated first. The clinical evaluation includes a review of medical history and examination of physical sign. Clinical risk factors indicating a high probability of malignancy include the size of nodule, age, history of tumor, COPD, smoking history, and history of asbestos exposure (See Table 1) (4).
Full table
Common non-invasive examination of SPNs
Commonly used non-invasive tests of SPNs include: sputum cell biology techniques, blood biomarker detection and imaging.
Sputum cell biology techniques
Sputum cytology is a non-invasive and simple cytological test, with a sensitivity of 28-80% for early diagnosis of lung cancer. Due to certain restrictions, however, the positive rate in the diagnosis of SPNs is not high. In recent years, thin liquid based cytology has been introduced, but it still can not meet the clinical demands. The detection of DNA ploidy changes in sputum cytology can help increase the early diagnosis rate of malignant pulmonary nodules.
Detection of biomarkers
These mainly include a number of tumor markers, such as carcinoembryonic antigen (CEA), neuron-specific enolase (NSE), cytokeratin 19 fragment (Cyfra21-1), carbohydrate antigen (CA125), lung cancer-associated antigens, vascular endothelial growth factors, proliferating cell nuclear antigens and epidermal growth factor receptors, which have attracted a wide range of interests. Detecting a single marker is of limited value in the diagnosis of malignant lesions, and the combined use of multiple markers is thus preferred. It has been reported (5) that malignant SPNs have significantly elevated tumor marker values compared with benign SPNs. In cases with SPNs, serum CEA and Cyfra21-1 are highly sensitive indicators of lung cancer, and the combination of both is helpful in differentiating the benign and malignant lesions.
Imaging techniques
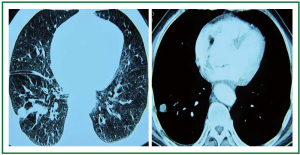
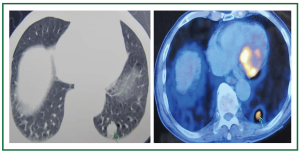
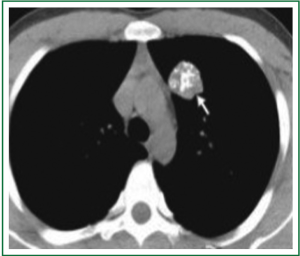
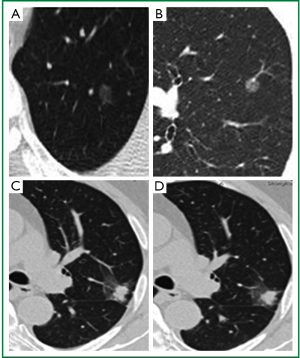
(I) Chest radiographs (CR) are commonly used in chest examination. Most patients are often found to have SPNs through this method. According to foreign reports, the examination pulmonary nodules rate on CR is about 0.09-0.2% (6) (Figure 3); (II) computed tomography (CT) is currently considered the most sensitive imaging examination of lung nodules. In particular, the introduction of multi-slice CT has greatly improved the detection rate and qualitative accuracy in the diagnosis of pulmonary nodules (Figure 4); (III) positron emission computed tomography (PET): PET/CT combines PET that reflects the metabolic capacity of a tumor and CT that shows the organizational structure in a high-resolution way. It has a sensitivity of 97% and a specificity of 85% to SPNs, and is recognized as the optimal non-invasive means of differentiating benign SPNs from malignant ones (7). According to most studies, the maximum standardized uptake value (SUVmax) of 2.5 is used as a diagnostic threshold, in which a SUVmax of ≥2.5 is suggestive of malignancy (Figure 5); Malignancies with a SUVmax of ≤2.5 are often bronchioloalveolar carcinoma and metastatic carcinoid tumors. For SPNs ≤1 cm in diameter, a SUVmax of ≥2.5 is not highly accurate in the diagnosis of malignancy. False positive results can occur in granulomatous inflammation, fungal infections, tuberculosis, or other active inflammation.
Imaging characteristics and assessment of probability of malignancy
Imaging parameters used to assess the risk of pulmonary nodules include the nodule size, margin characteristics, density, and peripheral signs.
Size
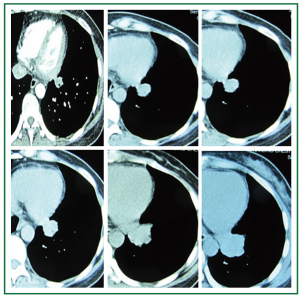
Generally, small nodules tend to be benign, while larger ones are more likely malignant (Figure 6). The probability of malignancy is less than 1% in nodules <4 mm; and around 0.9%, 18% and 50% in those of 4-7 mm, 8-20 mm and 20-30 mm, respectively (8). Therefore, the SPN diameter can be used as an independent risk factor for differentiating malignant and benign lesions.
