Feasible and promising modified trans-subxiphoid thoracoscopic extended thymectomy for patients with myasthenia gravis
Introduction
Surgery is one of the most important treatments for patients with myasthenia gravis (MG) (1-3). The goal of surgery in these patients is to safely remove as much thymic tissue and mediastinal fat as possible. Sternotomy has long been considered an essential approach for extended thymectomy (4-7). However, there is no consensus as to whether sternotomy is better than less invasive techniques recently reported in terms of efficacy in MG (8,9).
Among many minimally invasive procedures, such as video-assisted thoracic surgery (VATS) and a robot-assisted thoracic surgery (RATS), we believe that the single-port trans-subxiphoid thoracoscopic approach is ideal and superior to other approaches in terms of not only less intercostal neuralgia, better cosmetic results, faster recovery, and lower cost, but also better operative views of the bilateral phrenic nerves and the upper area of the innominate vein (10,11). However, a single-port procedure does not allow easy manipulation, and much time is needed to master it.
Here, we report a promising procedure, a modified single-port trans-subxiphoid approach (MTXA) that improves the maneuverability of the single-port approach by adding a 5-mm port on the right side of the chest. Furthermore, we compared the clinical outcomes of extended thymectomy via our approach to those of extended thymectomy via sternotomy in terms of less invasiveness and effectiveness for MG.
Methods
This retrospective cohort study was approved by the Kitasato University Medical Ethics Committee (B16-233). All patients who underwent extended thymectomy for MG at our institution between January 1, 2010 and December 31, 2016 were identified from the database of the Thoracic Surgery Department. We excluded patients with Masaoka stage III–IV thymoma and/or thymomas greater than 5 cm because our modified trans-subxiphoid approach is only applicable to patients with MG and/or thymoma that is up to 5 cm in diameter and have no infiltration into the surrounding tissues. Subsequently, we divided the remaining patients into two groups, the MTXA group and the Sternotomy group, and compared the factors listed below.
The patients’ medical records were reviewed for age, sex, comorbidities, perioperative laboratory data, surgical procedures, history and symptoms of MG, and therapies for MG. The Myasthenia Gravis Foundation of America (MGFA) clinical classification, which is determined based on the worst condition of each patient, was used as one of the indicators of preoperative patient condition (12). The Quantitative Myasthenia Gravis (QMG) score and Myasthenia Gravis Activities of Daily Living (MG-ADL) scale were used to evaluate the severity of MG (12,13). To evaluate the effect of the two techniques on MG, we compared the preoperative QMG score, MG-ADL scale, serum level of AChR-Ab (acetylcholine receptor antibody), and dose of prednisone with the values at 3 months postoperatively because the neurologists in our institutions consider the condition of MG at 3 months after surgery to be one of the indicators of therapeutic effect on MG. The majority of the neurologists make it a goal to reduce the amount of prednisone to 5 mg or less per day within 1 year. Therefore, they basically reduce the dose of prednisone as early as possible after surgery, when the MG symptoms are in pharmacologic remission or show minimal manifestation. Oral immunosuppressive agents (cyclosporine or tacrolimus) are sometimes used in combination with prednisone basically to maintain a lower dose of prednisone.
Descriptive statistics for categorical variables are reported as frequency and percentage, and continuous variables are reported as mean (SD) or median (range) as appropriate. The variables in the MTXA and Sternotomy groups were compared using a Fisher exact test or Pearson’s chi-square test for categorical variables and t-test or Mann-Whitney U test for continuous variables. A P value of <0.05 was considered significant. All analyses were conducted with JMP version 11.0 (SAS Inc., Cary, NC, USA) and EZR [(Saitama Medical Center, Jichi Medical University; http://www.jichi.ac.jp/saitama-sct/SaitamaHP.files/statmed.html; Kanda), a graphical user interface for R (The R Foundation for Statistical Computing, Vienna, Austria, Ver. 2. 13.0) and a modified version of R commander (Ver. 1.8-4)].
