Enhanced recovery after thoracic surgery reduces discharge on highly dependent narcotics
Introduction
There is a large prescription drug epidemic in the United States. About 54 million people have used prescription narcotics for nonmedical reasons in their life time (1). Some of these people were first introduced to highly dependent narcotics after a surgical procedure (2). Moreover, many patients are overprescribed highly addictive pain medication after surgery (3), which contributes to the epidemic. The Drug Enforcement Agency (DEA) classifies narcotics based on their abuse or dependency potential (4). Schedule I is a class of narcotics that is too addictive to be used for medical purposes, such as heroin or cocaine. Schedule II drugs are highly addictive narcotics that can be used for medical purposes. Norco (hydrocodone/acetaminophen) is an often-prescribed drug in this class. Schedule III drugs are narcotics that have less potential for abuse than schedules I and II and includes Tylenol #3 (acetaminophen with codeine). Schedule IV is a less addictive class of narcotics such as Tramadol, a synthetic narcotic. Although all narcotics can be abused, schedule II narcotics are particularly concerning due to their addictive properties.
General thoracic surgery specializes in the treatment of patients with diseases of the chest and upper abdomen. Lung resection requires incisions in the chest cavity with surgery often taking place between the rib spaces. This is often a very painful operation since each rib has an intercostal nerve that often gets compressed during the operation. Moreover, the presence of a chest tube after the surgery causes notable pain. Foregut surgery, although typically performed with minimally invasive incisions, does have a degree of pain requiring narcotic pain medication. Enhanced recovery protocols have only recently been developed in thoracic surgery, but have been shown to reduce length of stay and postoperative complications. We have implemented our protocol in stages, beginning with a preoperative education program, then adding a multilevel intercostal nerve block intraoperatively with a non-narcotic-based pain medication regimen as the primary source of postoperative pain control. Finally, we added an intraoperative protocol including the use of total intravenous anesthesia (TIVA) during the surgery, multimodal analgesia with minimal opioids, PONV prophylaxis and maintenance of euvolemia. We applied the protocol across all cases.
Prior to starting any components of enhanced recovery after thoracic surgery (ERATS) program in our institution, both groups of patients went home with a prescription of schedule II medication for post-operative pain control. ERATS have shown to decrease morbidity (5,6) and hospital length of stay (7). However, there has not been a great focus on the type of narcotics with which patients are discharged home after an enhanced recovery as part of the surgery protocol. We want to determine if an enhanced recovery protocol can decrease the number of patients who go home with schedule II narcotics medications.
Methods
The Institutional Review Board at Houston Methodist Research Institute approved this study (IRB# Pro00013680). Patients who were undergoing either lung surgery or foregut surgery were put on the ERATS protocol (Table 1). We analyzed the patients who underwent the protocol in 8-month time period since the full implementation of the program. We excluded patients who underwent urgent or emergent operation. There were three phases in ERATS protocol (Table 1). During the office visit, patients were told about the ERATS protocol and the goal of decreasing the use of narcotics during the operative experience. Patients were also instructed to walk 1 mile a day prior to surgery to prepare for the operation. Patients were given an incentive spirometer to practice at home. If the patient was an active smoker, he or she was counseled to stop smoking, and if the patient had heavy alcohol use, he or she was asked to stop drinking 2 weeks prior to surgery.
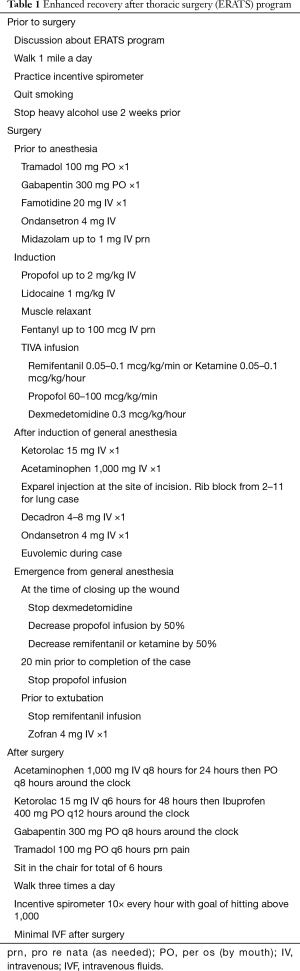
Full table
About 1 hour prior to surgery, unless allergic, patients were given PO tramadol and gabapentin. Approximately 5–10 minutes prior to induction patients were administered up to 1 mg midazolam IV, famotidine 20 mg, and ondansetron 4 mg IV. At induction, up to 2 mg/kg propofol was titrated IV along with up to 100 mg of lidocaine and a muscle relaxant of choice. Patients also received up to 100 mcg fentanyl IV. TIVA infusions were started with induction, maintained and titrated throughout the case to a bispectral index (BIS) of 40–60. Infusions included propofol 60–100 mcg/kg/min, remifentanil 0.05–0.1 mcg/kg/min or ketamine 0.05–0.1 mcg/kg/hour and dexmedetomidine 0.3 mcg/kg/hour. Generally propofol at 100 mcg/kg/min and remifentanil at 0.075 mcg/kg/min were the starting infusion doses. Patients were intubated with the appropriate size single or double lumen endotracheal tube.
