Guidelines for the diagnosis and treatment of malignant pleural mesothelioma
Foreword by Andrew Penman and Nico van Zandwijk
Malignant Pleural Mesothelioma (MPM), the asbestos-induced neoplasm originating in the mesothelial lining of the lung cavities represents significant diagnostic and therapeutic challenges for clinicians in Australia. Very seldom diagnosed prior to the advent of widespread asbestos mining in the early to mid-twentieth century, it has sharply risen in incidence over the last five decades. According to the most recent Australian Institute of Health and Welfare data, there were 666 cases of malignant mesothelioma diagnosed in Australia in 2009 and around 90% of them originated in the pleura.
MPM is almost always a fatal disease and the prognosis can only be modestly influenced by oncological treatments. The diagnostic process can be complex, with highly specialised advice frequently required to arrive at a definite diagnosis. Treatment varies from therapeutic nihilism to radical combined-modality treatment approaches. Although the disease and its management have a huge impact on the social, emotional, and material well-being of patients and families, supportive and palliative care pathways appear to be under-developed. The development of guidelines under the auspices of the Asbestos Diseases Research Institute (ADRI) has been undertaken in response to these circumstances. The guidelines organize the diagnostic and assessment process along the lines of the scientific evidence available, and provide for tailoring treatment on the basis of each patient’s characteristics. Considerable emphasis has been placed on investigating and addressing supportive and palliative care needs in MPM, however the volume and quality of evidence specific to MPM available in these domains was disappointingly small.
MPM is almost exclusively a man-made disease and Australia has one of the highest burdens of MPM on a population basis in the world. For the experts involved in collating and assessing the literature on the management of MPM for these guidelines, the level of active Australian research in areas such as diagnostic techniques, prognostic assessment, advanced radiotherapy techniques, and surgical outcomes has been a source of gratification. Many of these developments remain in the research and development phase.
These “Guidelines for the Diagnosis and Treatment of Malignant Pleural Mesothelioma” systematise the approach to the management of MPM based on the best available evidence in accordance with standards to the assessment of evidence developed by The National Health and Medical Research Council in 2011 (1). The ADRI, and the national team of experts involved in the preparation of the Guidelines, intends that they be a source of reference for health practitioners and consumers, because optimal management, by adherence to best practice guidelines, will improve the quality of life for each patient with MPM and their confidence in the treatment approach.
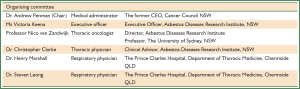
The development of “Guidelines for the Diagnosis and Treatment of Malignant Pleural Mesothelioma” has drawn on contributions from a large number of people. Particular thanks are due to the Steering Committee members who took responsibility for drafting each section of the Guidelines, to librarians Suzanne Bakker, Jeremy Cullis and Yaping Liu for the retrieval of relevant literature, to Christopher Clarke, Henry Marshall and Steven Leong for their detailed assessment and grading of evidence, and to Ms Victoria Keena of the ADRI whose energy and commitment over an extended period has been a source of strength to all. Many of these contributions were voluntary. All were beyond the strict call of duty. The reward for this effort will be in seeing these guidelines used widely leading to better outcomes for patients with MPM.
Executive summary
Malignant mesothelioma is an aggressive tumour originating in the serosal membranes that line the thoracic and abdominal cavities. More than 90% of reported mesothelioma cases occur in the pleura.
The occurrence of malignant mesothelioma is typically related to exposure to mineral fibres such as asbestos and erionite.
The World Health Organization (WHO) has recognised asbestos as one of the most important occupational carcinogens and in 2010 upgraded its global estimate of asbestos-related diseases (ARD) to 107,000 annual deaths. Australia, as one of the largest consumers of asbestos worldwide in the post-World War II period, has one of the highest incidences of malignant mesothelioma.
The current epidemic of malignant mesothelioma is closely associated with past occupational exposure. Asbestos, however, persists in our natural and built environments, and it is important that we continue to minimise exposure to it by all reasonable means.
There are indications that in Australia the diagnostic and treatment practices for MPM are not equally distributed, with considerable expertise concentrated in some hospitals and lacking in others. Moreover, there are no guidelines that specifically consider diagnosis and treatment of this almost invariably fatal disease in the Australian context.
These evidence-based guidelines have been developed by a multidisciplinary team (MDT) of experts (volunteers) that is encouraging improved management of MPM through evidence-based decision making. Guidelines are guides and not rules. A good approach is to be fully aware of appropriate guidelines before making management decisions.
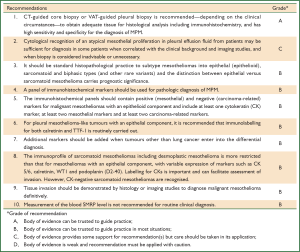
Summary of recommendations
Chapter 2—Diagnosis
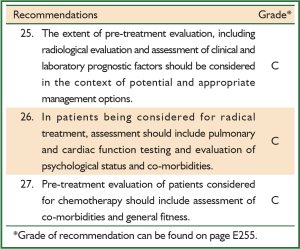
Chapter 3—Assessment
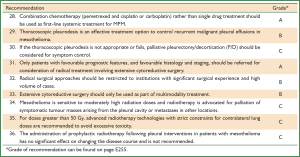
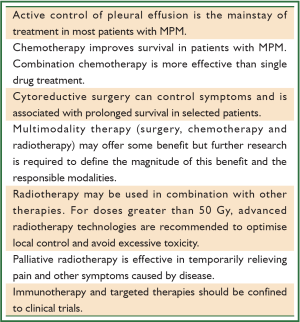
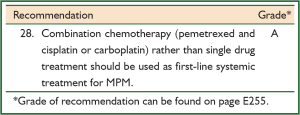
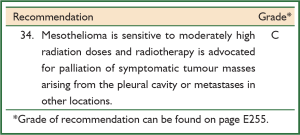
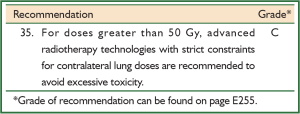
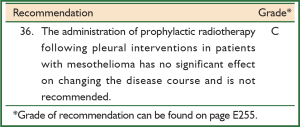
Chapter 4—Active anti-cancer treatment
Chapters 3 & 4—Assessment and active anti-cancer treatment
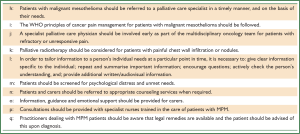
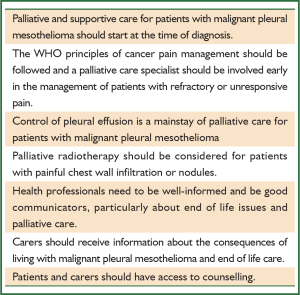
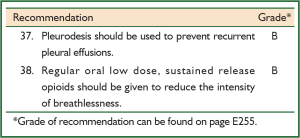
Chapter 5—Palliative and supportive care
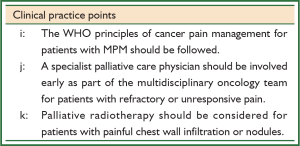
Clinical practice points
Chapter 2—Diagnosis
Chapter 3—Assessment
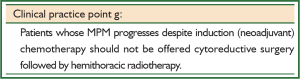
Chapter 4 —Active anti-cancer treatment
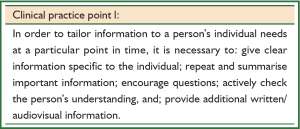
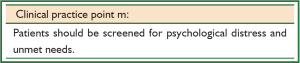
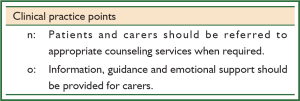
Chapter 5—Palliative and supportive care
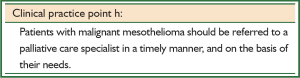
Chapter 6—Models of care
1 Introduction
1.1 Background
Malignant mesothelioma is an aggressive tumour that originates in the serosal membranes that line the thoracic and abdominal cavities. This disease has become an important health issue over recent years, with Australia having one of the highest reported incidences (2-4). More than 90% of reported cases of mesothelioma occur in the pleura, compared with 4-7% affecting the peritoneum, and fewer than 1% jointly occurring in the pericardium and tunica vaginalis testis (2,4,5). Even rarer cases have been recorded as apparently primary ovarian mesotheliomas (6,7).The occurrence of malignant mesothelioma is typically related to exposure to mineral fibres such as asbestos and erionite (8-10). Asbestos is a collection of naturally occurring crystalline hydrated silicates that are resistant to high temperatures and humidity. Asbestos fibres are biopersistent (retained in the human body) and can be detected as ‘asbestos bodies’ in the lung many years after inhalation (11).
The WHO has recognised asbestos as one of the most important occupational carcinogens and in 2010 upgraded its global estimate of ARD to 107,000 annual deaths (12).
1.2 History of mesothelioma
The first studies on the association between asbestos and malignant mesothelioma appeared in the 1950s. Weiss’ case report of asbestosis and pleural malignancy and Van der Schoot’s paper describing three insulation workers with malignant disease were the first of many to be published (13,14). Wagner confirmed the association between asbestos and malignant mesothelioma through his work in the 1950s in South Africa, a country that mined all three commercial types of asbestos (15).
Because most asbestos exposure occurred in the work environment, malignant mesothelioma has traditionally been considered an occupational disease. Para-occupational malignant mesothelioma has been described in households of asbestos workers in which cohabitants had been exposed via contaminated clothes (16). The term ‘environmental malignant mesothelioma’ has been used to describe disease identified in people living close to asbestos mines or factories or when people have been exposed to asbestos or asbestos-like material present in the soil (17,18).
Other factors have been recognised as potential causes of malignant mesothelioma. Radiotherapy to the chest has been reported but the number of patients with this association is limited (19). The role of SV40 (one of the simian viruses) viral infection as an important etiologic cofactor in malignant mesothelioma remains under discussion (20,21).
Exposure to asbestos is more common in occupations with a predominantly male workforce, which explains why the current incidence of malignant mesothelioma is higher among men than women. Most mesothelioma patients have been primary asbestos workers or people who handled raw asbestos in the mining, milling, transportation and manufacturing of the material. As this high-risk occupational exposure has been limited by the total ban on the use of asbestos products in Australia, the exposure-mix may change to include a greater proportion of people who have been exposed in non-occupational settings.
A dose-response relationship between cumulative asbestos exposure (increased levels or duration of exposure, or both) and malignant mesothelioma has been demonstrated (22). A ‘safe’ threshold of cumulative exposure, below which there is no increased risk, has not been defined (23).
The latency period, or the period between first exposure to asbestos and the diagnosis of mesothelioma, shows a wide range (20-60 years) and there are indications that the latency in Australia has increased in recent years (24). The median age at diagnosis of malignant mesothelioma in Australia is slightly above 70 years, with many patients presenting with co-morbidities (4).
1.3 Incidence of malignant mesothelioma
Variation in the incidence of malignant mesothelioma is reported in different parts of the world. For example, seven people per million in Japan have been diagnosed with malignant mesothelioma compared with 40 people per million in Australia. These differences are largely attributable to the amount of asbestos ‘consumed’ in a certain period (25).
Australia, as one of the largest consumers of asbestos worldwide in the post-World War II period, has one of the highest incidences of malignant mesothelioma. Around 660 new cases of malignant mesothelioma were documented in 2007 and, in terms of mortality, this disease is approaching the numbers of deaths caused by multiple myeloma and ovarian cancer.
There is also regional variation in the incidence of malignant mesothelioma. For example, in Australia the highest reported incidence has been in men in Western Australia. This variation is largely attributable to occupational exposure associated with crocidolite mining in Wittenoom (3).
Most deaths caused by malignant mesothelioma in Australia and other developed countries are due to occupational exposure to asbestos. The frequency of cases attributable to occupational exposure may have begun to decline owing to stringent control of asbestos use and handling. Asbestos, however, persists in our natural and built environments, and it is important that we continue to minimise exposure to it by all reasonable means. Among mesothelioma patients who do not have a history of occupational exposure, there is now a high proportion of people with a history of home renovation, in which exposure to asbestos might have occurred (26). Research is needed to determine if asbestos exposure explains this high proportion. It is important also that we remain alert to sources of possible exposure to asbestos in the community and control any such exposure as it is identified.
Data on the incidence and mortality of malignant mesothelioma in Aboriginal and Torres Strait Islanders and culturally and linguistically diverse groups has not been reliably estimated due to the lack of recorded ethnicity. However, from July 2010, all new cases of malignant mesothelioma diagnosed in Australia are monitored by the Australian Mesothelioma Registry.
1.4 Clinical need for these Guidelines
A recent study highlighted the lack of standardisation or adherence to guidelines during diagnosis, treatment, and surveillance of cancer patients as one of the major barriers to providing high quality cancer care (27).
According to the US Institute of Medicine (28), high quality health care must be:
- based on the best evidence;
- efficient;
- safe from avoidable errors;
- delivered in a timely manner;
- patient-centred;
- equitable.
There is scant data available on the current medical practices for patients with MPM in Australia. A report on 295 patients diagnosed with malignant mesothelioma in the 1980s found considerable variation in practice (29). There are indications that diagnostic and treatment practices are not equally distributed, with considerable expertise concentrated in some hospitals and lacking in others.
Several clinical guidelines for MPM have been published recently (21,30-35). All were collated by experts but none of them used a systematic analysis of the literature retrieved through general search terms and patient, intervention, comparison, outcome (PICO) questions as required by the Australian National Health and Medical Research Council (NHMRC) (1). Moreover, there are no guidelines that specifically consider diagnosis and treatment of MPM in the Australian context. To address this gap, a team of experts decided to write guidelines based on a systematic review of the available literature.
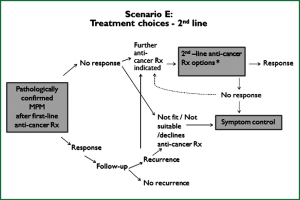
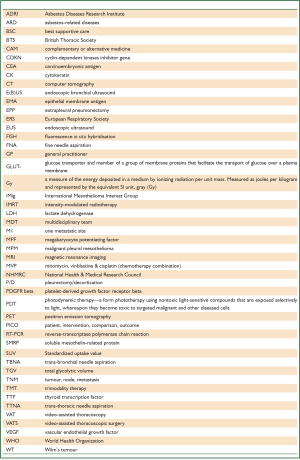
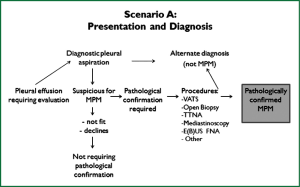
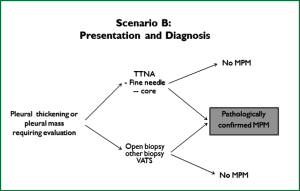
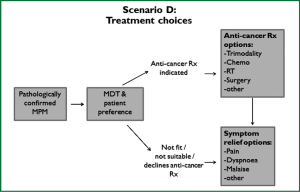
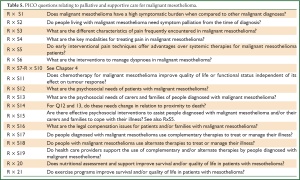
These guidelines are based on a systematic review of the literature executed according to the NHMRC guidelines development plan (36). ‘Primum non nocere’ was regarded a primary issue when formulating the guideline recommendations. In addition we have drafted five scenarios that have assisted us in selecting the most important PICO questions. Scenario A (Figure 1) is based on the most common presentation of patients with malignant mesothelioma—those presenting with a pleural effusion. Scenario B depicts another (less frequent) pathway, when a patient presents with a pleural mass (Figure 2). In scenario C the assessment journey of patients with a pathologically confirmed diagnosis is outlined (Figure 3) and scenario D deals with treatment choices for malignant mesothelioma patients after diagnosis and assessment (Figure 4). Scenario E (Figure 5) depicts the second-line treatment choices. PICO questions were formulated according to these scenarios and literature searches were based on these PICO questions (see Tables 1-6). The evidence found in the literature searches was graded to produce evidence-based recommendations applicable to the Australian clinical context. Although the cutoff date of the literature review was 31st October 2011, a few exceptions (eight) were made to include prominent articles that were published after this date, adding important new information. These guidelines will provide a benchmark for the evaluation of current patterns of care for patients with MPM.
