Histological subtypes of solitary pulmonary nodules of adenocarcinoma and their clinical relevance
Solitary pulmonary nodules (SPNs) are a group of single, opaque, and small (diameter ≤3 cm) lesions, characterized by dense shadows in the pulmonary X-ray picture. They are usually surrounded by the air-containing lung tissue but without obstructive pneumonia, atelectasis, pulmonary hilar enlargement, or pleural effusion (1,2). The causes of SPNs are diverse but mainly include granulomatous disease and bronchopulmonary cancer; in rare cases, they can also be resulted from carcinoids or the single lung metastasis of other tumors. Once SPNs are confirmed to be lung cancer, they are often still in stage 1, and the patients often can be cured or have a long survival after proper treatment (3). Compared with the squamous cell carcinoma, the lung adenocarcinoma, with a rapid metastasis and short clinical course, is often not sensitive to radiotherapy or chemotherapy. In 2011, the International Association for the Study of Lung Cancer (IASLC), American Thoracic Society (ATS), and European Respiratory Society (ERS) released an international muhidisciplinary classification of lung adenocarcinoma (4). The new classification is still morphology-based but also incorporated the new advances in oncology, imaging, thoracic surgery, molecular biology, and many other relevant fields, providing a new multidisciplinary classification protocol for lung adenocarcinoma. However, it has been proposed that the prognoses significantly differed when different pathological typing was applied, and the new classification-based grading/scoring system was remarkably superior in predicting the relapse/metastasis of stage 1 lung adenocarcinoma (5). Therefore, a strict subtyping of the adenocarcinoma in accordance with the new classification criteria will be clinically valuable to determine the clinical characteristics of the adenocarcinoma.
In our current study, we retrospectively analyzed the clinical data of 188 patients with pathologically confirmed SPN of adenocarcinoma (ASPN). According to the 2011 new classification protocol of lung adenocarcinoma, we subtyped all the histological sections and compared the clinicopathological features of different ASPN types.
Subjects and methods
Subjects
A total of 188 patients with pathologically confirmed invasive adenocarcinoma in our hospital from January 2007 to December 2011 were enrolled in this study. The pathologic data of these patients were reviewed, and meanwhile the clinical data including age, gender, smoking status, lymph node metastasis, as well as the sites and diameters of ASPN were collected and analyzed.
Methods
The specimens were obtained by biopsy or surgical resection, and then fixed in 10% neutral-buffer formalin solution, embedded in parafin wax, sectioned, and stained with hematoxylin and eosin (HE). The morphological and microscopic findings were described. All the histological sections were reviewed and subtyped in accordance with the 2011 lung cancer classification. All the sectioned were independently read by two experienced pathologists. If the results differed, these two pathologists jointly discussed the sections under a multi-head microscope.
Statistical analysis
The statistical analysis was performed using the SPSS 19.0 software package. Parameters were compared using chi square test, whereas the comparison of the tumor diameter was performed using univariate analysis of variance. P<0.05 was considered significantly different.
Results
Clinical features
Of these 188 patients with invasive ASPN, there were 73 men (38.8%) and 115 women (61.2%) aged 32-67 years (mean: 57 years). Seventy-eight patients (41.5%) had a history of smoking. Cancer was confirmed in the left lung in 73 cases (38.8%) and in the right lung in 115 cases (61.2%). Lymph node metastasis was detected in 69 patients (36.7%). The mean diameter of these nodules was 2.87±0.36 cm.
Histopathological findings
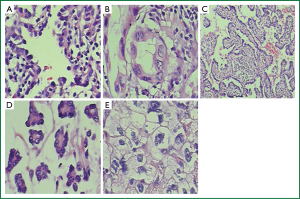
According to the new classification, there were 6 cases of lepidic predominant adenocarcinoma (LPA), 71 cases of acinar predominant adenocarcinoma (APA), 74 cases of papillary predominant adenocarcinoma (PPA), 15 cases of micorpapillary predominant adenocarcinoma (MPA), and 22 cases of solid predominant adenocarcinoma with mucin production (SPA), accounting for 3.2%, 37.8%, 39.4%, 7.9%, and 11.7%, respectively. The LPA was featured by the cancer cells with lepidic growth but without stroma, vessel, or papillary/micro-papillary structures; also, there was no cancer cell aggregation inside the alveolar cavity. The APA had round or oval glands with central lumen. The PPA was mainly composed of fibrovascular cores covered by ramified papillae. In the MPA, the tumor cells formed papillary cell clusters without fibrovascular cores. For the SPA, the tumors were mainly formed by sheet-like polygonal cells (Figure 1).