Prior to incision, patients were administered 1 g of IV Acetaminophen and 4–8 mg of dexamethasone. Patients with creatinine ≤1 and age <75 years old (after confirming with surgeon) were administered ketorolac 15 mg IV. Patients received ondansetron 4mg IV (repeated dose) prior to extubation. All patients received Exparel (bupivacaine liposome injectable suspension), administered at the sites of incision. For those patients who underwent lung resection, the patient underwent an intercostal nerve block with Exparel from the 2nd intercostal space to the 11th intercostal space. Patients received TIVA during the surgery. Patients received minimal narcotics, minimal benzodiazepines and were kept euvolemic during the operation. We employ a strategy of goal directed fluid therapy with monitoring through measuring stroke volume variation, pulse pressure variation and cardiac index.
When trocars were removed or approximately 30 minutes prior to extubation, dexmedetomidine was stopped. About 20 minutes prior to extubation, remifentanil/ketamine and propofol infusions were decreased by half. Propofol was stopped 10 minutes prior to extubation and remifentanil was stopped immediately before extubation. Patients were extubated when extubation criteria were met.
After the operation, the patients were given IV acetaminophen 1 g q8 for 24 hours and switched to PO acetaminophen around the clock. The patients were given ketorolac 15 mg q6 hours for 48 hours then ibuprofen around the clock. The patients received gabapentin 300 mg q12 hours around the clock. Finally, patients were given tramadol as needed. If patients had pain despite this regimen, patients were given IV dilaudid 0.5 mg every 1 hour ×2 doses. If the pain was persistent, patients were given IV dilaudid PCA. In addition to this pain regimen, patients were asked to walk three times a day after the surgery, work on IS 10 times every hour while awake with the goal of hitting >1,000 mL and sit in the chair for >6 hours a day. We adjusted the pain medication if patients were unable to perform these tasks. Patients who had a lung resection were given a regular diet after the surgery and received minimal IVF after surgery. Patients who had foregut surgery were kept NPO overnight and their diet was advanced the next morning.
All outcomes were obtained from the prospective database for the Society of Thoracic Surgeons at Houston Methodist Hospital, which is extracted from the electronic health record. We then performed a retrospective analysis to determine the prescription the patient received when they were discharged after surgery. We obtained information on whether patients were on narcotics prior to surgery from the electronic health record. We analyzed categorical variables and determined the percentage of patients in each category. We analyzed the patients’ age with mean and standard deviation. We analyzed the length of stay using median and range. We determined the number of patients with complications and recorded each complication from Grade I to Grade V based on the Clavien-Dindo classification of surgical complication (8,9). Patients with multiple complications were assigned the highest grade of complication.
Results
There were 52 patients who underwent lung resection. The average age of this group was 65 years old and they were predominantly female (65%). The common co-morbidities were hypertension (56%), COPD (25%), CAD (19%) and diabetes (19%). Most patients were former smokers (60%). All of the patients underwent a minimally invasive procedure with most of the patients undergoing robot-assisted lung resection (69%). The most common procedures were lobectomy (44%) and wedge resection (35%). In the foregut group, there were 54 patients. The average age of the group was 56 years old and they were mostly female (59%). The most common co-morbidity was hypertension (54%). Most of the patients were nonsmokers (76%). All of the patients underwent a minimally invasive procedure with most of the patients undergoing robot-assisted surgery (87%). The most common procedure was hiatal hernia repair with fundoplication (Table 2).