Surgical technique
MTXA is performed with general anesthesia, which usually does not require differential lung ventilation. Patients are placed in the supine position with legs spread apart. First, the surgeon stands between the patient’s legs while the assistant stands on the right side of the patient to operate the camera. A 2.5-cm longitudinal incision is made below the xiphoid process. Blind blunt dissection with fingers is used to open the retrosternal space. A single port, a GelPOINT Mini (Applied Medical, Rancho Santa Margarita, CA, USA), is inserted into the incision through which carbon dioxide gas (CO2) is insufflated at a pressure of 8–10 mmHg. A long rigid endoscope of 50 cm in length, with a diameter of 5 mm and angle of 30 degrees (Stryker Japan KK Inc.) is used because it helps to minimize interference between the forceps in the right hand of the surgeon and the camera head of the assistant inserted from the single subxiphoid port. The surgeon holds a long, 44-cm LigaSureTM Maryland vessel sealing system (Covidien, Mansfield, MA, USA) in his right hand and dissects the retrosternal space toward the head side of patient. The right pleural cavity is entered, and a 5-mm port is placed in the 5th intercostal space on the lateral side of the midclavicular line. Then, the surgeon switches places with the assistant standing to the right side of the patient. Use of the forceps with the left hand through the additional port dramatically improves operability and enables more delicate movements. The left pleura are opened. CO2 insufflation, which pushes the bilateral lungs, innominate vein, and pericardium away, provides a good view of the bilateral phrenic nerves and provides a wider open field at the head side of the innominate vein.
The right epiphrenic fat pads are initially dissected from the diaphragm and pericardium. The right lobes of the thymus and mediastinal fat tissue are dissected off the pericardium with the LigaSureTM Maryland toward the head side while carefully confirming the right phrenic nerve location. The same procedure is done for the left-hand side. Then, we begin to dissect the right superior horn and the surrounding fat tissue. We can get a good view of the right superior horn without dividing the right internal thoracic vein because the forceps with left hand naturally move the right internal thoracic vein aside during the procedure (Figure 1). Furthermore, using the forceps and the LigaSureTM Maryland through the additional port makes it possible for us to dissect thymic tissue off the inferior pole of thyroid at an ideal angle (Figure 1). In this step, it is very important to apply gentle and deliberate traction on the thymic tissue inferiorly with the long forceps in the right hand from the single port. To identify the left superior horn of the thymus with certainty and divide it safely, an approach from the right alone is not enough. Checking the superior edge of the innominate vein from the left approach is also important. Thymic veins and some of the inferior thyroid veins are sealed by the LigaSureTM. The specimen is removed in a plastic bag through the subxiphoid incision. A 20F chest tube is then inserted into the mediastinum.

Results
Patient characteristics
During the study period, 50 consecutive patients underwent extended thymectomy for MG. Excluded were 11 patients with advanced-stage thymoma (Masaoka stage III or IV), 4 patients with a thymoma of greater than 5 cm, and 2 patients with inadequate information on follow-up. Finally, 13 patients in the MTXA group and 20 patients in the Sternotomy group remained and were analyzed in this study.
Patient characteristics are shown in Table 1. There did not appear to be any significant differences between the two groups in regard to age, sex, BMI, MGFA classification, preoperative QMG score, preoperative MG-ADL scale and preoperative AChR-Ab level. In terms of the variable of thymoma, there were only three patients with thymoma in the MTXA group. The breakdowns of thymoma and thymus pathology are also shown in Table 1.
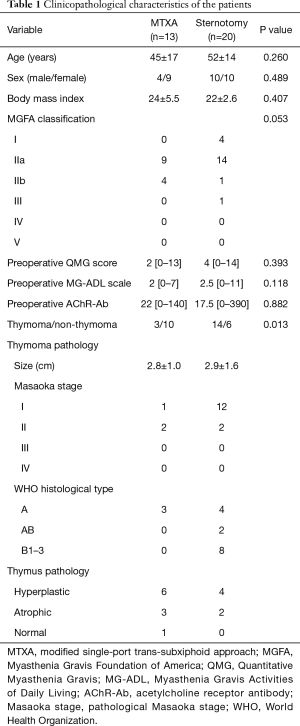
Full table
The perioperative variables including postoperative morbidity between the MTXA group and Sternotomy group are summarized in Table 2. Although the operative time was longer in the MTXA group, intraoperative blood loss, postoperative length of stay, and the value of C-reactive protein (CRP) on postoperative day 1 were significantly more favorable in the MTXA group than in the Sternotomy group. Four patients experienced postoperative crisis in the Sternotomy group, and one patient had left phrenic palsy in the MTXA group.
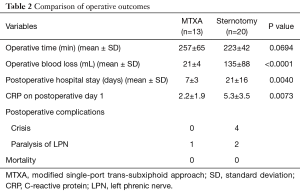
Full table
The variables related to MG status are reported in Table 3. Improvement or no change of symptoms was observed in all patients. The frequency of patients with a decrease in the serum level of AChR-Ab and that of patients with a dose reduction of prednisone was not significantly different between the two groups.