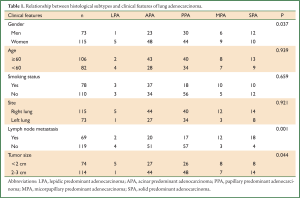
Relationship between histological subtypes and clinical features
The diameters of tumors were relatively small in LPA (mean: 1.47 cm) and PPA (mean: 1.89 cm) but were relatively large in SPA (mean: 2.54 cm), APA (mean: 2.83 cm), and MPA (mean: 2.90 cm) (P<0.05).
The LPA was more common in women (P<0.05), but was not significantly associated with age, smoking status, and sites (P>0.05).
The lymph node metastasis rate differed among different histological subtypes. It was remarkably high in SPA (81.0%) and MPA (80.0%), but was relatively low in PPA (22.9%), LPA (33.3%), and APA (28.2%) (Table 1).
Full table
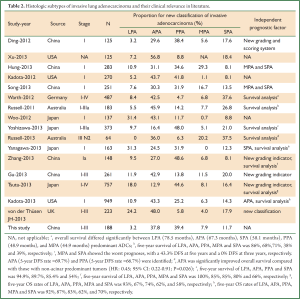
Relationship between lung adenocarcinoma histologic subtypes and clinical prognoses in literature
In 2011, the IASLC/ATS/ERS jointly released the new pathological classification criteria of lung adenocarcinoma. Since then, many clinical studies have described the new pathological classification of lung adenocarcinoma; however, the proportions of different subtypes of invasive lung adenocarcinoma as well as their prognostic relevances varied among these studies. Therefore, we searched all the clinical studies on the new pathological classification of lung adenocarcinoma and made a brief summary in Table 2. A total of 16 articles (6-21) entered the final analysis, involving the populations mainly in the United States, China, Japan, Australia, the United Kingdom, and Germany. Seven articles were focused on stage I adenocarcinoma, whereas the remaining studies were on stage I-IIIa tumors. The sample sizes of these studies ranged 64-949. Of these 16 studies, the proportions of the different subtypes of invasive lung adenocarcinoma remarkably differed: LPA, 0-31.4%; APA, 12-56.8%; PPA, 5.8-48.6%; MPA, 0-29.3%; and SPA, 8.1-20%. Obviously, APA and PPA are common subtypes, whereas LPA and MPA are less common. Thirteen studies reported the prognostic significances of different lung adenocarcinoma subtypes. Hung et al. (8) and Song et al. (10) suggested MPA and SPA are independent poor prognostic factors for lung cancer, and Kadota et al. (20) argued that APA is an independent indicator of poor prognosis for lung cancer. Ding et al. (6), Zhang et al. (17), Tsuta et al. (19), and von der Thüsen et al. (21) reported that the new classification system and the score are independent prognostic factors for lung cancer. Most studies agreed that MPA and SPA were associated with poor prognosis while LPA and APA with relatively better prognosis.
Full table
Discussion
SPNs are commonly seen in clinical practice. In a normal population census conducted by Comstock et al. (22), the incidence of SPNs reached up to 0.2%. Along with the wide application of computed tomography (CT), the detection rate of SPNs has remarkably increased. The proportions of malignant SPNs (mainly lung adenocarcinoma) varied among different articles, ranging from 5-69% (23-25). A study has confirmed that the prognoses of different lung adenocarcinoma subtypes remarkably differ. Adenocarcinoma in situ, microinvasive adenocarcinoma, and LPA tend to have “good” prognosis, PPA and APA have “relatively good” prognosis, whereas invasive mucinous adenocarcinoma, colloid carcinoma, SPA, and MPA often have “relatively poor” prognosis (5). In their study, Kadota et al. (20) enrolled 949 patients with stage I lung adenocarcinoma, and the prognostic analysis of the different subtypes showed that the 5-year survival of LPA, APA, PPA, MPA, and SPA was 100%, 85 %, 85%, 80%, and 66%, respectively. Therefore, determination of the histological subtype of a lung adenocarcinoma is helpful for predicting the prognosis.
Warth et al. demonstrated that the different histological subtype of lung adenocarcinoma is a stage-independent prognostic factor; survival differences according to patterns were influenced by adjuvant chemoradiotherapy; in particular, solid-predominant tumors had an improved prognosis with adjuvant radiotherapy. The predominant pattern was tightly linked to the risk of developing nodal metastases. As shown in our current study, the lymph node metastasis rates were high in SPA and MPA; therefore, for SPA or MPA patients who have undergone lobe resection or VATS, systematic lymph node dissection should be considered.