Full table
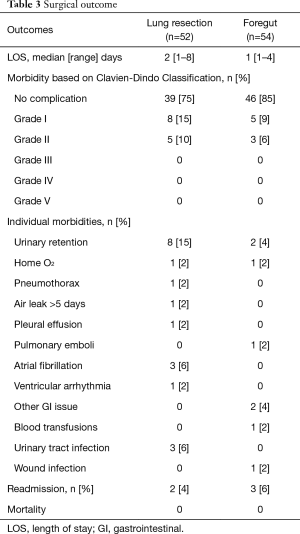
The median length of stay for lung resection was 2 days while it was 1 day after foregut surgery. Most patients had no complication with 75% in the lung resection group and 85% in the foregut group. Most of the patients who had a complication after lung resection had a grade I complication (15%) such as urinary retention, pneumothorax after chest tube removal and discharge home with O2. Ten percent of the patients after lung resection had a grade II complication such as atrial fibrillation, UTI and a wound infection treated with medication. No patients had grade III, IV or V complications after lung surgery. After foregut surgery, 9% of the patients had a grade I complication such as urinary retention and discharge home on O2 and 6% had a grade II complication such as postoperative transfusion and pulmonary emboli treated with medication. The readmission rate after lung resection was 4% and 6% after foregut surgery. There was no mortality in either group (Table 3).
Full table
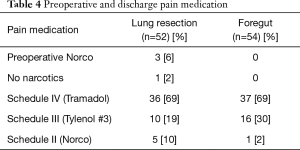
No patients in the foregut group and 6% of patients in the lung resection group were on narcotic medication prior to surgery. After the surgery, 69% of the patients in the lung resection group and 69% of the foregut group went home on schedule IV narcotics pain medication. Only 10% in the lung resection group and 2% in the foregut group went home on schedule II narcotics pain medication. All patients who were on schedule II narcotics pain medication prior to surgery went home on schedule II narcotics pain medication (Table 4).
Full table
Discussion
Early recovery in thoracic surgery protocols has shown pain reduction for patients, decrease in complication rate and total length of stay (10,11). We also found similar outcomes in our study. We had no mortality, a very low complication rate and a very short length of stay after surgery. This is very favorable outcome in the background of the expected outcomes from similar operations. In addition, we were able to demonstrate a decrease in the number of patients who are discharged home with highly dependent narcotics. In our experience, 100% of our patients were discharged home with highly dependent narcotics with both types of operation prior to starting the program. We implemented the program in stages where we first focused on the preoperative component then postoperative component and finally an operative component. A key factor that contributed to success of the program is a multidisciplinary team approach, which included including thoracic surgery, thoracic surgery staff, cardiovascular (CV) anesthesia, intensivist, nursing, pharmacy and house staff to develop and implement the program.
Overall preparing the patient for surgery is an important aspect of the protocol. The preoperative discussion involves active participation by the patients in their own recovery. Although it is hard to quantitate, having motivated patients getting ready for surgery and being actively involved with their recovery makes it easier to take care of them in the post-operative period. We focus on three areas in the preoperative setting. First, we discuss the factors that can be modified prior to surgery to improve surgical recovery. These include smoking cessation, stopping alcohol consumption and stopping any medication that can be safely stopped that can increase complication such as blood thinners and steroids. Second, we discuss things the patients can do to improve their recovery. Two things that we stress in this category are walking 1 mile a day and learning how to use the incentive spirometer. The last category is discussing with patients what to expect regarding pain control after surgery. We found that this significantly improves the patient’s preparation for surgery and encourages them to take responsibility for their recovery. Studies have shown that an exercise program prior to surgery can improve function after surgery (12,13). This has helped patients to recover faster with fewer complications.
In the perioperative period, we have always used minimally invasive techniques to improve outcomes but the addition of pre-emptive pain control and minimizing narcotics has made a major impact in post-surgical use of highly addictive narcotics. The use of scheduled acetaminophen, ketorolac and gabapentin as well as Exparel for nerve block has significantly decreased the use of highly addictive narcotics at the time of discharge. Exparel, especially in the lung resection, makes a significant impact with blocking the nerve that causes pain in the chest cavity (14). Most patients do not have pain after the nerve block and just notice the chest tube. All of these patients have decreased pain after the removal of the chest tube.
One group that we are unable to discharge home with less addictive narcotics includes patients who are already taking highly addictive schedule II narcotics prior to surgery due to pre-existing pain. Less addictive narcotics in these groups did not work and we would have to quickly transition to narcotic PCA and back to home regimen. Studies have shown that patients who are on narcotics prior to surgery were more likely to have a longer hospital stay, discharge to rehabilitation facility and higher readmission (15). We did not have enough patients to analyze determine if this is the case in our group but our overall experience is that it is more difficult to manage the post-operative pain in patients who were on narcotics pain medication prior to surgery.