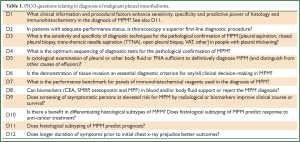
Full table
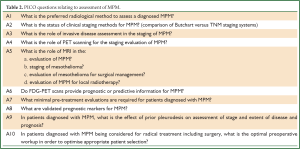
Full table
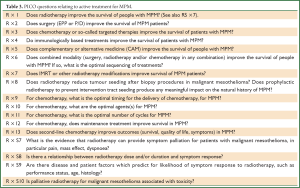
Full table
Full table
Full table

Full table
Although there is a substantial evidence base to draw on, the number of comparative randomised studies on MPM is limited, and a sufficient level of evidence to make definitive recommendations was not always available. When quality evidence was lacking, consensus-based recommendations were formulated according to the guidelines of NHMRC (1).
1.5 Purpose of these Guidelines
The purpose of these Guidelines is to provide clear and concise evidence-based recommendations for the diagnosis, treatment and care of patients with MPM in Australia. The Guidelines will contribute to improving treatment planning for patients with MPM by assisting in identifying where quality treatment and patient volume are related and where specialist and multidisciplinary (palliative/supportive) teams are needed.
1.6 Intended users and scope of these Guidelines
These Guidelines are intended for use by:
- general practitioners (GPs), who are most likely to first encounter patients with complaints and symptoms that will eventually lead to the diagnosis of MPM;
- respiratory physicians, who in most cases will be responsible for initiating the diagnostic process;
- pathologists, radiologists, nuclear medicine specialists, surgeons, medical and radiation oncologists, palliative care specialists and nurse specialists, involved in the confirmation of the diagnosis or in drafting a treatment plan;
- allied health professionals;
- consumer representatives;
- health service planners, managers, funders and policy makers responsible for providing services for patients with malignant mesothelioma;
- patients and carers affected by malignant mesothelioma.
As indicated earlier, the scope of these Guidelines is confined to clinical pathways initiated when a person presents with signs and symptoms and/or preliminary tests suggestive of MPM. They provide recommendations for the diagnosis and treatment of patients with MPM who are admitted to Australian hospitals. The areas covered include diagnosis, assessment, active treatment, palliative and supportive care and preferred models of care. From these evidence-based guidelines a consumer version will be produced for patients and their carers.
Given the poor prognosis for patients with MPM, particular attention has been given to the following outcomes:
- short term mortality, morbidity and treatment complications;
- physical and social functioning;
- quality of life, general health status and patient satisfaction.
The Guidelines do not specifically deal with the epidemiology of malignant mesothelioma, population measures to reduce exposure risk, chemoprevention or other personalised prevention measures for individuals who have been exposed to asbestos and/or erionite. Also the Guidelines do not deal with cost implications (cost-effectiveness) of the diagnostic procedures and treatment approaches as recommended.
During the development of these Guidelines we have identified a number of future research areas that are listed in Appendix A.
1.7 Methods used to develop these Guidelines
The ADRI, established by the Asbestos Diseases Research Foundation, in collaboration with a national team of experts, has developed these Guidelines in accordance with NHMRC guideline development processes (1).
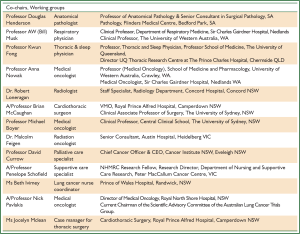
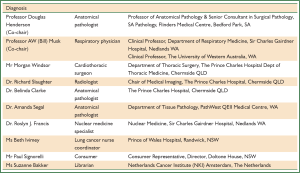
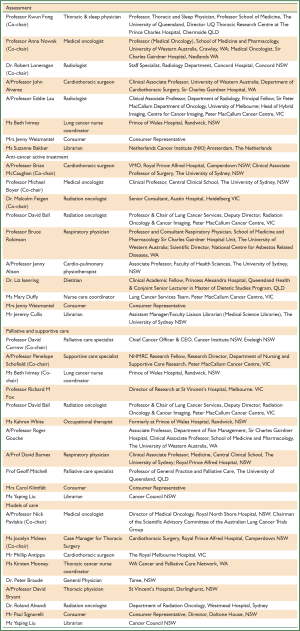
In February 2010, ADRI convened a MDT with expertise in malignant mesothelioma. Details of the membership of the Steering Committee for the Guidelines and the five expert Working Groups involved in reviewing evidence and formulating recommendations are provided in Appendix B. The process of appointment for members of the Steering Committee and the Terms of Reference are also included in Appendix B. Given the poor prognosis of MPM, achieving consistent consumer representation over an extended period for the development of guidelines was challenging. The ADRI’s close relationship with the Asbestos Disease Foundation of Australia was an invaluable asset in engaging consumers. The financial support and involvement of the Biaggio Signorelli Foundation was further testament to the strong consumer interest and engagement with the development of these Guidelines. There have been reports on specific asbestos exposures experienced by a number of aboriginal communities in Australia, notably in Wittenoom, Roebourne and Baryulgil (37,38). However, there is not enough medical data available to allow accurate assessment of the incidence and mortality of asbestos-related disease in these communities. The developers of these Guidelines have made an effort to engage a representative of the Aboriginal Community as a consumer representative. Unfortunately we haven’t been successful. Given the current incidence of MPM and the short life expectancy after diagnosis this was not an unexpected outcome.
The Technical Report attached to these Guidelines includes a description of the process used to develop clinically meaningful guidelines in the Australian context, the literature search and the development of recommendations.
1.8 Scheduled review of these Guidelines
NMHRC recommends that guidelines be reviewed and revised no more than five years after initial publication. The Steering Committee will be reconvened to review relevant sections of the Guidelines if any of the following occur within five years:
- registration by the Australian Therapeutic Goods Administration of any new drugs for the treatment of patients with malignant mesothelioma;
- publication of new major randomised controlled trials or systematic reviews that have a potential effect on diagnosis treatment or care of patients with malignant mesothelioma.
1.9 Funding
The development of these Guidelines was made possible by a generous donation from the Biaggio Signorelli Foundation; a Cancer Institute NSW grant and a contribution from Cancer Council NSW. Publication of the Guidelines has been made possible by a grant from Comcare’s Asbestos Innovation Fund.
2 Diagnosis
Key messages
2.1 Introduction
The diagnosis of malignant mesothelioma can be difficult, with symptoms and clinical findings that can mimic and be mimicked by other diseases. Pleural mesothelioma patients may present with dyspnoea, chest pain (pleuritic or non-pleuritic), cough and weight loss, or any combinations of these symptoms (39-42). Initial clinical and radiological examination usually reveals a pleural effusion, often massive. Rarely, patients are asymptomatic at the time when a radiological abnormality is demonstrated, and patients seldom present with metastatic disease.
Some patients with malignant mesothelioma experience a long interval between the first onset of symptoms and subsequent diagnosis, but whether a long interval signifies enhanced or diminished survival following diagnosis is unclear. Most patients with MPM have a background of asbestos exposure (40,42), and some may have had antecedent symptoms associated with benign asbestos-related disease—for example, symptoms related to asbestosis or benign asbestos pleuritis with effusion. Others may have radiological evidence of past asbestos exposure, such as pleural plaques.
In general, biopsy, immunohistochemical analysis and correlation with radiological and clinical features are needed for the diagnosis of mesothelioma (42). When immunohistochemical findings are non-diagnostic or discordant, electron microscopy—including electron microscopic examination of tissue retrieved from blocks of paraffin-embedded biopsy tissue or cytology cell blocks—can be used, but electron microscopy is not recommended for ‘routine’ diagnosis of mesothelioma (21,43).
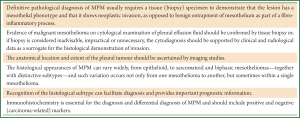
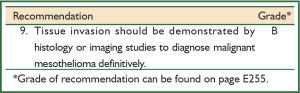
Although several cytological and histological findings may raise varying levels of suspicion of MPM (see section 2.4) a current requirement for the definitive clinicopathological diagnosis of MPM is the demonstration of neoplastic invasion—for example, infiltration into subpleural fat, chest wall skeletal muscle, rib or lung—by histological examination or by imaging studies (41,44,45), and by clinical exclusion of alternative causes for an atypical mesothelial proliferation.
A component of malignant mesothelioma in situ can be diagnosed when invasion has been demonstrated in the same or different biopsy or by imaging studies (44). This applies specifically to epithelioid malignant mesotheliomas. Sarcomatoid malignant mesotheliomas are rarely diagnosable from effusion fluid cytology and are usually identified histologically, by the demonstration of invasion or overtly sarcomatoid areas.
2.2 First-line diagnostic procedures
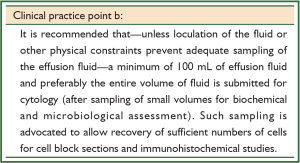
After clinical assessment and imaging studies such as chest X-ray or CT imaging, thoracocentesis with aspiration of pleural effusion fluid is usually conducted as the first-line pathological assessment (please see later discussion on the cytodiagnosis of malignant mesothelioma). In many centres, tissue biopsy is the primary investigation for diagnosis, but some patients are in poor physical condition and unable to tolerate a surgical procedure.
In general, the confidence index for a biopsy diagnosis of malignant mesothelioma is proportional to the volume of tumour sampled. A number of factors influence the choice of, and prioritisation for, different types of biopsy, including:
- the general medical condition of the patient and any co-morbidities that contraindicate procedures which are more invasive than others;
- the clinical imaging findings—for example, a pleura-based mass lesion is often amenable to a core biopsy, with a high diagnostic yield in comparison to a case where no significant pleural thickening or mass is detectable (46-48);
- existing patterns of clinical practice at the medical centre where the patient is under management.
Procedures used include ‘blind’ percutaneous needle biopsy, fine needle aspiration (FNA) biopsy, imaging-guided core biopsy, video-assisted thoracoscopy (VAT)-guided biopsy and thoracotomy.
Thoracocentesis with cytological examination is discussed below. FNA biopsy has a low diagnostic yield (about 30%) and is not routinely recommended in malignant mesothelioma diagnosis (21). Likewise, percutaneous pleural biopsy has a low diagnostic yield and is not recommended for routine diagnosis (41,42).
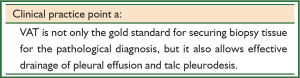
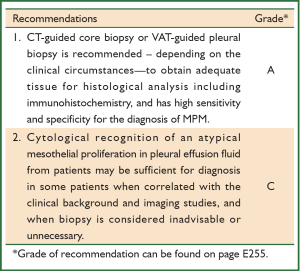
Thoracoscopy-guided biopsy and CT-guided core biopsies have high sensitivity and low complication rates, depending on the circumstances and indications for each, with a diagnostic yield of about 80-90% or more (21,46-51). CT-guided core biopsy is suitable for cases where imaging studies have demonstrated pleural thickening or a nodular/mass lesion, and in such cases this procedure has a high diagnostic yield and usually few complications (46-48). Standard VAT-guided biopsy is suitable for other patients with a pleural effusion but no mass lesion, or patients for whom surgical pleurodesis is considered (21,47). In the 2010 Guidelines from the European Respiratory Society (ERS) and the European Society of Thoracic Surgeons (ESTS), thoracoscopy was the preferred technique, allowing extensive inspection of the pleura and the taking of multiple and large biopsies that include subpleural tissue for the histological assessment of invasion (21). VAT is tolerated well in general, with a low complication rate (41,42,52). Flexible thoracoscopy under local analgesia or neurolept anaesthesia is used increasingly by respiratory physicians, with a diagnostic yield comparable to standard surgical VAT (52).
Even so, the diagnostic return from a VAT-guided biopsy is not quite equivalent to that of an open biopsy, which also allows more accurate subtyping of mesothelioma (50,53,54)—83% for open biopsy in comparison to 74% for VAT-guided biopsy, and 44% for CT-guided biopsy, as reported by Kao et al. (55) for a series of extrapleural pneumonectomy (EPP) patients. However, the 2004 WHO chapter on mesothelioma states that thoracotomy is not required for diagnosis—VAT being sufficient—and is best avoided because of the risk of ‘tumour implantation in the chest wall’ (40). ‘Thoracotomy’ should probably be restricted to a small incisional biopsy into the chest wall for those cases where the pleural space has been obliterated—so that VAT cannot be performed. Cytological examination of effusion fluid usually allows for detection of epithelioid cells only, so that mesotheliomas with a sarcomatoid component will not be recognised as such.
2.3 Sequencing of diagnostic tests
There is no evidence regarding the optimum sequencing of diagnostic tests for the pathological confirmation of MPM. The usual sequence is imaging studies (for example, a CT scan), followed by aspiration of effusion fluid, then limited or VAT-guided biopsy.
2.4 Cytological features of malignant mesothelioma
The majority opinion among surgical pathologists is that an essential condition for definitive histological diagnosis of pleural mesothelioma is the demonstration of neoplastic invasion—such as infiltration into underlying fat, skeletal muscle, rib or lung—as opposed to benign entrapment of mesothelium (21,45,56,57).
Effusion fluid cytology in isolation does not allow assessment of invasion, although a 2007 Update Statement on Mesothelioma from the British Thoracic Society (BTS) (42) stated that cytological examination of pleural effusion fluid from patients may be sufficient for diagnosis in some patients, when correlated with imaging studies—that is, using imaging studies as a surrogate for the histological demonstration of invasion (42).
For example, the combination of the following may allow a diagnosis of mesothelioma at a high level of confidence: florid atypical mesothelial proliferation on pleural effusion fluid cytology supported by immunohistochemical studies on cell-block sections and with no evidence of any infective process on microbiological investigation, plus confluent pleural thickening with nodularity on imaging studies (with/without evidence of chest wall invasion), plus absence from imaging studies of any intrapulmonary mass lesion or extrathoracic tumour with the capacity for spread to the pleura.
Cytology-only diagnosis based on effusion fluids remains controversial (41). Although several cytological findings raise varying levels of suspicion of MPM (58) —such as the extent of the mesothelial proliferation, the presence of papillary structures (especially in the pleura), cytological atypia, frequent cytoplasmic vacuoles and focal necrosis—there is some overlap in the cytological appearances between reactive mesothelial hyperplasia and malignant mesothelioma (40,41,56,57).