Edge characteristics
The edge characteristics provide an important basis for the differentiation between benign and malignant nodules. Malignant SPNs are often associated with irregular contours, spiculated edge and increased lobes (Figures 7,8). In a clinical prediction model based on Logistic regression analysis, Swensen et al. (9) established that lobulation has a positive predictive value of 88-94% for malignant nodules, and can be used as an independent risk factor for malignant nodules. Lindell et al. (10) analyzed lung cancer screening results for five years, and found margin changes in 42% of tumors with progression, of which 80% was lobulation and increased burrs. However, nearly 25% of benign nodules have lobulated edge as well (11).
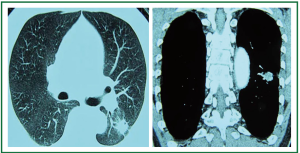
Density
Calcification is considered to be an important imaging characteristic for differentiation of malignant and benign lesions. A study reported (12) that benign and malignant SPNs accounted for 97% and 3%, respectively, in 504 patients with calcified nodules, and 29% and 71% in 1,109 patients without calcification, respectively. Popcorn-like calcification is often associated with hamartoma (Figure 9). Calcification is, however, still present in about 2-13% of nodular lung cancer, 33% of carcinoid tumors and other malignancies (13). Fat-containing nodules are a specific diagnostic sign of hamartoma, but can also be present in a small part of malignancies (14).
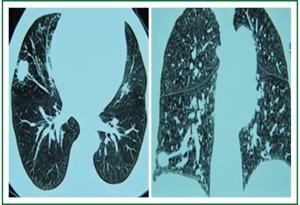
The uneven density of solid nodules is mainly reflected as the vacuole sign, air bronchogram and cavity. Vacuoles and aerated bronchioles are significantly more frequently seen in lung cancer compared with benign nodules (Figure 10). As reported (15), vacuoles are present in 28.7% of lung cancer in a size of <3 cm, while those ≤2 cm in diameter account for 60.4%. In contrast, only 8.5% of lesions with this sign are benign. According to the report by Kui et al. (16), of 132 SPN patients, 30% patients with lung cancer had aerated bronchi, while benign lesions presented only 5.9%. Lung cavities are not as often seen in small lung cancer as tuberculoma. A cavity in lung cancer is mostly eccentric with uneven wall thickness (Figure 11).
Compared with solid nodules, ground-glass opacities (GGOs) or semi-solid pulmonary nodules are more likely malignant. According to a report (17), 75% GGOs are bronchioloalveolar carcinoma or adenocarcinoma with bronchioloalveolar carcinoma as the primary component, 6% atypical adenomatous hyperplasia, and approximately 19% benign lesions (Figure 12).
Peripheral signs
The vessel convergence sign is often seen in peripheral lung cancer (18), and in 83-94.8% malignant SPNs (Figure 13). Pleural indentation is present in 49% lung cancer, all of which are peripheral lung cancer, mostly adenocarcinoma and alveolar cell carcinoma (19) (Figure 14). Satellite lesions around a SPN are commonly indicative of granulomatous inflammation in the lung (Figure 15).
Growth rate
The growth rate of nodules is commonly evaluated with the volume doubling time. If a lesion grows significantly in volume, it tends to be malignancy and often has a doubling time of about 30-400 days (20). Those with a doubling time longer than 400 days are often benign tumors or granulomatous inflammation due to pulmonary infections (21) (Figure 16).
Minimally invasive techniques for early diagnosis in medical departments
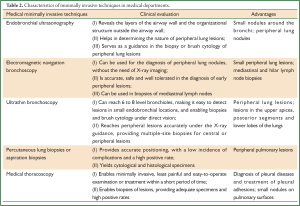
Medical minimally invasive techniques for the early diagnosis of SPNs include: fiber optic bronchoscopy (FOB), percutaneous lung biopsy or needle aspiration biopsy, and medical thoracoscopy (Table 2).
Full table
Fiber optic bronchoscopy (FOB)
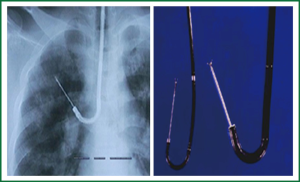
FOB-based pathological techniques for the diagnosis of SPNs include bronchial brush cytology (BB), bronchial alveolar lavage (BAL) and transbronchial lung biopsy (TBLB) (Figure 17). When a SPN is ≤2 cm in diameter, especially located in the outer 1/3 field of the lungs, its diagnostic accuracy is merely 14% (22). The development of endobronchial ultrasound, ultrathin bronchoscopy and electromagnetic navigation has improved the sensitivity of TBLB.