The prognosis of lung cancer patients (particularly those with adenocarcinoma) may differ even after receiving the same treatment, suggesting that many intrinsic biological characteristics of these tumors may also have prognostic significance. The histological heterogeneity of different subtypes is characteristic for lung adenocarcinoma. Morphological heterogeneity may exist among different lung adenocarcinomas and even within the same type, and different histological subtypes of lung adenocarcinoma also have different response to treatment (26-28). In our current study, the LPA was predominantly seen in female patients. Interestingly, women are also more likely to develop lung adenocarcinoma with epidermal growth factor receptor (EGFR) mutations, which histologically is seen to be tumors with lepidic growth. Therefore, LPA is the predominant histologic subtype that is suitable for targeted therapies.
Sakurai et al. (29) retrospective analyzed the clinical data of 380 patients with adenocarcinomas sized ≤2 cm; among the 91 patients with tumors sized <0.6 cm, only 3.3% experienced tumor relapse. More importantly, all the patients survived for more than seven years. Martini et al. (30) retrospectively analyzed 498 cases of stage IA non-small cell lung cancer and found that the survival of patients with tumors sized <1 cm was significantly superior to those with tumors sized 1-3 cm. Therefore, tumor size can be a prognostic factor. As shown in our study, LPA had relatively small diameter, whereas the diameters of SPA, APA, and MPA were relatively large, which is consistent with a previous study (5).
Among the 188 cases of invasive lung adenocarcinoma, APA and PPA accounted for 77%, while LPA and MPA only accounted for 11.1%. The proportions of the different subtypes of invasive lung adenocarcinoma in our study are basically similar to the results of the other 16 articles (6-21). Our current study was also limited by its retrospective design, and no detection result of the EGFR gene mutation lung in tissue was available. An ongoing follow-up study among these patients will provide more evidences.
In summary, the histological subtypes of lung adenocarcinoma have their unique clinicopathological features. Strict subtyping of the lung adenocarcinoma based on the new international classification criteria is of great clinical importance.
Acknowledgements
The study was supported by a grant from “Twelve-Five Plan”, the Major Program of Nanjing Medical Science and Technique Development Foundation (Molecular Mechanism Study on Metastasis and Clinical Efficacy Prediction of Non-small Cell Lung Cancer) and Third Level Training Program of Young Talent Project of Nanjing Health, Nanjing Medical Science and Technology Development Project (QRX11226), and Young Professionals Foundation of Nanjing Chest Hospital.
Disclosure: The authors declare no conflict of interest.
References
- Ost D, Fein AM, Feinsilver SH. Clinical practice. The solitary pulmonary nodule. N Engl J Med 2003;348:2535-42. [PubMed]
- Dargan EL. The enigma of the solitary pulmonary nodule. J Natl Med Assoc 1973;65:101-3 passim. [PubMed]
- Gould MK, Ghaus SJ, Olsson JK, et al. Timeliness of care in veterans with non-small cell lung cancer. Chest 2008;133:1167-73. [PubMed]
- Tmvis WD, Brambills E, Noguchi M. J Thoracic Oncol 2011;6:244-85.
- Yoshizawa A, Motoi N, Riely GJ, et al. Impact of proposed IASLC/ATS/ERS classification of lung adenocarcinoma: prognostic subgroups and implications for further revision of staging based on analysis of 514 stage I cases. Mod Pathol 2011;24:653-64. [PubMed]
- Ding FG, Liu B, Zhang XH, et al. Prognostic significance of a newly proposed grading and scoring system in stage I pulmonary adenocarcinoma. Zhonghua Bing Li Xue Za Zhi 2012;41:145-50. [PubMed]
- Xu L, Tavora F, Burke A. Histologic features associated with metastatic potential in invasive adenocarcinomas of the lung. Am J Surg Pathol 2013;37:1100-8. [PubMed]
- Hung JJ, Jeng WJ, Chou TY, et al. Prognostic value of the new International Association for the Study of Lung Cancer/American Thoracic Society/European Respiratory Society lung adenocarcinoma classification on death and recurrence in completely resected stage I lung adenocarcinoma. Ann Surg 2013;258:1079-86. [PubMed]
- Kadota K, Colovos C, Suzuki K, et al. FDG-PET SUVmax combined with IASLC/ATS/ERS histologic classification improves the prognostic stratification of patients with stage I lung adenocarcinoma. Ann Surg Oncol 2012;19:3598-605. [PubMed]