The most useful cytological features of malignant mesothelioma include the presence of numerous relatively large (>50 cell) balls of cells with berry-like external contours comprising cells that are much larger (with enlarged cytoplasm, nucleus and nucleolus) than most benign mesothelial cells; the presence of macronucleoli—although prominent nucleoli can be present in reactive mesothelial cells and not all malignant mesothelioma cells have macronucleoli; and nuclear atypia.
Many cytological features of malignant mesothelioma—such as scalloped borders of cell clumps, intercellular windows, variation in cytoplasmic staining and its ‘density’, and low nuclear-to-cytoplasmic ratios—are shared between reactive and malignant epithelioid mesothelial cells (45).
Reported sensitivities for a clear cytodiagnosis of mesothelioma on effusion fluids have ranged widely. One 1997 study reported a low sensitivity of 32% (59). In another study of 162 cases (60), effusion fluid cytology showed high specificity (~99%) when all criteria specified for mesothelioma were fulfilled, but the sensitivity was only 47.5% when not all criteria were met. This sensitivity was improved by interpreting the cytological findings together with effusion fluid hyaluronic acid concentrations. Some centres with specialised interest and experience in the cytodiagnosis of mesothelioma from effusion fluid (58) have found a high positive predictive value for diagnosis. Such results may not be obtainable for other centres with less experience in cytological assessment of mesothelial proliferations.
Some investigators have found that strong circumferential immunolabelling of mesothelial cells for epithelial membrane antigen (EMA) is evidence in favour of mesothelioma as opposed to reactive mesothelial hyperplasia (61-63)—provided that the EMA antibody is based on the E29 clone (44,64). Positive labelling for GLUT-1 also appears to favour a diagnosis of mesothelioma (65). Conversely, immunolabelling for desmin is claimed to be evidence in favour of a benign mesothelial proliferation (62,63).
There is evidence that homozygous deletion of the cyclin-dependent kinase inhibitor gene p16/CDKN2A, as demonstrated by fluorescence in situ hybridisation (FISH), may be useful for the distinction between malignant mesothelioma and benign reactive mesothelial proliferations, with sensitivity and specificity in one study that were superior to immunolabelling for GLUT-1 (66). For example, three studies (66-68), have reported such deletions of p16 in 43-70% of pleural mesotheliomas (mainly but not exclusively epithelioid mesotheliomas), but not in reactive mesothelial hyperplasias. The presence of this deletion was associated with a poorer prognosis than for those mesotheliomas without it (68). The p16 deletion was less frequent in peritoneal mesotheliomas than in pleural mesotheliomas (66,67). However, at present there is insufficient evidence that these markers, either in isolation or in combination, have demonstrated sufficient specificity, consistency and reproducibility to replace biopsy or imaging evidence of invasion (44,45). See also section 2.9.
Also, malignant cells in sarcomatoid malignant mesothelioma tend not to be shed into the effusion fluid, yet the fluid may contain reactive epithelioid mesothelial cells that can be misleading. In addition, sarcomatoid mesotheliomas are less frequently associated with a pleural effusion than mesotheliomas with an epithelial component. Effusion fluid cytology is rarely diagnostic with sarcomatoid, pleomorphic, lymphohistiocytoid and desmoplastic mesotheliomas, and can lead to false diagnosis.
The cytological distinction between mesothelioma and secondary carcinoma is less problematic now than in earlier decades—provided that the sample submitted is adequate for preparation of a cell block for immunohistochemical studies.
2.5 Histological features of malignant mesothelioma
Most malignant mesotheliomas can be identified or strongly implicated by routine haematoxylin-eosin (H&E) histology. Determining the histological subtype of malignant mesothelioma is a factor that influences prognosis in this disease.
Mesotheliomas can be broadly divided into three histological subtypes—epithelioid, sarcomatoid and biphasic (mixed epithelioid and sarcomatoid)—with a number of rare variants (40,41,44,45). This classification facilitates the differential diagnosis of benign and malignant lesions and subsequent immunohistochemical analysis.
Epithelioid mesothelioma is the most common subtype and accounts for about 60% of all mesotheliomas (40,41,44,45). These tumours contain polygonal, oval or cuboidal cells that often mimic reactive mesothelial cells that occur in response to various types of injury. The differential diagnosis also includes metastatic carcinomas (lung, breast, ovarian and colonic adenocarcinomas and squamous cell and renal cell carcinomas) and other epithelioid tumours, as well as reactive mesothelial proliferations (45).
Sarcomatoid malignant mesotheliomas represent about 10-20% of mesotheliomas (41,44) and consist of spindle cells that may mimic malignant mesenchymal tumours such as malignant fibrous histiocytoma, leiomyosarcoma or synovial sarcoma (69). The sarcomatoid tissue rarely shows heterologous differentiation such as osteoid/bone or cartilage (70).
Biphasic malignant mesotheliomas contain a mixture of epithelioid and sarcomatoid areas within the same tumour and comprise about 30% of mesotheliomas (40,41). Malignant mesotheliomas are arbitrarily classified as biphasic when there is at least 10% of each component (40,41,44). When there is less of either, the malignant mesothelioma can be designated as predominantly sarcomatoid or predominantly epithelioid. The differential diagnosis includes synovial sarcoma and other biphasic or mixed tumours.
The histological distinction between a desmoplastic malignant mesothelioma and benign fibrous pleuritis can be difficult, with potential for either benign or malignant misdiagnosis. Malignant mesotheliomas are arbitrarily classified as desmoplastic when hypocellular collagen-rich tissue represents 50% or more of an adequate biopsy sample (40,41,44,71).
Useful criteria for the biopsy diagnosis of desmoplastic malignant mesothelioma are (40,44,45,71):
- identification of neoplastic invasion—as opposed to benign entrapment of mesothelium due to a fibro-inflammatory disorder, or artefact that can be misconstrued as invasion of fat in cases of fibrous pleuritis;
- identification of overtly sarcomatoid areas;
- the combination of an abnormal architecture for the collagen-rich fibrous tissue that characterises desmoplastic malignant mesothelioma, such as a storiform or nodular architecture, and absence or reversal of the zonal architecture characteristic of benign pleuritis, plus the presence of focal ‘bland’ necrosis.
Desmoplastic mesotheliomas appear to have a propensity to metastasise to bone, and the metastases can rarely facilitate correct diagnosis for an antecedent pleural lesion (fibrous pleuritis) (44). Metastases from desmoplastic mesotheliomas are also liable to misinterpretation as a primary fibrous tumour of bone (40).
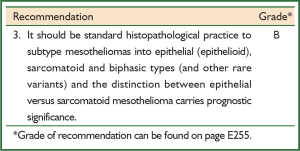
2.6 Differentiating between histological subtypes
Recognition of histological subtypes of a suspected malignant mesothelioma facilitates selection of the most appropriate immunohistochemical protocol for diagnosis and is of significance for prognosis (40,42,72-77).
Some specific subtypes of malignant mesothelioma are particularly liable to misdiagnosis, such as desmoplastic sarcomatoid mesothelioma, and lymphohistiocytoid, pleomorphic (epithelial or sarcomatoid), small cell, clear cell and localised malignant mesotheliomas (41,44).
2.7 Immunohistochemistry in the diagnosis of malignant pleural mesothelioma
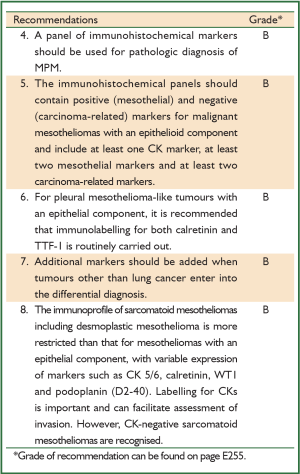
Immunohistochemistry is integral to the diagnosis of malignant mesothelioma and is currently the most useful and standard ancillary procedure for distinguishing this malignancy from other types of cancer.
The primary differential diagnosis for epithelioid mesothelioma in the pleura is with metastatic lung adenocarcinoma. Immunohistochemistry has replaced electron microscopy as the preferred ancillary method, and differential diagnosis now relies on the detection of various mesothelial and carcinoma-related antigens/markers in cytology cell block sections or in biopsy tissue (21,40,41,44,45,63,78,79). Carcinoma-related markers include carcinoembryonic antigen (CEA), LeuM1 (CD15), Ber-EP4, B72.3 and BG8 (45,63,80-84) and—whenever lung adenocarcinoma is included in the differential diagnosis—thyroid transcription factor-1 (TTF-1) (45) and/or napsin A (85,86). Antigens characteristically expressed by mesothelial cells include calretinin, Wilms’ tumour gene product (WT-1), mesothelin, CK 5/6, HBME-1 antigen (63,79,87-100), thrombomodulin and podoplanin (D2-40) antibody (101-113) .
The exact combination and number of antigens to evaluate is dependent on the differential diagnosis and the antibodies available. Currently, calretinin is considered to have the greatest specificity for a diagnosis of malignant mesothelioma, followed by WT1 and D2-40 (21,44,45,79,99). The International Mesothelioma Panel (IMP) (41) recommends at least one CK marker plus at least two mesothelial markers (for example, calretinin and WT1) together with at least two carcinoma-related markers (for example, CD15 and TTF-1). The guidelines from the ERS and the ESTS (21) reiterate this IMP approach, as do the Guidelines from the International Mesothelioma Interest Group (IMIG) (45). When tumours other than lung cancer enter into the differential diagnosis (for example, secondary prostate carcinoma) additional markers become necessary. The ERS/ESTS guidelines do not recommend use of CK7/CK20 (114) for diagnosis of mesothelioma (21).
As a practical reference for pathologists, the IMIG recommends that markers have sensitivity or specificity greater than 80% for the lesions in question (45), whereas the ERS/ESTS guidelines specify a minimum sensitivity of 60-70%. Interpretation of positivity should take into account the localisation of the stain (for example, nuclear versus cytoplasmic) and the percentage of cells stained: more than 10% has been suggested for cytoplasmic membranous markers (45).
From the preceding discussion, it is clear that none of the antibodies used for the diagnosis of mesothelioma is 100% specific or sensitive—hence the requirement for panels of mesothelial and non-mesothelial antibodies. As one example of the diagnostic pitfalls that can be encountered, up to 15% of a subset of high-grade carcinomas of the breast can express calretinin, and these carcinomas may also express CK5/6 and lack detectable oestrogen receptor protein—with the potential for misdiagnosis of pleural metastases as malignant mesothelioma (115,116).
Immunohistochemistry has a more restricted role for the diagnosis of sarcomatoid malignant mesotheliomas than for malignant mesotheliomas with an epithelial component, because many sarcomatoid malignant mesotheliomas express only CKs in addition to vimentin and, in some cases, smooth muscle markers (44,45,117,118). Expression of calretinin is variable (30-89%) in sarcomatoid areas of mesothelioma (40,41,44,111,117,119). The high percentage labelling recorded in some studies is explicable by acceptance of cytoplasmic labelling for calretinin as a positive result (117), whereas positive nuclear labelling is required in addition to any cytoplasmic labelling (41,44). Most sarcomatoid and desmoplastic malignant mesotheliomas are strongly positive for CKs (although CK-negative sarcomatoid malignant mesotheliomas do occur), and CK labelling can also highlight invasion, such as genuine invasion into subpleural fat by a desmoplastic malignant mesothelioma (44). The ERS/ESTS guidelines recommend use of at least two broad-spectrum CK antibodies and two markers with negative predictive value, to support a diagnosis of sarcomatoid mesothelioma (21).
The place of immunohistochemistry in the diagnosis of MPM is a constantly evolving area and specific information on antibodies and their source should be obtained from the current literature. It also seems likely that molecular approaches to diagnosis (120)—such as profiling of microRNA expression in tumour tissue (121) or extrapleural samples—will supplement immunohistochemistry for the diagnosis of mesothelioma, but these approaches are at an investigational phase of evaluation and at present they cannot be recommended for routine use in diagnosis.
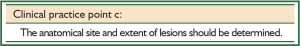
2.8 Anatomical features of malignant pleural mesothelioma
Anatomical aspects of MPM are important to support a clinicopathological diagnosis, in particular when biopsy tissue is insufficient to obtain a clear and definitive diagnosis.
Clinical information such as the anatomical distribution of the lesion as shown by imaging studies should be obtained (42). For example, whether:
- the lesion is pleura-based and confluent;
- the lesion is an intrapulmonary mass with characteristics of a primary lung cancer;
- there is an extrapleural tumour elsewhere with the capacity to metastasise to the pleura;
- there is a pleural effusion and, if present, its size.
This information can be important for probabilistic clinicopathological assessment when the amount of tissue taken with a small core biopsy is insufficient for diagnosis in isolation, or when there are discordant immunohistochemical findings, or when the tumour is undifferentiated and not clearly classifiable by immunohistochemistry. Even so, CT imaging—although a standard procedure for the investigation of mesothelioma—may not detect superficial invasion of subpleural tissues by early stage mesotheliomas (40).
2.9 Distinguishing benign mesothelial hyperplasia from malignant pleural mesothelioma
As emphasised earlier in this chapter, the demonstration of fat or stromal tissue invasion by histology or imaging is an essential criterion for definitive diagnosis of MPM.
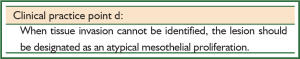
Although reactive mesothelial proliferations are non-invasive, entrapment of benign mesothelial cells within the fibrous tissue of organising inflammation can simulate neoplastic invasion (44,45). This can make histological discrimination between entrapment and invasion difficult. It is recommended that when invasion cannot be identified in biopsy tissue, the lesion should be designated as an atypical mesothelial proliferation (41,44,45).
Clinical decision-making for a diagnosis of malignant mesothelioma may be made when a limited biopsy has shown an atypical mesothelial proliferation without invasion. This requires correlation with imaging studies, a more adequate biopsy or, in many instances, serial imaging studies to ascertain whether the lesion is progressive (42).
2.10 Molecular biomarkers and screening
Serum biomarkers such as mesothelin (also known as soluble mesothelin-related protein or SMRP), osteopontin, CA125 and megakaryocyte potentiating factor (MPF) have been investigated as tools to aid the diagnosis of malignant mesothelioma, or for screening of ‘at risk’ groups (120,122-142). A positive blood test for mesothelin at a high specificity threshold is a strong incentive for further diagnostic steps, provided there is no renal failure (141,143). However, the poor sensitivity of mesothelin at diagnosis (35-50%) limits its value. In screening studies, mesothelin levels are elevated before diagnosis in fewer than 15% of mesothelioma patients in a high risk group, so it is not recommended as a screening tool (144).
Also osteopontin and CA125 lack specificity as diagnostic markers (127,131), but serum mesothelin and CA125 may have value in monitoring response to treatment (145,146). To date, no serum biomarker has shown sufficient positive predictive value for a diagnosis of malignant mesothelioma that would allow it to replace existing imaging-cytology-biopsy requirements (120,144-147). (See preceding mention of p16/CDKN2A, in section 2.4.).
Whenever pleural synovial sarcoma enters into the differential histological diagnosis, tumour tissue should be investigated by either FISH or the reverse-transcriptase polymerase chain reaction (RT-PCR) for the t(X;18) translocation diagnostic of synovial sarcoma (SYT-SSX) (148,149).
Sarcomatoid mesothelioma and especially desmoplastic mesothelioma have significantly shorter median survival times than epithelioid mesotheliomas (40,42,72,73)—and thus they represent markers for particularly poor prognosis—and are usually unresponsive to chemotherapy (see section 2.5, Recommendation 3 and Chapter 4).