Full table
Discussion
Our approach was devised to improve the operability of the single-port subxiphoid approach, which was reported by Suda et al. (10,11). The simple addition of a single 5-mm port in the right intercostal space allowed us to perform more delicate and safer movements. As a result, we are certain that with our VATS procedure, it is now possible to remove equal or greater amounts of mediastinal and cervical adipose tissue than with the trans-sternal procedure.
Although presently there are, of course, no convincing data that our approach is superior, we believe as strongly as some surgeons do who use variations of the trans-subxiphoid approach (15-17) that our approach has several advantages compared to other minimally invasive approaches. In comparing our approach with the lateral VATS approach, we can obtain a better view of the bilateral phrenic nerves and the upper area of the innominate vein, and there is less intercostal neuralgia. CO2 insufflation and the midline camera make it possible to clearly observe the entire length of the bilateral phrenic nerves and to observe the left thymic horn carefully from both sides, which are essential to a safe operation. Recently, we performed our approach on patients weighing over 100 kg and could obtain our usual good views. This indicates that obesity might not affect the mediastinal view as much as we might have imagined.
Compared to RATS, our approach is superior in terms of cost, the sense of touch, and, possibly, less intercostal neuralgia. The sense of touch is of the greatest importance when judging whether the thymoma is invading surrounding tissue, especially, the pericardium or the innominate vein.
However, the disadvantages of our approach are the necessity of a long scope and long forceps, and the procedure is more difficult than the lateral VATS approach due to the interference between the instruments controlled by the operator’s right hand and the camera inserted in the same single port. As well, there can be some complications associated with CO2 insufflation. For example, when bleeding occurs from the innominate vein, the possibility of air embolism might increase. Furthermore, if a large tumor is located at the head side area of the innominate vein, which is very small space, it is difficult to operate safely enough only with our procedure.
In this study, we examined whether our VATS procedure is superior to sternotomy in terms of invasiveness and efficacy for MG. In regard to invasiveness as reported by others (18,19), our data also showed this approach to be less invasive than sternotomy in terms of blood loss, postoperative length of stay, and the CRP value on postoperative day 1. Some reasons for the lower amount of bleeding include the delicate movements used to avoid hemorrhage that are peculiar to the VATS procedure, the pressure of CO2 insufflation on the small vessels, and no sternal splitting. The faster recovery, which is indicated by the shorter postoperative length of stay and lower CRP value on postoperative day 1 in the MTXA group, show just how great the stress of a splitting the sternum is to patients. Although the operative time was longer in the MTXA group, we think this depends largely on the learning curve. We think that the reason for the difference in the frequency of postoperative crisis was caused not by differences in the procedures but by the poorer preoperative condition of the patients with MG in the Sternotomy group. The differences in the preoperative QMG score and MG-ADL scale between the two groups in Table 1 might support this hypothesis. This bias may work a little more favorably for the MTXA group.
The efficacy of minimally invasive surgery for MG remains controversial. However, some reports show that in terms of remission rates, minimally invasive surgery is equally or more efficacious in MG than the trans-sternal approach (18,19). Our data indicated that importantly, the efficacy of extended thymectomy using our approach is at least not inferior to that of extended thymectomy via sternotomy (Table 3). Although we will have to follow our patients over the long term to more accurately evaluate the effectiveness of our MTXA for MG, it seems that our approach can be a viable replacement for median sternotomy for MG.
Limitations in our study include all of the biases typically caused by a retrospective design and small sample size. Furthermore, we could not show long-term results for MG. In addition, propensity score analysis was not performed due to the small sample size, and we did not measure pain scores although the patients in the MXTA group experienced little intercostal neuralgia. Nevertheless, this approach has great potential to be established as a more minimally invasive procedure that does not cut the mediastinal pleura and as a more aggressive procedure that requires resection of the pericardium, lungs, and brachiocephalic vein.
In summary, the addition of a 5-mm port on the right side of the chest has made it possible for us to operate more easily, more safely, and more delicately than ever while maintaining the advantages of single-port thymectomy from the subxiphoid approach. The VATS extended thymectomy by our approach might be considered as one of the standard procedures for patients with MG unless the superiority of sternotomy in terms of its effectiveness for MG can be proved in the future.