Endobronchial ultrasonography (EBUS)
Sends the ultrasound probe into the tracheal and bronchial lumens through bronchoscope, and achieves the images through real-time ultrasound scanning of the trachea, bronchial wall layers and surrounding organs and vessels. It can be used to identify the abnormal changes of submucosal, wall and peripheral airway lesions and locate peripheral lesions (Figure 18). Depending on the ultrasound probe type, EBUS can be divided into radial probes (RPs) and convex probes (CPs). RP-EBUS has a smaller diameter, and thus can be put through the bronchoscope to the target area, which is mainly used to examine peripheral lesions, but can not be used for lesion biopsies under real-time monitoring. CP-EBUS combines ultrasound probe and the distal end of the endoscope, enabling lesion biopsies under real-time monitoring with significantly improved accuracy and safety of the puncture. It is mainly used for observations and biopsies of large airway walls and the surrounding lesions. According to a report (23), transbronchial biopsy using endobronchial ultrasonography with a guide sheath (TBLB-EBUS-GS) has a diagnosis rate of 77% for peripheral lung lesions and, in particular, 74% for those with a diameter ≤3 cm. Yamada et al. (24) reported that TBLB-EBUS-GS had a diagnosis rate of 67% for peripheral lung nodules, and proposed that, to maximize the diagnostic accuracy, at least five biopsies should be carried out. Apparently, EBUS has significantly improved the diagnosis level of peripheral lung nodules.
Electromagnetic navigation bronchoscopy (ENB)
Integrates ENB to empower three-dimensional spiral CT image reconstruction and labeling. With combination of the obtained 3D simulated images and the bronchoscopic images, guidance is achieved through observation of the orientation of catheters with electromagnetic positioning sensors at the top so that the catheters can reach the specified position in the lungs for biopsies. It has been reported (25) that ENB has a diagnosis rate of 67% for peripheral lung lesions.
Ultrathin bronchoscopy (UB)
Refers to bronchoscopes with an outer diameter of less than 3.0 mm, UB diameter of up to 1.8 mm and biopsy pipeline of 1.2 mm. In theory, they are able to reach into the peripheral bronchi. UB is a powerful tool for the diagnosis of peripheral lung lesions, particularly under the effective guidance of a navigation system. As UB plays its superior performance when inserted into the specific locations, it can not only detect peripheral lesions in the distal ends of the bronchial tree, but also collect the specimens, which improve the diagnostic capacity of peripheral lung lesions (Figure 19). Yamamoto et al. (26) suggested in a study that UB could be an effective supplementary option to conventional bronchoscopy for the diagnosis of peripheral lung lesions. They also pointed out that, for lesions in the upper apices, posterior segments and lower lobes of the lungs, UB could be considered as the preferred examination.
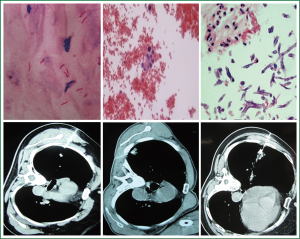
Fine-needle aspiration biopsy (FNAB)
FNAB is a common method for lung tissue biopsies in clinical settings, particularly for SPNs located close to the chest wall. The mainstream needles include aspiration needles and cutting needles (Figure 20). Both can be used to obtain cytological and histological specimens. While those obtained by the former are smaller, incomplete and easily crushed, which may compromise the pathological findings, those with the latter type are more complete and useful for observing changes in the organizational structure. CT has a high spatial and density resolution, and clearly shows the lesion size, density, location and the spatial relationship between the lesion and surrounding organs, which facilitates the selection of the optimal puncture site, measurement of the distance and angle of the site relative to the lesion, thereby greatly improving the accuracy of the puncture. In particular, CT guidance has its unique value for smaller lesions. A meta-analysis (27) reports that FNAB diagnosis has a sensitivity of 86% and specificity of 98.8% for malignant SPNs, while combination with CT-guided puncture will add up to a sensitivity of 91% and specificity of 94% (28). The diagnostic accuracy mainly depends on the operator’s positioning and puncturing skills, in addition to the pathology technical level that may have a certain impact on the results. The main contraindications of FNAB are: severe pulmonary congestion or hyperemia; severe airway obstruction; severe cardiopulmonary dysfunction; severe coagulation disorders or active large hemoptysis; suspected vascular lesions, such as vascular malformations and aneurysm; inability to maintain a constant position for long; and inability to hold breath or be cooperative in surgery. The complications of FNAB include pneumothorax, hemoptysis, needle tract seeding of tumors and air embolism in other organs.