There is no evidence that screening procedures for malignant mesothelioma affect clinical outcomes and most authorities recommend against ‘routine’ screening(21,146).
3 Assessment
Key messages
3.1 Introduction
Following a diagnosis of MPM by pathological means, further assessment and characterisation of the disease provides the following information:
- baseline status to assess response to therapy;
- an estimate of prognosis of disease;
- guidance for treatment planning;
- selection of patients for radical surgical therapy;
- evaluation of residual disease after therapy;
- stratification of patients to be enrolled in clinical trials;
- accurate data for disease registers—epidemiology and outcomes.
3.2 Disease staging
Correct staging is important for several reasons. It ensures:
- appropriate management plans can be made;
- appropriate information is collected for clinical trials and translational research;
- the anatomical spread of MPM can be adequately described by, and communicated among, health professionals.
A common system for disease staging is important for comparing the outcomes obtained with different forms of treatment.
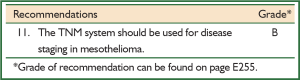
For most major tumour types, large datasets have been made available to validate the prognostic importance of the TNM system but scant prospective staging data is currently available for MPM.
The initial staging system for MPM was a four-stage system introduced by Butchart (150) and based on observations in 29 patients only. In subsequent years modifications were proposed by a number of investigators including Mattson, Boutin and Sugarbaker (151-153). These staging systems also suffered from the limitation of being based on small numbers of patients. The IMIG/International Association for the study of Lung Cancer (IASLC) staging system proposed by Rusch in 1995 (154) was the result of a retrospective analysis of several small surgical databases. It was based on the TNM descriptor system, which requires surgical (pathological) confirmation. It was unclear if stage estimated by clinical investigations might have the same predictive power as a pathologically-based system.The IMIG staging system could predict prognosis (155-159), but in the clinical setting this system failed as an independent (multivariate analysis) prognostic factor (160,161). After the first analysis of an IMIG/IASLC database with data from 3,101 patients with MPM, several areas of the current staging system have been defined as requiring modification (162). Multivariable analyses showed significant differences in overall survival for most T stages but not for T2 vs. T1. Although a negative node status was of prognostic importance, no difference between N1 and N2 was noted.
Disease stage according to the TNM system, when assessed by surgical staging, is a significant predictor of prognosis in patients with mesothelioma, and is the preferred system.
3.3 Clinical staging and assessment
Computed tomography is the preferred radiological method to assess patients with MPM. Plain chest radiography lacks sufficient sensitivity for routine staging because small malignant pleural effusions are not detected and large pleural effusions can obscure pleural/chest lesions (163). Furthermore, positive plain radiographic findings in patients do not clearly discriminate between MPM and other diagnoses, such as carcinoma metastatic to the pleura, lymphoma or benign asbestos disease.
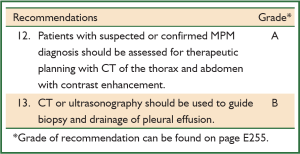
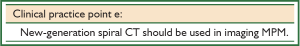
CT provides better information than plain radiography with regard to tumour characteristics and extent of disease (163). CT is the radiological standard used for staging of disease, identifying possible resectability of primary tumour and baseline pre-chemotherapy assessments. The sensitivity of CT is limited when it concerns the early detection of chest wall involvement, mediastinal lymph nodes, transdiaphragmatic extension and small peritoneal and solid organ metastases (164-167). The performance of CT has been improved with the introduction of spiral scanners, particularly those with a configuration of 64-slice or more. The use of intravenous contrast to define vasculature enhances definition and interpretation of lesions (168).
CT scanning can define the macroscopic anatomical extent of disease, but its ability to characterise specific pleural and mediastinal lesions as benign or malignant is limited. As mentioned earlier, CT scanning can underestimate the stage of MPM because of its low sensitivity in detecting intrathoracic lymphadenopathy, occult contralateral pleural and peritoneal disease (164-166,169-171). This is important if patients are to be considered for radical treatment, but is unlikely to alter management of patients in whom radical treatment is not considered an option.
Ultrasonography is frequently used as a guide for drainage of pleural effusion and to guide percutaneous biopsy.
3.4 Assessment for multimodality and other radical therapy
Accurate staging of MPM is vitally important when surgery is considered to be part of radical (multimodality) treatment approaches.
3.4.1 Fluorodeoxyglucose-positron emission tomography (FDG-PET) staging
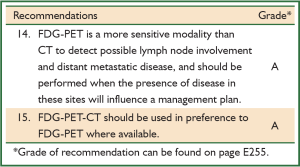
FDG-PET images tumour metabolic activity rather than anatomical location. It is more sensitive than CT in detecting nodal involvement and distant metastasis, and in differentiating tumour activity from benign disease. In comparison to CT, it both downstages some disease by excluding lesions potentially significant by CT, and upstages disease by detecting tumour in sites not detected by CT.
FDG-PET-CT should be used in preference to FDG-PET as FDG-PET-CT has demonstrated significantly better sensitivity and specificity in staging patients with stage II and III (172,173).
In patients scheduled to undergo radical surgical resection, a distinction between M0 and M1 tumours, or between T3 and T4 tumours, is critical in determining possible resectability. Two systematic reviews have addressed the staging information provided by FDG-PET in pleural mesothelioma (164,173). The use of FDG-PET to identify metastatic disease or nodal metastases may upstage or downstage patients, leading to a change of management in between 20-38% of patients (164,174). FDG-PET is more accurate in detecting occult distant metastases than anatomical imaging and identifies a higher number of mediastinal lymph node metastases than CT alone, with moderate specificity, although low sensitivity, in the detection of nodal disease (171,174). FDG-PET should be performed when the presence of distant metastases or nodal involvement will alter the management plan, for example, in those patients scheduled to undergo radical surgical procedures with the goal of long-term control of disease.
The two systematic reviews also noted that FDG-PET can distinguish benign from malignant pleural disease, with higher mean, maximum, and delayed phase Standardised Uptake Values (SUV) in malignant disease (164,173). Nevertheless, although this has the potential to provide an advantage in biopsy site selection, it remains to be determined whether FDG-PET can usefully facilitate selection of appropriate biopsy sites by evaluating areas of pleural thickening in patients who have been exposed to asbestos.
3.4.2 MRI staging
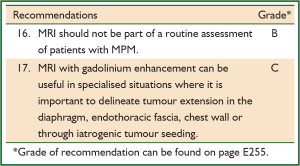
MRI inherently provides better soft tissue contrast than CT. However, the combination of high quality FDG–PET and CT surpasses MRI in staging disease prior to radical therapy (172).
For clinical staging, MRI and CT perform equivalently. In some circumstances, MRI may offer better delineation of a single focus of chest wall or diaphragm invasion because pleural malignancy enhances avidly with gadolinium-based contrast material (175).
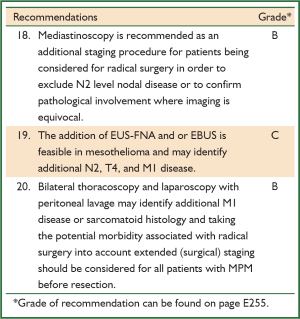
3.4.3 Surgical staging
Determining whether tumours have spread to the mediastinal or hilar lymph nodes is important when patients with mesothelioma localised to the pleura are being considered for radical surgery. The number of involved nodes (but not their anatomic location) is clearly associated with survival after EPP (176). The results of staging with FDG-PET-CT and mediastinoscopy after induction chemotherapy led to abandoning of surgical plans (EPP) in respectively 29% and14% of patients with MPM (epitheloid subtype) (177). However, both FDG-PET-CT and mediastinoscopy lack accuracy and the role of mediastinoscopy in selecting patients for EPP has been questioned on the basis of retrospective data (170). Pathological assessment of biopsy specimens may also influence the sensitivity of staging procedures as occult disease was more readily detected by immunohistochemistry (178).
Translation of images of FDG-PET-CT into T and N stages is often inconclusive and the greatest value of FDG-PET-CT seems to lie in the exclusion of patients with M1 disease from radical surgery within the context of multimodality therapy (167,171). A prospective study on the value of mediastinoscopy, VAT and laparoscopy in determining the stage of disease prior to radical (trimodality) therapy showed that these procedures were able to avoid futile thoracotomy in a significant (24%) percentage of patients (166). A retrospective review of 118 patients with MPM, who underwent extended surgical staging (laparoscopy, peritoneal lavage and mediastinoscopy) after clinical and CT evaluation revealed that 13% of patients were not accurately staged by imaging alone (179). More recent studies using endobronchial (EBUS) and esophageal (EUS) endoscopic ultrasound-guided FNA revealed that these staging procedures may also lead to more accurate assessment of disease (nodal) status (180,181).
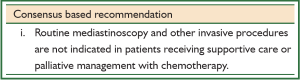
Where a patient’s treatment plan, on the basis of clinical staging, is to provide supportive care or palliative management with chemotherapy, surgical staging with mediastinoscopy or other invasive staging procedures is inappropriate.
Extended staging with mediastinoscopy, endobronchial ultrasound or trans-esophageal biopsy, thoracoscopy and laparoscopy defines an important subset of patients with unresectable MPM not identified by imaging (165,166,171,179-182). Because of the potential morbidity associated with radical surgery, extended staging should be considered for every patient selected for resection.
3.5 Assessment of prognosis
Valid and robust assessments of disease progression and survival prospects are important for many reasons:
- they help patients and families to make more appropriate decisions about treatment;
- they help patients and carers to manage important personal issues;
- they enable doctors to make appropriate management recommendations for individuals;
- they help explain variations in patient outcomes;
- they enable the stratification of patients in clinical trials.
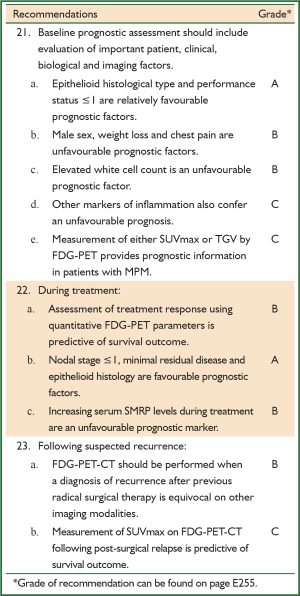
Prognostic markers for patients with mesothelioma can be divided into the following four basic categories: clinical and patient-reported prognostic markers, blood or serum prognostic markers, imaging prognostic markers and molecular prognostic markers. In addition, among patients receiving radical surgery, complete pathological assessment provides more specific tumour information for prognostic purposes.
Most studies of prognostic markers have been retrospective in design, often extending over many years, and with differences in exposures to treatment. These studies have reported male sex, older age, weight loss, appetite loss, chest pain and poor performance status to be patient factors associated with poor prognosis (72,76,183). However, in another large study, age was not found to be a prognostic factor (184), and several of these factors are downgraded or cease to be significant in multivariate predictive models. Other factors (smoking, laterality, time since diagnosis, asbestos exposure) are factors that have not consistently been shown to predict survival.
Studies of prognosis have examined disease progression and survival. No information is available on factors that predict quality of life (155). A number of prognostic factors have been used by the European Organisation for Research and Treatment of Cancer (EORTC) and the Cancer and Leukaemia Group B (CALGB) to develop prognostic scores to assist in stratification of patients in clinical trials (76,183). Their prognostic performance has been independently validated (see for example (72,161) but their role and value in routine clinical care is not determined (76,183). Performance status ≤1 and epitheloid histological type consistently indicate a relatively better survival outlook.
Inflammatory markers (white cell count, neutrophil to lymphocyte ratio (NLR), and C-reactive protein) are frequently found to be significantly elevated in different studies of prognosis in mesothelioma (185,186). Decreased haemoglobin levels, thrombocytosis and elevated serum lactate dehydrogenase (LDH) are also associated with poor prognosis (155). Elevated white cell count is a significant prognostic factor in both EORTC and CALGB studies. The value of NLR has been independently confirmed recently but needs additional prospective evaluation (186). The independent prognostic value of markers such as C-reactive protein (187) and thrombocytosis needs further validation.
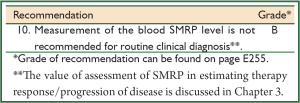
Soluble mesothelin-related peptide (SMRP) and ostepontin are among a broad range of serological or tissue markers that have been investigated for prognostic significance in MPM. High baseline SMRP serum levels are predictive of reduced mean survival in the epithelioid subtype (128,142,188,189). SMRP appears to be an indicator of tumour burden and metabolic activity. Its predictive power is removed in multivariate models which include FDG-PET (131). As serum osteopontin levels add no more prognostic information than SMRP, (189) there is no evidence to support its use as a marker of prognosis. Also other serum, tissue and molecular markers investigated in MPM (155) fail to have any proven status in assessment of prognosis or in stratification of patients in clinical trials.
Quantitative FDG-PET techniques provide prognostic information for malignant mesothelioma, however the optimal quantitative assessment method is yet to be determined (164,173). In systematic reviews, a higher SUV is associated with shorter median survival from a number of studies (164,173). Another quantitative PET parameter, total glycolytic volume (TGV), is a composite of anatomical (tumour volume) and functional (SUV, metabolic activity) data to reflect total metabolically active tumour burden (190). Higher baseline TGV is associated with shorter survival in patients scheduled to undergo chemotherapy and a prognostic nomogram using TGV has been developed but not independently validated (173,191). While this consistently suggests the potential for quantitative FDG to improve the prognostic value of clinical staging, the appropriate clinical application of prognostic information derived from FDG-PET parameters remains unclear.
3.5.1 Assessment of treatment response
Some markers of prognosis also provide information to assess response to, and prognosis after, treatment.
Two systematic reviews of the topic support the use of quantitative FDG-PET or FDG-PET-CT in the assessment of treatment response (164,173). Decreasing SUV (192) or TGV/Total lesion glycolysis (TLG) (190,193) following one, two or three cycles of chemotherapy is associated with improved survival, longer time to tumour progression, and with partial response on CT response criteria. Two studies found these associations with TGV/TLG but not with maximum SUV, suggesting that TGV/TLG quantitative techniques may be preferable in the assessment of treatment response. The optimal timing for assessment of treatment response (after cycles 1, 2 or 3) has varied between studies and is unclear.
Change in SMRP levels from baseline is also being investigated as a tool to judge response to therapy with rising SMRP indicating progressive disease. The SMRP response correlates with radiological response and TGV on FDG-PET (189).
3.5.2 Assessment of disease recurrence
FDG-PET-CT is a sensitive modality to identify suspected recurrent locoregional or metastatic disease after previous surgical management. FDG-PET-CT has been reported to have a sensitivity of 94-98%, specificity of 75-100%, and positive and negative predictive values of 95-100% and 86-88% respectively (164,194). Furthermore, at recurrence, maximum SUV is predictive of overall survival (194). FDG-PET-CT should be performed at suspected recurrence when a diagnosis of recurrence is equivocal on other imaging modalities, or where an accurate understanding of the distribution of sites of involvement by recurrent disease will change management.
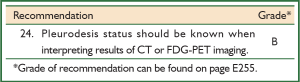
3.6 Effect of pleurodesis on staging investigations
There is limited information on the effect of talc pleurodesis on nodal staging assessed by CT scan. Similarly, there is limited information on the effect of talc pleurodesis on patterns of local and nodal uptake on FDG-PET. There has been no study assessing radiological lymph node staging pre- and post-pleurodesis.