Acknowledgements
We thank all of the members of the Department of Thoracic Surgery and Department of Neurology of Kitasato University School of Medicine for helping in the management of this study.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This retrospective cohort study was approved by the Kitasato University Medical Ethics Committee (B16-233).
References
- Wolfe GI, Kaminski HJ, Aban IB, et al. Randomized trial of thymectomy in myasthenia gravis. N Engl J Med 2016;375:511-22. [Crossref] [PubMed]
- Taioli E, Paschal PK, Liu B, et al. Comparison of conservative treatment and thymectomy on myasthenia gravis outcome. Ann Thorac Surg 2016;102:1805-13. [Crossref] [PubMed]
- Barnett C, Katzberg HD, Keshavjee S, et al. Thymectomy for non-thymomatous myasthenia gravis: a propensity score matched study. Orphanet J Rare Dis 2014;9:214. [Crossref] [PubMed]
- Jaretzki A 3rd, Aarli JA, Kaminski HJ, et al. Thymectomy for myasthenia gravis: evaluation requires controlled prospective studies. Ann Thorac Surg 2003;76:1-3. [Crossref] [PubMed]
- Jaretzki A 3rd, Wolff M. "Maximal" thymectomy for myasthenia gravis. Surgical anatomy and operative technique. J Thorac Cardiovasc Surg 1988;96:711-6. [PubMed]
- Masaoka A. Extended trans-sternal thymectomy for myasthenia gravis. Chest Surg Clin N Am 2001;11:369-87. [PubMed]
- Masaoka A, Monden Y. Comparison of the results of transsternal simple, transcervical simple, and extended thymectomy. Ann N Y Acad Sci 1981;377:755-65. [Crossref] [PubMed]
- Sonett JR, Jaretzki A 3rd. Thymectomy for nonthymomatous myasthenia gravis: a critical analysis. Ann N Y Acad Sci 2008;1132:315-28. [Crossref] [PubMed]
- Orsini B, Santelmo N, Pages PB, et al. Comparative study for surgical management of thymectomy for non-thymomatous myasthenia gravis from the French national database EPITHOR. Eur J Cardiothorac Surg 2016;50:418-22. [Crossref] [PubMed]
- Suda T. Single-port thymectomy using subxiphoid approach-surgical technique. Ann Cardiothorac Surg 2016;5:56-8. [PubMed]
- Suda T, Kaneda S, Hachimaru A, et al. Thymectomy via a subxiphoid approach: single-port and robot-assisted. J Thorac Dis 2016;8:S265-71. [PubMed]
- Jaretzki A 3rd, Barohn RJ, Ernstoff RM, et al. Myasthenia gravis: recommendations for clinical research standards. Task Force of the Medical Scientific Advisory Board of the Myasthenia Gravis Foundation of America. Ann Thorac Surg 2000;70:327-34. [Crossref] [PubMed]
- Wolfe GI, Herbelin L, Nations SP, et al. Myasthenia gravis activities of daily living profile. Neurology 1999;52:1487-9. [Crossref] [PubMed]
- Shiomi K, Kitamura E, Ono M, et al. Surgical technique of a modified single-port trans-subxiphoid thoracoscopic extended thymectomy for patients with myasthenia gravis. Asvide 2018;5:377. Available online: http://www.asvide.com/article/view/23847
- Tang Y, Ou ZA, Liao M, et al. Subcostal thoracoscopic extended thymectomy for patients with myasthenia gravis. J Thorac Dis 2016;8:499-504. [Crossref] [PubMed]
- Zhao J, Wang J, Zhao Z, et al. Subxiphoid and subcostal arch thoracoscopic extended thymectomy: a safe and feasible minimally invasive procedure for selective stage III thymomas. J Thorac Dis 2016;8:S258-64. [PubMed]
- Zhong Y, Zhou Y, Jiang L, et al. Modified transsubxiphoid thoracoscopic extended thymectomy in patients with myasthenia gravis. Thorac Cardiovasc Surg 2017;65:250-4. [Crossref] [PubMed]
- Gung Y, Zhang H, Li S, et al. Sternotomy versus video-assisted thoracoscopic surgery for thymectomy of myasthenia gravis patients: a meta-analysis. Asian J Endosc Surg 2016;9:285-94. [Crossref] [PubMed]
- Raza A, Woo E. Video-assisted thoracoscopic surgery versus sternotomy in thymectomy for thymoma and myasthenia gravis. Ann Cardiothorac Surg 2016;5:33-7. [PubMed]