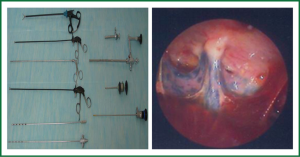
Medical thoracoscopy
Medical thoracoscopy, as opposed to video-assisted thoracoscopic surgery (VATS), is operated by physicians of the respiratory department in the endoscopy room, which enables minimally invasive, least painful, and easy-to-operate examination or treatment within a short period of time (Figure 21). It is mainly used for the diagnosis of pleural disease and treatment of pleural adhesions, and has certain value for examinations of unexplained peripheral lung lesions, as it is helpful in obtaining large parenchymal biopsy specimens. Attention should be paid to follow the indications strictly. Closed chest cavity due to pleural adhesions and pulmonary hypertension, honeycomb lung and vascular tumors during lung biopsies are absolute contraindications; severe cough, hypoxemia, coagulopathy and severe heart diseases are relative contraindications.
Video-assisted thoracoscopic surgery (VATS)
Following the above methods, when the diagnosis is still inconclusive and the imaging findings clearly suggest malignant SPNs, VATS inspection can be considered if there is no contraindication. VATS is advantageous in its minimally invasive nature, adequate exposure, image clarity, fewer complications and low mortality, and is thus an ideal method for the diagnosis and management of SPNs (29). To address the challenges for SPN diagnosis and management and intraoperative positioning particularly in deep lung lesions, <1 cm nodules, and GGO under VATS at present, such techniques have been reported (30) as anatomical positioning, technology imaging, CT guided catheter Hook Wire positioning, methylene blue injection, and intraoperative ultrasound positioning. In the case of difficulties in applying VATS treatment, diagnostic surgical thoracotomy can be performed.
In short, SPNs are still one of the challenges for clinical diagnosis and treatment of pulmonary lesions. With the increasing development of imaging, ultrasound and bronchoscopic techniques, the diagnosis and treatment levels of SPN will be greatly improved. The combination of biomarkers and other means will be a trend of development in the future.
Acknowledgements
The study was supported by a grant from “Twelve-Five Plan’’ the Major Program of Nanjing Medical Science and Technique Development Foundation (Molecular Mechanism Study on Metastasis and Clinical Efficacy Prediction of Non-small Cell Lung Cancer) and Third Level Training Program of Young Talent Project of Nanjing Health, Nanjing Medical Science and Technology Development Project (QRX11226), and Young Professionals Foundation of Nanjing Chest Hospital.
Disclosure: The authors declare no conflict of interest.
References
- Albert RH, Russell JJ. Evaluation of the solitary pulmonary nodule. Am Fam Physician 2009;80:827-31. [PubMed]
- Ost D, Fein AM, Feinsilver SH. Clinical practice. The solitary pulmonary nodule. N Engl J Med 2003;348:2535-42. [PubMed]
- Dargan EL. The enigma of the solitary pulmonary nodule. J Natl Med Assoc 1973;65:101-3 passim. [PubMed]
- Goo JM, Park CM, Lee HJ. Ground-glass nodules on chest CT as imaging biomarkers in the management of lung adenocarcinoma. AJR Am J Roentgenol 2011;l96:533-43.
- Bekci TT, Senol T, Maden E. The efficacy of serum carcinoembryonic antigen (CEA), cancer antigen 125 (CA125), carbohydrate antigen 19-9 (CA19-9), carbohydrate antigen 15-3 (CA15-3), alpha-fetoprotein (AFP) and human chorionic gonadotropin (hCG) levels in determining the malignancy of solitary pulmonary nodules. J Int Med Res 2009;37:438-45. [PubMed]
- Gould MK, Fletcher J, Iannetoni MD, et al. Evaluation of patients with pulmonary nodules: when is it lung cancer?: ACCP evidence-based clinical practice guidelines (2nd edition). Chest 2007;132:108S-130S.