Pleurodesis is often used to prevent recurrent pleural effusions in malignant disease. It is performed by instillation of a sclerosant such as talc into the pleural space (causing inflammation, and obliteration of the pleural space) after drainage of the pleural fluid.
In some patients with suspected malignancy such as MPM, pleurodesis may be conducted just after diagnostic biopsies at the same procedural setting to reduce the number of procedures for the patient. Most commonly, pleurodesis accompanies a VAT examination, when there is a high likelihood of malignancy. Alternatively, it can be undertaken as a separate therapeutic procedure.
In general, pleurodesis creates an intense inflammatory reaction leading to adhesions between the visceral and parietal pleura. The presence of pleural inflammation may alter assessment of disease stage or extent of disease, likely through increased pleural uptake on an FDG–PET scan and/or inflammatory adenopathy.
Inflammatory processes give false positive results on FDG-PET due to increased macrophage uptake and retention of labelled FDG, but there is limited data specific to MPM.
One study suggested that talc pleurodesis did not affect T4 or N2 staging, but conversely found FDG-PET-CT to be inaccurate compared to subsequent surgical staging (171). In another study, it was suggested that talc did not adversely influence the development of a prognostic model based on FDG-PET TGV and that an increase in TGV in patients with prior pleurodesis could be quantitated and corrected for in the prognostic nomogram (191).
3.7 Pre-treatment evaluation
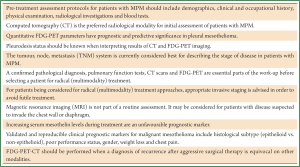
An optimal pre-treatment assessment protocol for patients diagnosed with malignant mesothelioma should be simple and widely applicable, sequential and logical, with limited invasive procedures. Patients should be assessed individually for suitability and preferences for potential treatment plans. Specific staging evaluations where radical treatment is being considered are recommended (see above). Otherwise, relatively limited higher level data exists for this population in terms of evaluation after diagnosis. Of relevance is the 2010 Guidelines of the European Respiratory Society and the European Society of Thoracic Surgeons for the management of malignant pleural mesothelioma (21) which followed on from the consensus report from van Meerbeeck in 2005 before PET scans became generally available (195).
These guidelines suggest that for all patients who present or are diagnosed with MPM, routine clinical history including demographic and clinical symptoms and signs, performance status and physiology such as weight loss, chest radiographs and simple blood investigations should be considered. Assessment of asbestos exposure should also be conducted and recorded for each patient at presentation.
According to these guidelines, all patients at diagnosis should be assessed as follows:
- demographics: sex and age;
- social history in so much as it may influence treatment choices and access;
- clinical and occupational history (asbestos exposure): performance status, co-morbidities, presence/absence of chest pain, dyspnoea, change in body weight or body mass index, medication requirements;
- physical examination: presence or absence of shrinking hemithorax, presence of evidence of metastatic disease or direct extension of tumour (cutaneous nodules etc.);
- radiological investigations: plain chest X-ray;
- blood tests: haemoglobin, leucocytes, platelets, and basic biochemistry (renal and hepatic function and LDH).
In addition, patients likely to receive some form of active treatment should have:
- histological confirmation with an adequate biopsy;
- CT scan of chest and upper abdomen with intravenous contrast after drainage of pleural fluid (if drainage required for symptom control);
- pulmonary function testing;
- measurement of SMRP as a guide to determining response to therapy.
The selected group of patients thought to be candidates for multimodality therapy or other radical (surgical) therapy, in addition to (surgical) staging assessment, should also have routine pulmonary and cardiac function tests as indicated for patients undergoing thoracotomy.
4 Active anti-cancer treatment
Key messages
4.1 Introduction
MPM is purportedly resistant to treatment with classic anti-cancer treatments (surgery, chemotherapy and radiotherapy). Some recent progress has been made with prescribing combination chemotherapy regimens and treating patients with multimodal treatment, which involves various combinations of chemotherapy, surgery and radiotherapy. However, median overall survival for patients with malignant mesothelioma has remained modest (around seven months) as shown in recent population based updates (196,197).
4.2 Chemotherapy
Chemotherapy for MPM has been the subject of many phase II trials (198-200). Objective radiological response rates greater than 15% (based on a variety of tumour measurement criteria) have been reported for single drug therapy with various drugs including pemetrexed, raltitrexed, gemcitabine, platinum based drugs, vinorelbine and several anthracyclines (such as doxorubicin).
4.2.1 Combination chemotherapy
Combination treatment usually produces higher response rates than single drug therapy. There are few direct randomised comparisons of single versus combination drugs. One three-armed study, which compared the efficacy of combined chemotherapy with a single agent and a placebo in malignant mesothelioma, did not show significant differences in survival between the combined chemotherapy and supportive care arms, although a trend in favour of the single-agent arm (vinorelbine) was observed (201). It was prematurely stopped because of low recruitment and required both chemotherapy arms to be combined for analysis. This study has been criticised mainly because the combination chemotherapy (Mitomycin C, Vinblastine, Cisplatin) (MVP) is considered inadequate and the final study had insufficient power to address the effect of vinorelbine alone.
Two randomised studies have shown that combination chemotherapy that includes cisplatin and pemetrexed or raltitrexed is associated with increased survival (195,202). The median overall survival of patients given cisplatin—pemetrexed (12.1 months) or cisplatin—raltitrexed (11.4 months) was significantly longer than that of patients receiving cisplatin alone (9.3 and 8.8 months respectively), providing direct evidence that combination treatment has a beneficial effect. A large compassionate-use study of cisplatin or carboplatin in combination with pemetrexed suggests indirectly that carboplatin and cisplatin have similar efficacy (203).
Therefore, pemetrexed in combination with a platinum agent (cisplatin or carboplatin) is currently regarded as the optimal chemotherapy treatment for patients with malignant mesothelioma (204). Raltitrexed is an active alternative; however, this drug is neither approved nor reimbursed for this indication in Australia.
4.2.2 Number of chemotherapy cycles and timing
The optimal number of cycles of chemotherapy has not been defined. For patients with good performance status, and adequate organ function, a commonly used standard for first-line treatment in stable or non-progressing patients is a maximum of six cycles of pemetrexed (500 mg/m2) as a 10-minute intravenous infusion followed by cisplatin (75 mg/m2) over two hours on day one of a 21-day cycle. This was the de facto standard in the randomised clinical trial (202).
A small, underpowered randomised study which used the MVP regime, shown to lack activity in a larger study, suggested that giving MVP earlier rather than later was associated with an extended period of symptom control (205). This is the only study available on the optimal time to start chemotherapy in patients with malignant mesothelioma. Theoretically, chemotherapy is more effective at treating patients with a good performance status and small tumour volumes. Studies in patients with other types of cancer show that treatment results are superior for patients with these characteristics. However, for malignant mesothelioma convincing data is lacking.
A small non-randomised study showed that pemetrexed maintenance therapy is well tolerated (206). The role of maintenance therapy has not been prospectively evaluated although there is currently an ongoing US randomised phase II trial evaluating the role of maintenance pemetrexed in patients with stable disease after first-line chemotherapy. Second-line pemetrexed combined with best supportive care (BSC) elicited significant tumour response and delayed disease progression, compared with BSC alone, in selected patients with mesothelioma who had not previously received pemetrexed as part of first-line therapy (207). Additionally second-line pemetrexed was more likely to yield clinical benefit among patients who responded to first-line therapy. Retreatment with pemetrexed based chemotherapy has been noted as a treatment option for patients with durable responses from pemetrexed based therapy, but more studies are needed to further define the place of second-line therapy in malignant mesothelioma (208,209).
4.2.3 Targeted therapies
Deregulated expression of growth factors or proteins involved in downstream signaling pathways has been shown to play an important role in malignant transformation of mesothelial cells. Molecular studies in malignant mesothelioma have confirmed that growth factors such as vascular endothelial growth factor (VEGF), platelet-derived growth factor receptor beta (PDGFR beta) and the epidermal growth factor receptor family are frequently activated. Several phase I/II studies have tried to exploit these specific characteristics, but none of the early clinical studies using targeted therapy have shown convincing activity (210). Notwithstanding these negative results, it is expected that the rapidly increasing insight into the biology of mesothelioma will ultimately assist in developing therapies that progress beyond the existing therapeutic plateau.
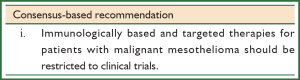
4.3 Immunologically based therapies
The existence of a relatively specific immunologic response (mesothelin antibodies) in mesothelioma patients, the observation of spontaneous regression of disease and the finding that tumour tissue of mesothelioma patients is sometimes highly infiltrated by immune cells, have raised significant interest in the potential of immunotherapy in malignant mesothelioma (211-213). Early clinical studies including trials with anti-mesothelin monoclonal antibodies and gene delivery strategies are ongoing (214-216). So far trials with immunologically based therapies (immunomodulating agents and vaccines) have not yet been shown to improve the survival of patients with mesothelioma and it is clear that immunology based treatment approaches should be restricted to clinical trials.
4.4 Surgery
Surgery for MPM may include relatively minor procedures for diagnosis, staging and pleurodesis (see also Chapter 5.4), more involved debulking operations for palliation and extensive cytoreductive procedures where the goal is to lengthen survival by reducing intrathoracic tumour burden to microscopic levels (32).
4.4.1 Thoracoscopy
One of the central aims in the management of patients with symptomatic pleural effusions caused by malignant mesothelioma is to achieve an early and successful pleurodesis (42). This helps symptom control and a ‘trapped lung’ is less likely to occur if the procedure is performed promptly. Given the relatively low diagnostic yield of bedside procedures, early thoracoscopy also gives the opportunity to obtain a definitive histological diagnosis. A prospective study in 25 patients suspected of having mesothelioma and in whom other diagnostic methods failed, confirmed that VAT is an extremely useful technique; it combines a high diagnostic yield with an effective way to prevent recurrent collection of fluid in the diseased hemithorax (217). Two major review articles revealed that complications of VAT are uncommon (218,219). Space infection and subcutaneous emphysema were the most frequent complications.
4.4.2 Pleurectomy/decortication (P/D)
There is a variation among surgeons with respect to what is involved in P/D by open thoracotomy or closed VAT surgery (VATS) (32). For some mesothelioma surgeons, P/D refers to a surgical procedure that aims to remove all macroscopic tumour from the affected hemithorax; others refer to this extensive procedure as a ‘radical P/D’ for resection of only the parietal and visceral pleura. Still others use the term P/D to describe a palliative procedure where the intention is debulking of tumour to ameliorate pain and pleural effusion and to improve respiratory mechanics (220).
Debulking pleurectomy with palliative intent is the more common procedure because most patients with mesothelioma will be unsuitable for a procedure with radical intent. It is not known whether debulking surgery enhances the efficacy of postoperative chemotherapy and/or radiotherapy. One observational VATS pleurectomy study suggested that this procedure might be associated with prolonged survival when compared to treatment without P/D, but this has not been tested in a randomised study (221).
4.4.3 Extrapleural pneumonectomy (EPP)
EPP aims to remove all macroscopic tumour from the chest by resecting the pleura, lung, pericardium, diaphragm and regional lymph nodes. Its development and adoption as a more aggressive surgical approach has elicited an intensive debate among the specialists involved in the treatment of MPM. It is generally assumed that EPP allows better macroscopic tumour clearance, and this procedure has been accepted as the debulking procedure of choice for early stage mesothelioma in a number of specialised centres in the North America, Europe and Australia (222-224).
A recent review, aiming to compare the published results after EPP with palliative treatment approaches, noted the extension of survival achieved with EPP in patients with epithelioid histology and limited nodal spread, but pointed to the high perioperative and 30-day mortality and morbidity rate of EPP (225). The experience of the thoracic surgical team is probably the most critical factor in obtaining optimal results in radical debulking approaches. In a large Australian single-institution cohort study involving 540 patients undergoing surgery for malignant mesothelioma, the experience of the surgeon (performed more than 100 radical mesothelioma operations) was one of three factors associated with improved survival. This is consistent with other studies showing the importance of patient volume in relation to complication rates and survival following lung and other cancer surgery (226,227).
Early evaluation of EPP (228) comparing patients undergoing EPP with those considered not candidates for EPP failed to demonstrate an overall survival benefit, though recurrence free survival was significantly improved (229). More recent studies have evaluated EPP as part of trimodality therapy (TMT).
Several prognostic and treatment features have been identified which compromise the goal of minimising or eliminating residual disease through debulking surgery and increasing the risk of progressive disease. These include mediastinal nodal or metastatic disease, and non-epitheliod histology (230), and persistence of mesothelioma in resection margins (231). Hence, a radical approach with EPP is unsuitable for most patients with mesothelioma.
4.5 Multimodality therapy (surgery, chemotherapy and radiotherapy)
4.5.1 Trimodality therapy (TMT)
It is virtually impossible to resect the pleura with an adequate margin that is microscopically negative in all directions. Treatment strategies have therefore been developed to consolidate local control from surgery with radiotherapy, and extend these gains with the addition of chemotherapy. Other local therapies [photodynamic therapy (PDT), hyperthermic lavage etc.] have also been employed.
TMT refers to a multimodality treatment strategy or intent that combines chemotherapy, with EPP, and radiotherapy (232). Typically the chemotherapy is administered as induction treatment followed by surgery and then by hemithoracic radiotherapy. The treatment course extends over a timeframe (of six months or more) and completion rates of 60% or more are achievable (233).
Evidence supporting TMT is derived from retrospective and prospective observational studies. Although longer median survival has been achieved in the more recent studies employing induction chemotherapy (234), no randomised or other controlled comparisons have been conducted to enable the contribution of sequencing, patient selection and drug regimen to be assessed.
In almost all of these studies the use of TMT was guided by prognostic factors such as extent of disease, the patient’s performance status, histological subtype and the absence of significant co-morbidities. Patients with good performance status, low volume disease and epithelioid histology were the most likely to benefit from multimodality therapy (235,236). When disease progressed despite induction chemotherapy subsequent, EPP was generally withheld. The treatment team involved in TMT must be experienced and able to carefully weigh up prognostic factors and co-morbidities (42).
The contribution of extensive cytoreductive surgery in the trimodality regimen has been questioned. A feasibility study for a randomised controlled trial undertaken in the UK to compare EPP (within a multimodality protocol) with no EPP failed to demonstrate that EPP offers additional benefit over induction chemotherapy and postoperative radiation therapy (237). The study experienced a large number of protocol deviations and EPP was associated with a high rate of postoperative mortality (18%). Hence the author’s interpretation of the results has been criticised (238). However, investigators from Western Australia were also unable to demonstrate a survival benefit for EPP, when reviewing prospectively collected data from a series of 36 patients referred for TMT (239).
4.5.2 Comparison of P/D and EPP
EPP has been the cytoreductive procedure employed in most studies of multimodality therapy. The only studies comparing survival outcomes between P/D and EPP as debulking procedures in multimodality treatment are descriptive case series. Although an Australian study associated EPP with a better median survival than P/D, other studies concluded that the type of debulking procedure either had no influence on survival (75,240,241), or favoured P/D (240,242,243). In the absence of adequately controlled trials it is impossible to be sure of the relative survival benefits of one radical procedure over another (radical P/D vs. EPP). Observed differences are as likely to be due to differences in prognostic factors, case selection as well as differences in the measurement of survival.
