Improved three-tubing approach for the reoperation of perforation suturing anastomotic fistula after radical radiotherapy of upper thoracic esophgeal squamous cell carcinoma
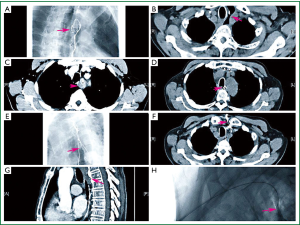
The patient (male, aged 63) was diagnosed as upper and middle thoracic esophageal squamous cell carcinoma (cT3N0M0) (Figure 1A,B) and denied a history of diabetes. The dual-location was carried out with CT and simulator preoperationally, fraction radiotherapy was delivered in 6 MV X-ray LINAC; based on the fluro display of barium meal, the field of irradiation was extended 3-4 cm out of the upper and lower limits of the lesion, with the dose of 68 Gy/34 f/6.8 weeks. Three weeks of radical radiotherapy later, the tumor shank significantly as evaluated according to re-examination with esophagography (Figure 1C). Six months later, the patient suffered severe pain in the thoracic back because of esophageal perforation as the thoracic CT suggested (Figure 1D). Thus the patient had an operation of Ivor-Lewis plus gastroesophageal stapled anastomosis in left neck. Three weeks after operation, symptoms such as fever and cough occurred after taking liquid diet; the esophagography suggested the formation of anastomotic-mediastinal fistula and mediastinal encapsulated abscess (Figure 1E). The patient underwent the treatments such as fasting, gastrointestinal decompression, anti-inflammation and nutritional support. Four weeks after operation, the patient suffered deterioration of irritable cough because of tracheo-mediastinal fistula as CT and fiber bronchoscope suggested (Figures 1F,2). CT and DSA-guided percutaneous cervical gastric wall puncture were performed for the patient while the Flocare nasoenteral tube was introduced entering the mediastinum via the anastomotic fistula under the guidance of contrast medium followed by the procedure of persistent vacuum-suction for 24 hours (Figure 1G,H). Gastrointestinal decompression and nutritional support via jejunum were performed as before. The tube had been replaced for three times during the treatment. Four months later, the patient was discharged after the healing of gastroesophageal anastomotic fistula, significant shrink of tracheo-mediastinal fistula and no discomfort when taking semi-liquid diet. The patient was followed up for six months, there was no recurrence, nor distantmetastasis, and the recovery of diet was satisfactory.
Discussion
Anastomotic fistula complicated following the operation against esophageal carcinoma is one of the commonest severe complications postoperatively, especially for the patient with the medical history of radical radiotherapy. Studies have indicated (1) that pathological changes such as swelling, cytoplasmic vacuole, nuclear degeneration and necrosis in different levels may appear in the carcinoma tissues, paracarcinoma tissues and surrounding normal tissues after radical radiotherapy. Perhaps the condition of the patient is controlled to some extent; however, the incidence of post-operational complications will increase accordingly, among which the anastomotic fistula and pulmonary infection prevail.
In terms of time, the anastomotic fistula complicated following the operation against esophageal carcinoma can be classified as early fistula and middle and advanced fistula. The early fistula is usually associated with the anastomotic technology whereas the middle and advanced fistula is associated with the blood supply of anastomosis. In this case, the occurance of anastomotic-mediastinal fistula when the patient takes liquid diet three weeks after operation, suggests that the condition may be related to difference in blood supply of anastomosis cause by radical radiotherapy and it may break the trachea membrane and form tracheo-mediastinal fistula because of severe adhesion around the anastomosis and resultant encapsulated abscess which is formed in the mediastinum. Since severe trauma and high risk of complication may be caused by the application of conventional surgical dissection, drainage and repair, we applied an improved Three-tubing Therapy (drainage tube, gastric tube and nutrition tube) for the treatment of the patient, with major experiences presented as follows: (I) difference of puncture Site. We observe the fistula and vomica with lipiodol in the interventional condition, and then select the puncture site under the guidance of CT; the guide wire is placed firstly and correctly reaches the position without any adverse effect on the fistula and then Flocare nasoenteral drainage tube is placed (sizing according to the anastomotic fistula). The placed tube is then introduced to the bottom of abscess via the anastomotic fistula for continual drainage after connected to the negative pressure. Compared with the transnasal operation (2), pain and psychological pressure the patient suffered caused by the percutaneous gastric wall puncture and insertion was insignificant; (II) the level of negative pressure is under control. As we all know that high negative pressure may cause adverse suction of gastric juice and low negative pressure may result in poor efficacy. We conclude that the negative pressure should be maintained at approx. 4-6 cm H2O with the vacuum device. Two weeks after tube placement, daily low-pressure washing for the vomica should be performed to clear the thick pus in the lacuna. The content in lacuna can be drained sufficiently, and therefore the encapsulated vomica will shrink rapidly; (III) timing of Tube Withdrawal. The vomica usually becomes sinus tract surrounding tightly the drainage tube after two weeks, however, sinus tract of the patient in this case formed gradually after five weeks. The tube may be withdrawn at the moment while it should be done slowly based on the clinical and radiographic state. The length of tube withdrawal each time is usually less than 5 mm according to the size of vomica. The drainage tube was withdrawn into the thoracostomach in ten days. The extubation was carried out after the patient is allowed to take food gradually and there is no special problem identified after one weeks of observation.
The retention of intraperitoneal gastrojejunostomy tube and gastrointestinal decompression tube is same as the conventional treatment. Perioperational relative low calorie (15-20 kcal/kg.d) is employed for jejunal nutrition because it is favorable to decrease infectious complications and expenses so as to reduce the duration of hospital stays (3). Gastrointestinal decompression tube is used to suck out gastric juice and part of the saliva in order to avoid the risk of their entering the vomica via fistula.
Not rinsing the vomica effectively while we found the anastomotic fistula due to the long-standing tracheo-mediastinal fistula, which leads to prolonged treatment duration, can be concluded as one of our major lessons. A conclusion can be drawn that, this therapy, with the benefits including mild trauma and long-term tube retention, will lead to positive and effective treatment even though the healing capacity of the tissue decreases due to radical radiotherapy.
Acknowledgements
We gratefully acknowledge the excellent advice given by professor Yu Yan and Junhua Liu.
Disclosure: The authors declare no conflict of interest.
References
- Zhang WM. Surgical treatment for recurrent esophageal carcinoma after curative radiotherapy. Applied Journal of General Practice 2007;5:1064.
- Löser C, Aschl G, Hébuterne X, et al. ESPEN guidelines on artificial enteral nutrition—Percutaneous endoscopic gastrostomy (PEG). Clin Nutr 2005;24:848-61. [PubMed]
- Jiang H, Jiang ZM. Does hypocaloric parenteral nutrition better for post-operative patient: a systematic review of the evidence with available clinical trials. JPEN supplement 2006Vinnars E, Wilmore D. History of parenteral nutrition. JPEN 2003;27:225-32.