One limitation of this study is that it is unknown how much of the prescribed pain medication the patients took at home. Most of the patients would comment at their follow up appointment that they only took narcotics pain medication for one or two days and transitioned to non-narcotics pain medication such as acetaminophen or ibuprofen. Thus, the benefits of this protocol may be greater than it has been observed in this study. Another limitation of this study is it is unknown which aspect of the protocol had the greatest contribution to the outcome. We decided to take the best evidence in the literature to create this program thus it is unknown the incremental benefit from each of the components.
Conclusions
The implementation of ERATS program for our thoracic surgery patients has significantly decreased the availability of highly addictive narcotics in the community and has decreased the possibility of our patients to abuse these drugs, while ensuring that we still provide adequate pain relief following surgery. We can do our part in reducing the prescription drug epidemic that is prevalent in the United States.
Acknowledgements
We thank Anna Saikin for language editing the manuscript. We thank Kathryn J. Schulze and Debra Selig-Rosen for providing the data collected for the Society of Thoracic Surgery at Houston Methodist Hospital.
Footnote
Conflicts of Interest: MP Kim and EY Chan consult for Boston Scientific, Medtronic and Olympus. FN Masud is a consultant for Mallinkrodt and Chiesi. LM Meisenbach and R Dumitru have no conflicts of interest to declare. JK Brown’s husband consults and on advisory board for Pacira Pharmaceuticals, ConMed and Edward Life Science.
Ethical Statement: The Institutional Review Board at Houston Methodist Research Institute approved this study (IRB# Pro00013680).
References
- Substance Abuse and Mental Health Services Administration. Results from the 2014 National Survey on Drug Use and Health: Detailed Tables. 2015. Available online: http://www.samhsa.gov/data/sites/default/files/NSDUH-DetTabs2014/NSDUH-DetTabs2014.pdf, accessed 7/20/2017.
- Brummett CM, Waljee JF, Goesling J, et al. New Persistent Opioid Use After Minor and Major Surgical Procedures in US Adults. JAMA Surg 2017;152:e170504. [Crossref] [PubMed]
- Bates C, Laciak R, Southwick A, et al. Overprescription of postoperative narcotics: a look at postoperative pain medication delivery, consumption and disposal in urological practice. J Urol 2011;185:551-5. [Crossref] [PubMed]
- Controlled Substance Schedules. U.S. Department of Justice, Drug Enforcement Administration. 2017. Available online: https://www.deadiversion.usdoj.gov/schedules/index.html
- Muehling BM, Halter GL, Schelzig H, et al. Reduction of postoperative pulmonary complications after lung surgery using a fast track clinical pathway. Eur J Cardiothorac Surg 2008;34:174-80. [Crossref] [PubMed]
- Jones NL, Edmonds L, Ghosh S, et al. A review of enhanced recovery for thoracic anaesthesia and surgery. Anaesthesia 2013;68:179-89. [Crossref] [PubMed]
- Preventza O, Hui HZ, Hramiec J. Fast track video-assisted thoracic surgery. Am Surg 2002;68:309-11. [PubMed]
- Clavien PA, Barkun J, de Oliveira ML, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg 2009;250:187-96. [Crossref] [PubMed]
- Katayama H, Kurokawa Y, Nakamura K, et al. Extended Clavien-Dindo classification of surgical complications: Japan Clinical Oncology Group postoperative complications criteria. Surg Today 2016;46:668-85. [Crossref] [PubMed]
- Das-Neves-Pereira JC, Bagan P, Coimbra-Israel AP, et al. Fast-track rehabilitation for lung cancer lobectomy: a five-year experience. Eur J Cardiothorac Surg 2009;36:383-91; discussion 391-2. [Crossref] [PubMed]
- Gimenez-Mila M, Klein AA, Martinez G. Design and implementation of an enhanced recovery program in thoracic surgery. J Thorac Dis 2016;8:S37-45. [PubMed]
- Carli F, Gillis C, Scheede-Bergdahl C. Promoting a culture of prehabilitation for the surgical cancer patient. Acta Oncol 2017;56:128-33. [Crossref] [PubMed]
- Carli F, Zavorsky GS. Optimizing functional exercise capacity in the elderly surgical population. Curr Opin Clin Nutr Metab Care 2005;8:23-32. [Crossref] [PubMed]
- Khalil KG, Boutrous ML, Irani AD, et al. Operative Intercostal Nerve Blocks With Long-Acting Bupivacaine Liposome for Pain Control After Thoracotomy. Ann Thorac Surg 2015;100:2013-8. [Crossref] [PubMed]
- Waljee JF, Cron DC, Steiger RM, et al. Effect of Preoperative Opioid Exposure on Healthcare Utilization and Expenditures Following Elective Abdominal Surgery. Ann Surg 2017;265:715-21. [Crossref] [PubMed]