In observational studies, P/D and EPP differ in relation to other outcomes. EPP generally achieves a greater degree of local control (240). Relapse after P/D is more likely to be in the thorax and the terminal course of disease more likely to feature respiratory symptoms; whereas distant relapse is a more prominent feature of EPP (229,240,244). However, EPP also confers a higher postoperative mortality risk.
4.5.3 Role of chemotherapy and radiotherapy within multimodality treatment
Induction or the adjuvant therapy approach for malignant mesothelioma has not been tested in a randomised study and the relative contribution of chemotherapy and/or radiotherapy given before or after radical debulking surgery is largely unknown. On the other hand, there are observations that platinum plus pemetrexed chemotherapy is occasionally able to induce a complete pathologic response (245) and that the addition of chemotherapy and/or radiotherapy to radical surgery is associated with more favourable outcomes (222). Retrospective studies consistently show that patients with epithelioid tumours receiving combined modality therapy have better outcomes than patients with sarcomatoid or biphasic tumours (246,247). Moreover, it is noteworthy that the choice for adjuvant radiotherapy is influenced by the type of radical surgical procedure (240).
It is generally assumed that disease progression during or shortly after induction chemotherapy is a sign of poor prognosis and that patients failing on induction chemotherapy should not undergo radical surgical procedures and that futile treatment should be avoided (245). Those patients who do respond to induction chemotherapy should be reviewed and assessed, in terms of their physical fitness, for radical surgery and postoperative radiotherapy.
4.6 Radiotherapy
Radiotherapy is widely used in the treatment of patients with malignant mesothelioma. It is used for palliation of symptoms such as pain, for port-site prophylaxis and is considered an integral part of multimodality therapy for early stage disease where it may prevent local relapses after surgical resection. A review of the evidence supporting the use of radiotherapy in patients with malignant mesothelioma was published in 2011 (248).
4.6.1 Palliative radiotherapy
Most publications on palliation of symptoms are retrospective descriptions of single centre practice. One retrospective report described 19 patients who received radiotherapy for dyspnoea, dysphagia, superior vena cava obstruction and brain metastases, with substantial relief of symptoms with radiotherapy doses of more than 40 Gy (249). A retrospective study from Melbourne reviewing a five-year experience reported that 65% of 26 courses of palliative radiotherapy were at least partly successful (250). A clear dose-response effect was not evident in the subsequent expansion of this study (251). Retrospective data from the Netherlands revealed that the palliative effect of radiotherapy was of relatively short duration and a review of 227 radiotherapy courses in 189 patients over a long period showed that responses were more common with fractions of 4 Gy or greater (252). A recent study from the UK of 54 patients given a dose of 36 Gy in 12 fractions using modern radiotherapy technologies, and with follow-up CT scans, found a 54% response for relief of chest pain. The authors concluded that palliative radiotherapy is able to induce a response rate in patients with malignant mesothelioma comparable to that of contemporary chemotherapy (253).
Effective palliation may prolong life but the review by Price (248) and previous systematic reviews have not found evidence that radiotherapy is able to prolong survival in patients with malignant mesothelioma (254-256). Radiation doses of 40 Gy or greater are more likely to provide long-term benefits (249,252,257,258) than lower doses. Chest wall pain and symptoms from spinal cord compression and superior vena cava obstruction are relieved in 60% of cases. Radiation toxicity at this dose is rare but higher doses and large field require techniques that spare normal tissues in and adjacent to the thorax.
4.6.2 Radiotherapy as a component of radical treatment
The use of hemithoracic radiotherapy is influenced by the anatomy of the pleura and it is challenging for the radiation oncologist to appropriately include all viable disease in the radiation volume. Moreover, the presence of vital structures – lung, liver, spinal cord and heart—makes it difficult to administer appropriate doses without causing side effects. The first experiences with high doses of radiotherapy to the full hemithorax after pleurectomy were not favourable, as significant deterioration of pulmonary function and significant radiographic changes of the remaining lung were noted several months after the radiation treatment (168,259).
Postoperative radiotherapy after EPP was part of a protocol that was used in one of the first trimodality studies (232). The technique was based on a photon and electron beam combination that was developed at the Memorial Sloan-Kettering Cancer Centre in 1987 (260), where a review of failures found a pattern of local recurrences frequently occurred in regions of dose heterogeneity at junctional sites (261). Another US single arm study suggested that hemithoracic radiotherapy was associated with a reduction in local failure, which was not statistically significant (262). Unfortunately no evidence from randomised studies is available to assess the weight of individual modalities in prolonging survival and it is important to note that any potential benefit of radical radiotherapy for malignant mesothelioma must be weighed up against the risk of radiation toxicity to the contralateral lung and other critical tissues.
Further attempts at improving local control with radiotherapy after EPP have focused on intensity-modulated radiotherapy (IMRT). Local control at 13 months with minimal toxicity was reported in a group of patients (182,263). A subsequent report in 2007 included 63 patients, and found recurrences within the irradiated volumes of only 5%. Distant recurrences were seen in 54% and median survival was 14 months (182). However, additional observations showed that IMRT was associated with significant toxicity (radiation pneumonitis) that was fatal in some cases (264-266). The authors suggested this was related to higher radiation doses received by the remaining lung. Following these reports several groups recommended more rigorous constraints for beam distribution and prescribed dose (264,267,268). More data is needed to show that the attempts at improving the results of IMRT are effective and that better local control can be obtained, as suggested by some authors (182,269,270). One randomised Swiss study is focusing on IMRT after EPP and the accrual of this important trial (234) should be completed soon. Although IMRT has been referred to as the preferred technique by US centres with experience in hemithoracic irradiation (269), IMRT cannot be advocated outside strict protocols.
The National Comprehensive Cancer Network has recently published practice guidelines with recommended doses for conventional fractionated radiation therapy in mesothelioma (271):
4.6.3 Prophylactic radiotherapy (port-site prophylaxis)
Mesothelioma cell seeding, which manifests as subcutaneous nodules, has been reported in several series of patients, ranging from 2-51%. The occurrence of subcutaneous nodules is more frequent in patients with mesothelioma than in patients with other cancers. These nodules can occur adjacent to intervention tracts that target the pleura, such as sites of percutaneous needle biopsies. However, they are only problematic in a minority of patients.
It is noteworthy that subcutaneous nodules are not well characterised in terms of timing following intervention, depth below the skin surface, extent of subcutaneous pleural extension, mesothelioma stage or subtyping. In 1995 a retrospective study noted that radiotherapy was effective in preventing tumour seeding following thoracoscopy (272). Many centres have used radiotherapy as the primary modality to prevent the local problems elicited by subcutaneous tumour growth (273).
Two systematic reviews of three randomised and nine non-randomised trials concluded that the use of prophylactic radiotherapy in thoracic intervention sites to prevent subcutaneous nodules was not justified and had no significant effect on overall survival (274,275). The three randomised studies were underpowered and showed variations in the timing, dose/field size, fractionation of radiotherapy and follow-up (276-278). The weight of evidence does not support a local control benefit of prophylactic radiotherapy following simple thoracic intervention that justifies its use.
So far, prophylactic radiotherapy has been unable to significantly alter the disease course and cannot be recommended for mesothelioma patients following pleural intervention (248,255,256,275,279).
Thus there is no high level evidence to support the routine role of radiotherapy in patients with MPM. Prospective studies and randomised trials are required to provide a solid basis for radiotherapy in this malignancy.
5 Palliative and supportive care
Key messages
5.1 Introduction
Palliative and supportive care involves healthcare practices, including treatments, intended to optimise a patient’s overall wellbeing, comfort and functional status. They play a key role in the management of pain and other symptoms, and in the provision of practical and emotional support for patients with malignant mesothelioma, their carers and their families (280).
MPM usually presents as advanced disease and the most commonly reported physical symptoms are (42,281):
- dyspnoea due to pleural effusion (in early stages) or lung encasement by pleural thickening (in later stages);
- fatigue;
- chest pain due to parietal pleural irritation and/or compression or invasion of the intercostal nerves by tumour invading the chest wall;
- weight loss;
- insomnia;
- ough (a less prominent symptom) (281,282).
Effective alleviation of these symptoms often requires a multidisciplinary approach.
Research evidence about palliative treatments specific to mesothelioma patients and their carers is sparse. Likewise, only a limited number of articles have been published about psychosocial and supportive care issues of patients with mesothelioma and their families, the majority of which produce low level evidence.
The paucity of literature addressing these issues is most likely due to a combination of disease related factors, including poor prognosis, as well as the relatively low number of diagnosed cases. As a result, psychosocial and supportive care is often based on practices generally formulated for patients with other illnesses such as lung cancer and chronic obstructive pulmonary disease. However, there is increasing awareness that individuals diagnosed with mesothelioma form a distinct patient group with unique and often complex physical and psychosocial needs.
5.2 Symptom management and control
Quality of life studies have revealed that patients with malignant mesothelioma have a high symptom burden (281). The scores for fatigue, dyspnoea, pain, insomnia, cough and anorexia in malignant mesothelioma studies exceeded scores seen in lung cancer studies. Palliative care has traditionally been delivered late in the course of disease to patients with uncontrolled symptoms (283). It has been suggested that late referrals to palliative care are a barrier to providing the quality of care required for people with advancing cancer. A recent randomised study comparing non-small cell lung cancer patients, who received early palliative care or standard (late) palliative care showed that early palliative care led to significant improvement in both quality of life and survival (284,285). It seems reasonable to apply these outcomes to patients diagnosed with MPM. They will also require palliative and supportive treatment from the time of diagnosis, or ideally even before the establishment of a definitive diagnosis for symptomatic patients.
5.3 Assessment, treatment and control of pain
Pain assessment and control in patients with MPM should follow the principles of cancer pain management (286). Pain in patients with MPM can be complex in nature (287) and may require extra measures. The pain is usually dull and diffuse but may also be pleuritic as a consequence of the direct effects of invasion on the parietal pleura. Bone pain and neuropathic pain from compression/invasion of intercostal nerves/ribs may also occur. A specialist in palliative pain medicine should be involved early in case of refractory or unresponsive pain. Occasionally neuroablative techniques may be required, depending on specialist advice and with careful consideration of risks and benefits (288,289).
Effective pain relief has been reported in more than half of the mesothelioma patients treated with palliative radiotherapy (see section 4.6). There is no direct evidence to support whether early intervention with radiotherapy and local pain techniques offers advantages over systemic therapy (chemotherapy).
5.4 Management of dyspnoea
Dyspnoea is a relatively common and frequently distressing symptom of patients with MPM and often worsens as the disease progresses. The management of dyspnoea includes:
- treating reversible causes contributing to dyspnoea—this includes drainage of substantial pleural effusions and treatment of arrhythmias or anaemia;
- regular use of oral low dose, sustained release morphine safely reduces the intensity of breathlessness (290-292);
- non-pharmacological techniques (293).
When dyspnoea is caused by accumulation of pleural fluid, aspiration is needed, followed by pleurodesis at first relapse (21,42). Pleurodesis is useful in preventing recurrent pleural effusions and sterile talc powder is preferred to other sclerosing agents. Recurrent pleural effusions become more difficult to drain and indwelling pleural catheters may be the most practical way to manage recurrent pleural effusion (21,294,295).
Oxygen can be beneficial when a patient is hypoxaemic; otherwise it is unlikely to be any more beneficial than use of a fan or medical air (296,297). In many patients a simple fan with a cool stream of air flowing across the face can help to reduce the sensation of dyspnoea (298).
5.5 Symptom control
Fatigue, weight loss, insomnia and cough are other symptoms frequently observed in patients with MPM. There are no data on the efficacy of specific interventions for these symptoms, but it seems reasonable to consider amelioration of insomnia and cough with medication. Many patients with MPM present with anorexia and weight loss and it is known from other groups of cancer patients that nutrition screening and intervention is associated with a better nutritional status and quality of life while undergoing disease-modifying treatment (299).
Chemotherapy may also ameliorate the symptoms of MPM as was shown in the two international studies investigating the addition of pemetrexed or raltitrexed to cisplatin (195,202). Symptoms such as shortness of breath were positively influenced by combination chemotherapy and are most likely related to tumour response (see section 4.2) (300).
5.6 Psychosocial needs of patients
5.6.1 Information and communication needs
Patients diagnosed with malignant mesothelioma and their carers require clear communication and tailored, accurate information from health professionals about diagnosis, prognosis, treatment options and end of life issues. There is a modest amount of evidence to suggest that adequate information is lacking in some domains.
In a UK survey of 83 patients by the British Lung Foundation, over 80% of patients reported receiving information about treatment options, welfare benefits and compensation; a lower proportion of patients received information about where to go for further advice, including out of hours support (62%) and how to control symptoms (53%). Even fewer received information about end of life issues and palliative care (25%) (301). In a qualitative Australian study of 13 people including two patients and six carers (302), results indicated that it was difficult to obtain reliable and accurate information relating to the disease. When information was not provided by their health professionals, internet searches resulted in negative or pessimistic information. Respondents also reported that patients were referred to palliative care too late into their cancer experience (302).
It is important that patients and carers are given the right information at the right time. In a small qualitative study of five patients with malignant mesothelioma, patients reported not being provided with the right information and support at the right time. They were unable to take in information due to the shock of the diagnosis and the overwhelming amounts of information being provided (303). These findings were echoed in a UK study of 15 patients, who recalled receiving a ‘hopeless message’ of incurable disease with no effective treatments sympathetically delivered by doctors. Issues relating to communication causing distress were reported to continue over the illness trajectory (304).
The Clinical Practice Guidelines for the Psychosocial Care of Adults with Cancer provide a detailed description of the specific types of information people with cancer require about diagnosis, prognosis, treatment options, preparation for threatening procedures and the transition to palliative care (305). Since the publication of these guidelines, updated Australian communication recommendations have been developed on the transition to palliative care (306), discussing complementary therapy use (307), and on ‘end of life’ discussions and responding to desire to die statements (308). However, there is no evidence yet to demonstrate that improved communication skills translate into superior patient outcomes (309-311).
5.6.2 Emotional needs
A small number of studies have been conducted on the emotional state of people with MPM. Not surprisingly, fear of death is the dominant recurring emotion (301,302,312). Table 4 presents results from the British Lung Foundation survey (301), and shows that a majority of patients and their carers reported negative feelings.
Similarly, in a sample of 49 Australian men diagnosed with malignant mesothelioma following occupational exposure to asbestos, 94% were afraid they were going to die from the illness and 43% worried about this on a daily basis (312). People living within communities that have been exposed to asbestos describe the immense fear they experience that every respiratory symptom might indicate that they had developed malignant mesothelioma when those around them, including workmates and friends, had died from this disease (302). Many patients with malignant mesothelioma reported that symptoms linked to the disease caused anxiety, particularly dyspnoea (304) which was associated with high anxiety and fear of impending death. Struggling to breathe was reported to be deeply distressing to both the patient and family.
A core element of good palliative and supportive care is the identification of, and assistance with, various sources of social and psychological stress. In the British Lung Foundation survey, less than half of the patients (47%) reported that health professionals had provided support in relation to ‘discussion about their psychological needs and hopes and fears for the future’. Healthcare providers need to be adept at eliciting and responding to emotional cues, conducting systematic assessments of patients’ needs and providing or arranging for appropriate multidisciplinary referrals including counseling to patients and their families (313).