- Song Z, Zhu H, Guo Z, et al. Prognostic value of the IASLC/ATS/ERS classification in stage I lung adenocarcinoma patients--based on a hospital study in China. Eur J Surg Oncol 2013;39:1262-8. [PubMed]
- Warth A, Muley T, Meister M, et al. The novel histologic International Association for the Study of Lung Cancer/American Thoracic Society/European Respiratory Society classification system of lung adenocarcinoma is a stage-independent predictor of survival. J Clin Oncol 2012;30:1438-46. [PubMed]
- Russell PA, Wainer Z, Wright GM, et al. Does lung adenocarcinoma subtype predict patient survival?: a clinicopathologic study based on the new International Association for the Study of Lung Cancer/American Thoracic Society/European Respiratory Society international multidisciplinary lung adenocarcinoma classification. J Thorac Oncol 2011;6:1496-504. [PubMed]
- Woo T, Okudela K, Mitsui H, et al. Prognostic value of the IASLC/ATS/ERS classification of lung adenocarcinoma in stage I disease of Japanese cases. Pathol Int 2012;62:785-91. [PubMed]
- Yoshizawa A, Sumiyoshi S, Sonobe M, et al. Validation of the IASLC/ATS/ERS lung adenocarcinoma classification for prognosis and association with EGFR and KRAS gene mutations: analysis of 440 Japanese patients. J Thorac Oncol 2013;8:52-61. [PubMed]
- Russell PA, Barnett SA, Walkiewicz M, et al. Correlation of mutation status and survival with predominant histologic subtype according to the new IASLC/ATS/ERS lung adenocarcinoma classification in stage III (N2) patients. J Thorac Oncol 2013;8:461-8. [PubMed]
- Yanagawa N, Shiono S, Abiko M, et al. New IASLC/ATS/ERS classification and invasive tumor size are predictive of disease recurrence in stage I lung adenocarcinoma. J Thorac Oncol 2013;8:612-8. [PubMed]
- Zhang J, Wu J, Tan Q, et al. Why do pathological stage IA lung adenocarcinomas vary from prognosis?: a clinicopathologic study of 176 patients with pathological stage IA lung adenocarcinoma based on the IASLC/ATS/ERS classification. J Thorac Oncol 2013;8:1196-202. [PubMed]
- Gu J, Lu C, Guo J, et al. Prognostic significance of the IASLC/ATS/ERS classification in Chinese patients-A single institution retrospective study of 292 lung adenocarcinoma. J Surg Oncol 2013;107:474-80. [PubMed]
- Tsuta K, Kawago M, Inoue E, et al. The utility of the proposed IASLC/ATS/ERS lung adenocarcinoma subtypes for disease prognosis and correlation of driver gene alterations. Lung Cancer 2013;81:371-6. [PubMed]
- Kadota K, Yeh YC, Sima CS, et al. The cribriform pattern identifies a subset of acinar predominant tumors with poor prognosis in patients with stage I lung adenocarcinoma: a conceptual proposal to classify cribriform predominant tumors as a distinct histologic subtype. Mod Pathol 2013. [Epub ahead of print]. [PubMed]
- von der Thüsen JH, Tham YS, Pattenden H, et al. Prognostic significance of predominant histologic pattern and nuclear grade in resected adenocarcinoma of the lung: potential parameters for a grading system. J Thorac Oncol 2013;8:37-44. [PubMed]
- Comstock GW, Vaughan RH, Montgomery G. Outcome of solitary pulmonary nodules discovered in an x-ray screening program. N Engl J Med 1956;254:1018-22. [PubMed]
- Xu Y, Zhou XJ, Dong YC, et al. Prognostic significance and grading of stromal invasion in pT1 adenocarcinoma of lung. Zhonghua Bing Li Xue Za Zhi 2009;38:451-5. [PubMed]
- Amin MB, McKenney JK. An approach to the diagnosis of flat intraepithelial lesions of the urinary bladder using the World Health Organization/International Society of Urological Pathology consensus classification system. Adv Anat Pathol 2002;9:222-32. [PubMed]
- Yim J, Zhu LC, Chiriboga L, et al. Histologic features are important prognostic indicators in early stages lung adenocarcinomas. Mod Pathol 2007;20:233-41. [PubMed]
- Borczuk AC, Qian F, Kazeros A, et al. Invasive size is an independent predictor of survival in pulmonary adenocarcinoma. Am J Surg Pathol 2009;33:462-9. [PubMed]
- Sakurai H, Maeshima A, Watanabe S, et al. Grade of stromal invasion in small adenocarcinoma of the lung: histopathological minimal invasion and prognosis. Am J Surg Pathol 2004;28:198-206. [PubMed]
- Barletta JA, Yeap BY, Chirieac LR. Prognostic significance of grading in lung adenocarcinoma. Cancer 2010;116:659-69. [PubMed]
- Sakurai H, Maeshima A, Watanabe S, et al. Grade of stromal invasion in small adenocarcinoma of the lung: histopathological minimal invasion and prognosis. Am J Surg Pathol 2004;28:198-206. [PubMed]
- Martini N, Bains MS, Burt ME, et al. Incidence of local recurrence and second primary tumors in resected stage I lung cancer. J Thorac Cardiovasc Surg 1995;109:120-9. [PubMed]