- Kim SK, Allen-Auerbach M, Goldin J, et al. Accuracy of PET/CT in characterization of solitary pulmonary lesions. J Nucl Med 2007;48:214-20. [PubMed]
- Tang AW, Moss HA, Robertson RJ. The solitary pulmonary nodule. Eur J Radiol 2003;45:69-77. [PubMed]
- Swensen SJ, Silverstein MD, Ilstrup DM, et al. The probability of malignancy in solitary pulmonary nodules. Application to small radiologically indeterminate nodules. Arch Intern Med 1997;157:849-55. [PubMed]
- Lindell RM, Hartman TE, Swensen SJ, et al. Five-year lung cancer screening experience: CT appearance, growth rate, location, and histologic features of 61 lung cancers. Radiology 2007;242:555-62. [PubMed]
- Leef JL 3rd, Klein JS. The solitary pulmonary nodule. Radiol Clin North Am 2002;40:123-43. [PubMed]
- Colice GL. Chest CT for known or suspected lung cancer. Chest 1994;106:1538-50. [PubMed]
- Choromańska A, Macura KJ. Evaluation of solitary pulmonary nodule detected during computed tomography examination. Pol J Radiol 2012;77:22-34. [PubMed]
- Beigelman-Aubry C, Hill C, Grenier PA. Management of an incidentally discovered pulmonary nodule. Eur Radiol 2007;17:449-66. [PubMed]
- Chen N, Xie P, Fu K. The value of vacuole sign in the early diagnosis of lung cancer. Yi Xue Ying Xiang Xue Za Zhi 2012;12:13-5.
- Kui M, Templeton PA, White CS, et al. Evaluation of the air bronchogram sign on CT in solitary pulmonary lesions. J Comput Assist Tomogr 1996;20:983-6. [PubMed]
- Kim HY, Shim YM, Lee KS, et al. Persistent pulmonary nodular ground-glass opacity at thin-section CT: histopathologic comparisons. Radiology 2007;245:267-75. [PubMed]
- Shen M, Lin J, Chen N, et al. Evaluation of vascular convergence sign (VCS) with multi-slice spiral computed tomography in diagnosing peripheral lung cancer. Zhongguo Lin Chuang Yi Xue 2008;15:247-8.
- Li M, Ito H, Wada H, et al. Pit-fall sign on computed tomography predicts pleural involvement and poor prognosis in non-small cell lung cancer. Lung Cancer 2004;46:349-55. [PubMed]
- Lillington GA, Caskey CI. Evaluation and management of solitary and multiple pulmonary nodules. Clin Chest Med 1993;14:111-9. [PubMed]
- Truong MT, Sablof BS, Ko JP. Multidetector CT of solitary pulmonary nodules. Thorac Surg Clin 2010;20:9-23. [PubMed]
- Baaklini WA, Reinoso MA, Gorin AB, et al. Diagnostic yield of fberoptic bronchoscopy in evaluating solitary pulmonary nodules. Chest 2000;117:1049-54. [PubMed]
- Kurimoto N, Miyazawa T, Okimasa S, et al. Endobronchial ultrasonography using a guide Sheath increases the ability to diagnose peripheral pulmonary lesions endoscopically. Chest 2004;126:959-65. [PubMed]
- Yamada N, Yamazaki K, Kurimoto N, et al. Factors related to diagnostic yield of transbronchial biopsy using endobronchial ultrasonography with a guide sheath in small peripheral pulmonary lesions. Chest 2007;132:603-8. [PubMed]
- Eberhardt R, Anantham D, Herth F, et al. Electromagnetic navigation diagnostic bronchoscopy in peripheral lung lesions. Chest 2007;131:1800-5. [PubMed]
- Yamamoto S, Ueno K, Imamura F, et al. Usefulness of ultrathin bronchoscopy in diagnosis of lung cancer. Lung Cancer 2004;46:43-8. [PubMed]
- Lacasse Y, Wong E, Guyatt GH, et al. Transthoracic needle aspiration biopsy for the diagnosis of localised pulmonary lesions: a meta-analysis. Thorax 1999;54:884-93. [PubMed]
- Cheung JY, Kim Y, Shim SS, et al. Combined fluoroscopy- and CT-guided transthoracic needle biopsy using a C-arm cone-beam CT system: comparison with fluoroscopy-guided biopsy. Korean J Radiol 2011;12:89-96. [PubMed]
- Congregado Loscertales M, Girón Arjona JC, Jiménez Merchán R, et al. Usefulness of video-assisted thoracoscopy for the diagnosis of solitary pulmonary nodules. Arch Bronconeumol 2002;38:415-20. [PubMed]
- Zaman M, Bilal H, Woo CY, et al. In patients undergoing video-assisted thoracoscopic surgery excision, what is the best way to locate a subcentimetre solitary pulmonary nodule in order to achieve successful excision? Interact Cardiovasc Thorac Surg 2012;15:266-72. [PubMed]