5.6.3 Daily living and social needs
There is a high symptom burden associated with MPM. The most commonly reported symptoms—dyspnoea, pain, fatigue and appetite loss—are significant predictors of a patient’s quality of life and ability to conduct daily activities, such as showering and dressing (300).
These physical symptoms also have an impact on the patient’s social identity, for example, when they are no longer able to maintain employment (303). In a comparison between patients with MPM and reference data from patients with non-small cell lung cancer, Nowak and colleagues (281) found that those with MPM had comparatively lower role and social function despite having better physical function. Physical symptoms can have a marked impact on a person’s social functioning by causing changes in identity, roles and relationships, feelings of worthlessness and social isolation (314).
5.7 Psychosocial needs of carers and families
A patient’s community of family and friends often undertake care-giving roles. Accepting these roles has implications for the physical and psychological wellbeing of carers and despite this burden, carers receive inadequate information and support from the health system (314).
The British Lung Foundation survey (301) suggested that more carers were experiencing negative emotions than patients (see Table 4).
In addition, 62% of carers reported that they had received information about how to control symptoms; 47% felt that health professional support had been provided for family and carers; and 62% received information on palliative care and end of life issues, while only 20% had received information about the needs of dependents. Carers also appeared to be less satisfied than patients with the support they received from health professionals (301).
In other studies, carers reported feeling burdened and fatigued (302,303). Some carers, many of whom are women, felt particularly burdened by the additional care-giving roles for ageing parents, young children or grandchildren (302). As the disease progresses, there is a high likelihood that changes in roles within a household occur with both parties finding these changes difficult (303). The physical impact of MPM on a patient can also adversely affect intimate relations with their partner and family members (303). In one small study, carers reported non-professional support, such as talking with friends about their experiences, as valuable (302).
While the evidence is scant, findings suggest that carers of people with malignant mesothelioma have high levels of psychological distress and fatigue, and receive inadequate support, information and guidance from health professionals (314).
5.8 Psychosocial interventions
Only one study which evaluated an intervention was identified (315). A post-intervention survey of patients who attended a diagnostic clinic run by specialist nurses was conducted, with 18 of 26 participants returning questionnaires. The clinic had longer appointment times (45 min as opposed to 20 min), greater patient focus and paid particular attention to a patient’s emotional responses to the diagnosis. The nurses had experience in managing patients with mesothelioma, received training in advanced communication skills and tailored information to the specific needs of the patient. The study found that 67% of patients understood their diagnosis and 89% believed their diagnosis had been communicated sensitively. The vast majority also reported that they had an opportunity to ask questions, talk about worries or concerns, were offered written information, and given the contact number of the specialist nurse.
Support groups are another potential form of intervention to help people with malignant mesothelioma and their carers. A UK team established a support group program which consisted of 15 one monthly sessions of two hours with half the sessions involving invited speakers, and the other half, facilitated discussions. The evaluation involved only four patients and two carers (30% response rate) but all of the respondents said they found the group useful (316). Similarly, two qualitative studies reported that both patients and carers found support groups to be helpful because they offered an opportunity to talk to others in a similar situation (302,303).
Mechanisms are required to assist patients and carers in daily living needs and the management of progressive symptoms, particularly towards the end of life. In an opinion piece, Hawley and Monk contend that many patients with MPM die in hospital despite their wishes to die at home and the reasons for this are the rapid disease progression and burden of care. They made three recommendations to assist patients to die at home:
earlier referral to specialist palliative care;
provision of community nursing and other support services;
provision of education for caregivers about preparing for end of life care (317);
Other experts endorse early referral to palliative care to manage not only the physical symptoms but also psychological distress (318,319). Chapman and colleagues believe that a combined psychological and pharmacological intervention delivered in a palliative care setting is particularly effective for pain management (319).
5.9 Legal compensation issues
Because malignant mesothelioma frequently results from exposure to asbestos, patients who have a history of exposure to asbestos may be eligible for legal compensation. Compensation claims frequently occur while the patient and family members are trying to deal with the diagnosis and treatment of an incurable disease and to cope with progressive symptoms and impending death. The avenues for compensation vary between States.
Based on a retrospective account from 38 workers diagnosed with malignant mesothelioma, less than 10 % were told by a professional source of their increased risk of developing mesothelioma prior to diagnosis. Most workers (83%) stated they were not aware of any increased risk of developing the disease (320). A more recent Australian report found that people involved in industry using asbestos felt that employers had not taken the threat seriously early on and deliberately kept workers ignorant of the risks associated with asbestos (302).
Making a claim for compensation is often expressed by patients and their carers as stressful and burdensome. The time consuming and complex medico-legal procedures involved in claiming compensation may provide for the family financially, but also impact negatively. Patients and carers both reported the legal process to be a seemingly endless burden which limited the time patients and their families had left to spend together, placing further strain on relationships (303,304). Some patients reported that they could not provide sufficient proof for a successful claim causing anger and distress (303). It is important to be aware that patients who have malignant mesothelioma may be experiencing additional stress related to legal processes. These patients and families may require additional psychosocial support.
5.10 Complementary or alternative therapies
Depending upon how complementary or alternative medicine (CAM) is defined, estimates of its use in cancer patients range from 7% to 64% (321). A more recent Australian study suggests that 17% of cancer patients use at least one form of CAM (322) but most oncology health professionals have difficulty discussing CAM use with their patients (323,324).There is no specific research on the use of complementary or alternate therapies by people diagnosed with malignant mesothelioma, or on whether health professionals support the use of these therapies for their patients.
Australian guidelines on discussing complementary and alternative therapies recommend that doctors ask and listen to patients about whether they are using these therapies, discuss relevant concerns while respecting a person’s beliefs, and then provide balanced, evidence-based advice relating to their use (307).
5.11 Nutritional assessment and exercise programs
There is no evidence relating to nutritional assessment or exercise programs and survival and/or quality of life in patients with malignant mesothelioma.
6 Models of care
Key messages
6.1 Introduction
Models of care are developed to ensure that best practice guides patient care. They also assist in providing reliable and equitable health services that aim to meet the health needs of the community and respond to the changing needs of the current health care system.
Information about health care services and models of care for people with MPM and their families is very limited. Consequently, publications about the care of people with lung cancer and other cancers such as breast and prostate cancer are drawn upon in modelling care for patients with MPM.
Although medical interventions cannot cure mesothelioma, medical teams can provide treatment which aims to minimise symptoms, improve quality of life and prolong life. Medical teams also provide much needed support and information to the patient and their family.
6.2 The MDT and care of malignant pleural mesothelioma
The management of cancer patients has become a multidisciplinary and often multimodal process requiring the involvement of many specialised health professionals. The key to providing optimal care for patients is effective coordination of specialised care and services. This is best provided by a MDT ensuring multidisciplinary care. There is no direct high level evidence to confirm that management by an MDT improves survival, symptoms or quality of life for patients with MPM, due to a lack of appropriate studies conducted in relation to this relatively uncommon disease. However, anecdotal reports suggest that patients are more likely to receive optimal care if a consistent approach to managing their disease is taken, with better symptom management and improved quality of life.
An MDT consists of healthcare professionals who, through an integrated approach, develop an individual patient treatment plan. The composition of a MDT will vary by disease site and institution, but in the setting of MPM the team should include representatives from medical oncology, radiation oncology, cardiothoracic surgery, respiratory medicine, pathology, diagnostic imaging, palliative care, nursing, nutrition, dietetics, psychology and social work (325). For practical reasons, and depending on the institution, it may not be feasible to have all members of an MDT in attendance at a multidisciplinary meeting at the same time. The MDT should also work closely with the patient’s GP and other allied health professionals.
The MDT is involved in managing the patient and carer(s) throughout treatment to ensure they obtain the most appropriate care for their clinical situation. In order to control disease progression, relieve symptoms and optimise quality of life, patients will move from one type of care to another as their clinical situation changes. Patients with MPM are currently managed by, and receive information from, lung cancer multidisciplinary care teams. Ideally, this team should include specialists experienced in treating MPM.
Members of the MDT work collaboratively to provide multidisciplinary care. They discuss diagnostic and treatment options specific to each individual patient, and provide diverse subspecialty input into patient management, including facilitating rapid diagnosis and the establishment of treatment protocols. These issues are of particular importance for patients with mesothelioma because of the progressive symptom burden of this disease and the potential legal compensation implications of the diagnosis.
One of the goals of multidisciplinary care is to ensure that the time between presentation of symptoms to diagnosis and treatment is as short as possible. This requires timely referrals to appropriate experts. A number of studies related to multidisciplinary care in lung cancer patients have focused on the timeliness of care (326), and the effect of simultaneous multidisciplinary appointments and weekly multidisciplinary management meetings (327). Comparative studies in this area are difficult because of the many confounding factors.
6.3 Involvement of GPs in managing malignant mesothelioma
GPs play a significant role in managing their patients with MPM. Communication between hospitals and GPs has been identified as an area that needs improvement (328). It is important to ensure that GPs are kept informed about their patients’ changing needs and have easy access to, and contact with, expert professionals to facilitate timely referrals and appropriate management when the patient is under treatment. This ongoing communication will help to avoid misdiagnosis, delays in starting treatment and unnecessary patient discomfort.
GP contact with MDT members can also optimise a patient’s ongoing care once discharged from hospital, and facilitates continuity of care and good communication between MDT members (328). The nurse care coordinator, a key member of the MDT, plays a pivotal role in liaising with the GP.
Research has shown the need for improved access to adequate information (329,330) and to out of hours care, such as specialist palliative care (328). Although some evidence is available about the optimal involvement of primary care in managing patients with cancer, there is no data on the perspectives of patients with malignant mesothelioma, or the views of their GPs.
Findings from a small exploratory study in Australian patients with lung cancer suggested that patients who live in rural areas have more symptoms and take considerably longer to consult their GP, leading to fewer treatment options (331). But, even in metropolitan areas, access to treatment is not guaranteed. A population based study in the Sydney area found that 28 percent of lung cancer patients did not receive any active treatment (332). The results of both of these studies reveal the importance of the timely involvement of an MDT for lung cancer patients and their findings are likely to be applicable to mesothelioma patients.
6.4 Nurse care coordinators
No studies have been conducted specifically on the impact of nurse care coordinators on patients with mesothelioma. One study involving thoracic oncology patients reported that nurse care coordinators can help to reduce the current unmet needs of these patients (333). Anecdotal evidence suggests that nurse care coordinators will have a similar positive impact on the outcomes for patients with MPM.
Nurse care coordinators play an important role in providing support and information to patients, and informed patients have been shown to have more positive outcomes (334). Care coordinators can also assist patients to navigate through their cancer journey (335) and such help has a positive impact on patient satisfaction (336).
The timeliness of care delivery is a key factor in multidisciplinary care (333). Nurse care coordinators work with other MDT professionals to ensure patients receive appropriate and timely care. Further research documenting the specific benefits of an MDT approach, and particularly the role of nurse care coordinators, would be useful.
6.5 The surgical team and outcomes in malignant pleural mesothelioma
There are several types of surgical treatments for MPM. These include VAT procedures for diagnosis and pleurodesis, and more complex procedures of P/D and EPP or pleuropneumonectomy (see Chapter 4 for more detail). The latter two procedures are only considered for selected patients with limited disease and are only performed within centres with the appropriate expertise and MDTs able to provide this therapy.
For diseases such as lung, prostate, breast, pancreatic and colorectal cancer, there is increasing evidence that the greater the volume of surgical oncological procedures conducted by a surgeon or centre, the better the patient outcomes, such as reduction in complications and patient fatalities (227,337-344). Population based case control studies confirm this, although confounders exist (345,346). One study showed that the volume of operations conducted by individual surgeons, rather than the hospital, correlated with a reduction in hospital inpatient deaths (347).
There is no direct comparative data from studies involving patients with MPM to support the proposition that a relationship exists between the volume of operations conducted by individual surgeons and improved treatment outcomes. However, it is highly likely that this relationship exists. Supportive evidence can be extrapolated from patient outcomes across different surgical series and specialist surgical centres over different time periods (230). One high volume centre in Australia has shown a significant reduction in operative mortality over a number of years suggesting that the experience of individual surgeons and their teams are important (348).
6.6 Follow-up
The optimal timing of follow-up and tests for patients with MPM has not been directly studied. Follow-up varies according to the type of therapy and its aims, and should be conducted according to the patient’s symptoms, the stage of the disease and the treatment goals.
Indirect evidence regarding the timing and type of tests is provided within the follow-up protocols of published randomised controlled trials (RCTs), and varies according to the type of therapy (chemotherapy or surgery) and its purpose.
The impact of a structured approach to patient follow-up and management is probably best seen in the active symptom control arm of the MS01 study. This randomised phase III trial compared the effectiveness of palliative therapy or active symptom control with or without different chemotherapy regimens in patients with MPM (201). In this trial the ‘essential elements of active symptom control were defined as regular follow-up in a specialist clinic; structured physical, psychological and social assessments at every clinic visit; rapid involvement of additional specialists; and parallel nursing support. Patients could receive, as required, steroids, analgesic drugs, appetite stimulants, bronchodilators, or palliative radiotherapy.’ The study results did not indicate an overall survival benefit for the specific chemotherapy used MVP or single agent vinorelbine. Importantly, it also did not show a difference in the predefined ‘quality of life’ subscales relevant to malignant mesothelioma (physical functioning, pain, dyspnoea and global health status). The active symptom control paradigm defined in the MS01 study is the closest any trial in MPM has come to defining a method of multidisciplinary patient-focused care. However, applying active symptom control as defined in the clinic requires mesothelioma-specific expertise that would be provided in an MDT environment.
General observations indicate that, apart from the MS01 study, patients receiving chemotherapy should be evaluated by CT every 2-3 cycles (6-9 weeks). Once treatment begins, patients should be reviewed by clinical assessment every 3-4 weeks depending on the treatment protocol. After completion of treatment, patients should be followed every 4-6 weeks or according to institutional protocol. Many clinical studies in MPM included ongoing CT scanning every 6-8 weeks to monitor and/or identify progression.
There is no direct evidence to support a specific protocol for clinical follow-up and test frequency for MPM. However, it would be reasonable to follow a similar protocol for monitoring patients when they are receiving chemotherapy or combined modality therapy, and to continue clinical monitoring and ongoing CT scanning thereafter where further treatment is anticipated in the event of progression.
Otherwise a pragmatic approach would be to order follow-up investigations according to patient symptoms and the intent of an intervention. A chest X-ray may be useful in identifying pleural effusions but its overall sensitivity is low compared with CT scanning. Consequently CT scanning would be the preferred radiological investigation. PET scanning is only to be used in circumstances where radical therapy is planned.
6.7 Allied health professionals
No studies have been conducted on the impact of allied health professional input on the outcomes for patients with MPM. Current practice tells us that allied health professionals are integral members of an MDT and may come from the following disciplines: nutrition and dietetics, occupational therapy, social work, clinical psychology, physiotherapy and pastoral care. Patients can be referred to these professionals at any time during their disease course and treatment trajectory. Feedback from patients suggests that input from allied health professionals contributes to patient satisfaction and improved quality of life by minimising their symptoms and/or helping them to cope with the disease and the effects of treatment as the disease progresses.
Appendix A: Future research areas
Development of accurate diagnostic, prognostic and predictive markers for malignant pleural mesothelioma
Development of sensitive methods that will assist in making an early diagnosis (of malignant pleural mesothelioma)
Validation of TNM system for staging of malignant pleural mesothelioma
Adequate selection of patients for radical (combined modality) therapy
Development of novel effective systemic therapies
Accurately define the optimal role of radiotherapy in malignant pleural mesothelioma
Prospectively evaluate the benefit of multidisciplinary care (MDT) in malignant pleural mesothelioma
Quality of Life studies in patients with malignant pleural mesothelioma
Psychosocial studies in patients with malignant pleural mesothelioma and their families
Patterns of care studies in patients with malignant pleural mesothelioma
Appendix B: Committee details
In the initial phase a core group of the Organizing Committee developed the guidelines scope and the following terms of reference.
- To oversee and direct the development of mesothelioma guidelines;
- To recruit and engage health professionals and others with expertise in mesothelioma and its treatment in Working Groups around the guidelines;
- To resolve differences in opinion among members and participant groups;
- To oversee drafting and to approve the final text;
- To be authors and accept the responsibilities of authorship in the production and publication of the final document.
The Organising Committee convened the first Steering Committee meeting (15th Feb 2010) where the purposes, scope, recommendations regarding the different disciplines that should be represented in the Guidelines Working Groups were determined. From this meeting five working groups were formed with two to three co-chairs per groups nominated. For each working group a list 5-6 relevant disciplines and clinical experts were formulated and subsequently sent a written invitation to join the Group. For each Working Group a consumer representative was also invited to join.
Working groups
Appendix C: Overview of guideline development process
These guidelines were developed in accordance with the NHMRC standard (1). All literature searches were completed by the 31st October 2011 identifying a combined total of 18,371 references. These articles, organized by PICO question, were screened by the appropriate Working Group co-chairs using the article title and abstract. Articles not meeting the inclusion criteria, and duplicates, were removed. This process resulted in 2,304 unique references for full text retrieval. These articles were entered into a database and a final assessment for relevance was made based on the full text article, by one of five independent readers. From this assessment 1,118 articles were deemed relevant to the Guidelines and went on to have an assessment of methodology and extraction of data. Eight potentially relevant papers could not be fully assessed as the full text articles were not obtained.
The 1,110 full text articles were categorised according to the main domain they sought to address (i.e., intervention, diagnosis, prognosis, aetiology, and screening) and rated according to the NHMRC level of evidence hierarchy (36). Individual studies were assessed in detail for methodological quality (risk of bias) using the methodology checklist from NICE and QUADAS 11 (36).
Summary data were extracted from each individual study and tabulated per PICO question in an Evidence Table. The Working Groups used these tables to assess and summaries the body of evidence informing each recommendation using the NHMRC Evidence Statement Form. Full details of the Guidelines development process can be found in the Technical Report.
Appendix D: NHMRC Evidence Statement Form
The body of evidence for each guideline recommendation was assessed and summarised using the NHMRC Evidence Statement Form (36) (see Technical Report for full details) according to five key components:
- Evidence base (the number, quality and level of evidence of studies);
- Consistency of results;
- Potential clinical impact of the proposed recommendation;
- Generalisability to the target population for the guideline;
- Applicability to the Australian healthcare context.
Each key component was rated using the NHMRC Body of Evidence matrix from ‘Excellent’ through to ‘Poor’. Summation of the ratings for the five key components allowed each guideline recommendation to be assigned an overall NHMRC Grade of Recommendation (A-D) ranging from ‘body of evidence can be trusted to guide practice’ to ‘ body of evidence is weak and recommendation must be applied with caution’. Where there was an absence of quality evidence, or low quality evidence, as the result of the systematic review, a consensus-based recommendation was made. Where there was no evidence or only very low evidence available a clinical practice point was made.
A final list of included studies and their evidence is contained in Evidence Tables (see Technical Report: C6); the Evidence Statement Form for each PICO (see Technical Report: C7).
Finally, each recommendation was discussed by all members of the Guideline Steering Committee in an open discussion.
Appendix E: Abbreviations
Appendix F: Glossary
Adenocarcinoma: cancer of glandular tissue present in surface structures of the human body.
Adjuvant chemotherapy: chemotherapy that is given in addition to the primary, main or initial treatment (surgery).
Adjuvant radiotherapy: radiotherapy that is given in addition to the primary, main or initial treatment.
Anti-cancer treatments: include surgery, chemotherapy and radiotherapy.
Asbestosis: a chronic inflammatory and fibrotic medical condition affecting the tissue of the lungs caused by the inhalation and retention of asbestos fibres.
Benign asbestos pleuritis: pleural effusion and/or thickening elicited by previous asbestos exposure.
Biomarker: indicator of a biological state. It is a characteristic that is objectively measured and evaluated as an indicator of normal biological processes , pathogenic processes, or pharmacologic responses to a therapeutic intervention.
Biopersistent: the persistence of a material in an organism (animals and humans).
Calretinin: a vitamin D-dependent calcium-binding protein involved in calcium signaling.
Carcinoembryonic antigen: a glycoprotein involved in cell adhesion which is usually not present in the blood of healthy adults.
Crocidolite: one of the types of asbestos , often referred to as blue asbestos.
Cuboidal: cuboid form.
Cytokeratin: proteins of keratin -containing intermediate filaments found in the intracytoplasmic cytoskeleton of epithelial tissue.
Cytology: the study of cells.
Cytological atypia: a condition of being irregular or nonstandard.
Cytoplasmic vacuoles: small cavities in the cytoplasm of a cell, bound by a single membrane and containing water, food, or metabolic waste.
Cytoreductive surgery: surgical removal of part of a malignant tumour which cannot be completely excised, so as to enhance the effectiveness of radiation or chemotherapy. It is used only in specific malignancies, as generally partial removal of a tumour is not considered a worthwhile intervention.
Desmoplasia: the growth of fibrous or connective tissue. It is also called desmoplastic reaction to emphasise that it is secondary to an insult. Desmoplasia may occur around a tumour.
Epitheloid: an epithelioid cell is a cell that resembles epithelial cells in that it directly contacts its neighboring cells via cell surface molecules or junctions.
Erionite: a naturally occurring fibrous mineral that belongs to a group of minerals called zeolites. Some properties of erionite are similar to the properties of asbestos.
Extrapleural pneumonectomy: a surgical treatment for malignant mesothelioma. It involves the removal of a lung, a portion of the diaphragm and the linings of the lungs and heart (parietal pleura and pericardium).
Fibrous pleuritis: an organising inflammation of the pleura, the lining of the pleural cavity surrounding the lungs.
Histiocytoma: a tumour consisting of histiocytes.
Immunohistochemistry: the process of detecting antigens (e.g. proteins) in cells of a tissue section by exploiting the principle of antibodies.
Leiomyosarcoma: a cancer of smooth muscle.
Lymphohistoiocytoid mesothelioma: variant of sarcomatoid mesothelioma.
Mediastinoscopy: a procedure that enables visualisation of the contents of the mediastinum (central compartment of the thoracic cavity), usually for the purpose of obtaining a biopsy.
Megakaryocyte potentiating factor: a biomarker for malignant pleural mesothelioma.
Mesothelial: a tumour marker for malignant pleural mesothelioma.
Neoadjuvant: the administration of therapeutic agents before a main treatment.
Neoplasia: an abnormal mass of tissue as a result of an abnormal proliferation of cells.
Pemetrexed: a chemotherapy drugs used to treat malignant mesothelioma.
PICO: patient, intervention, comparison, outcome.
Pleomorphism: variability in the size and shape of cells and/or their nuclei.
Pleural effusion: excess fluid that accumulates between the two pleural layers, the fluid-filled space that surrounds the lungs.
Pleural plaques: discrete fibrous or partially calcified thickened area which can be seen on x-rays of individuals exposed to asbestos.
Pleurectomy/decortication (P/D): a form of surgery performed on patients with malignant pleural mesothelioma. P/D aims to remove the lining surrounding the lung together with the tumour tissue.
Podoplanin: a human protein, the specific function of which has not been determined, but it has been proposed as a marker of lung injury.
Sarcomatoid: a growth pattern resembling a malignant tumour arising from connective tissues.
Soluble mesothelin-related protein: a biomarker for malignant pleural mesothelioma.
Squamous epithelium: epithelium characterised by its most superficial layer consisting of flat, scale-like cells called squamous epithelial cells.
Storiform: having an irregularly whorled pattern somewhat like that of a straw mat
Stromal tissue: the connective, supportive framework of tissue.
Synovial sarcoma: a rare form of cancer which usually occurs near to the joints of the arm, neck or leg.
Thoracocentesis: an invasive procedure to remove fluid or air from the pleural space for diagnostic or therapeutic purposes, also known as pleural tap.
Thoracotomy: is an incision into the pleural space of the chest.
Thrombomodulin: an integral membrane protein expressed on the surface of endothelial cells which serves as a cofactor for thrombin.
Thyroid transcription factor (TTF-1): a protein that regulates transcription of genes specific for the thyroid, lung, and diencephalon. It is also known as thyroid specific enhancer binding protein.
Transcription factor: sometimes called a sequence-specific DNA-binding factor, a transcription factor is a protein that binds to specific DNA sequences, thereby controlling the flow (or transcription) of genetic information from DNA to mRNA.
Trapped lung: unexpandable lung by constricting tumour growth and/or chronic pleural effusion.
Wilm’s tumour (WT): a cancer of the kidneys that typically occurs in children, also known as nephroblastoma.
Appendix G: Conflict of Interest
Members of the Steering Committee and the five Working Groups were required to declare their potential conflict of interests in writing prior to appointment. The purpose of declaring a conflict of interest was to avoid or manage any real or perceived conflict of interest between the private interests of the Steering Committee or Working Group members (including pecuniary interest or the possibility of other advantage) and their duties as part of the Committee or Working Group.
The members of the Steering Committee and Working Groups were required to update their information as they became aware of any changes in their circumstances. There was also an agenda item at the Steering Committee meetings where conflicts of interest was raised and documented.
All declarations of interests were added to a register and made available to the Chair and members of the Steering Committee. Open access to the register allowed the Steering Committee to consider all the potential conflicts of interest during discussion, decision-making and in the formulation of the
Acknowledgements
The development and dissemination of these Guidelines were funded by: a generous donation from the Biaggio Signorelli Foundation; grants from the Cancer Institute of NSW and Comcare’s Asbestos Innovation Fund, Comcare; a contribution from Cancer Council NSW, and in-kind contributions from the Asbestos Diseases Research Institute and the national team of experts.
This document is a general guide to appropriate practice, to be followed subject to the clinician’s judgment and the patient’s preference in each individual case. The guidelines are designed to provide information to assist in decision-making. They are based on the best evidence available at time of compilation. The guidelines are not meant to be prescriptive.
These guidelines were approved by the Chief Executive Officer of the National Health and Medical Research Council (NHMRC) on 2 July 2013, under Section 14A of the National Health and Medical Research Council Act 1992. In approving these guidelines the NHMRC considers that they meet the NHMRC standard for clinical practice guidelines. This approval is valid for a period of 5 years.
NHMRC is satisfied that they are based on the systematic identification and synthesis of the best available scientific evidence and make clear recommendations for health professionals practising in an Australian health care setting. The NHMRC expects that all guidelines will be reviewed no less than once every five years. This publication reflects the views of the authors and not necessarily the views of the Australian Government.
The development of these Guidelines was made possible by a generous donation from the Biaggio Signorelli Foundation; a Cancer Institute NSW grant and a contribution from Cancer Council NSW.
Disclosure: The development of these clinical practice guidelines has been undertaken by a working party of experts convened by the Asbestos Diseases Research Institute. Of the 47 experts involved five declared a potential conflict of interest. Advisory boards, and participation in educational meetings organised by the Pharma industry were mentioned as a source of potential conflicts of interests. The Guidelines Steering Committee reviewing the conflict of interest declarations concluded that the methodological rigor used for the evidence review and the involvement of many experts has effectively managed any conflict of interest real or perceived. None of the experts involved in the development of the Guidelines for the Diagnosis and Treatment of Malignant Pleural Mesothelioma has received remuneration for their activities. Three working party members, who were involved in reviewing and grading the available evidence, have received a modest compensation for the hundreds of hours spent on quality control.
References
- Procedures and requirements for meeting the 2011 NHMRC standard for clinical practice guidelines. version 1.1 ed. Melbourne: National Health and Medical Research Council, 2011.
- Leigh J, Driscoll T.. Malignant mesothelioma in Australia, 1945-2002. Int J Occup Environ Health 2003;9:206-17. [PubMed]
-
Musk AW, de Klerk NH. Epidemiology of malignant mesothelioma in Australia. Lung Cancer 2004;45 Suppl 1:S21-3.
[PubMed] - Mesothelioma in Australia Incidence 1982 to 2007 Mortality 1997 to 2007. Safe Work Australia, 2011:1-20. Available online: http://www.safeworkaustralia.gov.au/sites/swa/aboutsafeworkaustralia/whatwedo/publications/pages/Mesothelioma-in-Australia-2011.aspx
- Henderson DW, Whitaker D, Shilkin KB. The differential diagnosis of malignant mesothelioma: a practical approach to diagnosis during life. In: Henderson DW, Shilkin KB, Langlois SLP, et al. eds. Malignant mesothelioma. New York: Hemisphere, 1992:184.
- Attanoos RL, Gibbs AR. Primary malignant gonadal mesotheliomas and asbestos. Histopathology 2000;37:150-9. [PubMed]
- Clement PB, Young RH, Scully RE. Malignant mesotheliomas presenting as ovarian masses: a report of nine cases, including two primary ovarian mesotheliomas. Am J Surg Pathol 1996;20:1067-80. [PubMed]
- Asbestos. IARC Monographs on the Evaluation of Carcinogenic Risks to Humans. Geneva: WHO Press, 1977:1-106.
- Asbestos (Chrysotile, Amosite, Crocidolite, Tremolite, Actinolite, and Anthophyllite). Arsenic, Metals, Fibres, and Dusts 100 C. Geneva: WHO Press, 2012:219-310.
- Metintas M, Hillerdal G, Metintas S. Malignant mesothelioma due to environmental exposure to erionite: follow-up of a Turkish emigrant cohort. Eur Respir J 1999;13:523-6. [PubMed]
- Dodson RF, Williams MG Jr, Corn CJ, et al. Asbestos content of lung tissue, lymph nodes, and pleural plaques from former shipyard workers. Am Rev Respir Dis 1990;142:843-7. [PubMed]
- Asbestos: elimination of asbestos-related diseases. Fact sheet N°343 World Health Organisation, 2010. Available online: http://www.who.int/mediacentre/factsheets/fs343/en/index.html (cited 26 Oct 2011).
- Van der Schoot HC. Asbestosis & pleural tumors. Ned Tijdschr Geneeskd 1958;102:1125-6. [PubMed]
- Weiss A.. Pleurakrebs bei lungenasbestose, in vivo morphologisch gesichert. Medizinische 1953;1:93-4.
- Wagner JC, Sleggs CA, Marchand P. Diffuse pleural mesothelioma and asbestos exposure in the North Western Cape Province. Br J Ind Med 1960;17:260-71. [PubMed]
- Rake C, Gilham C, Hatch J, et al. Occupational, domestic and environmental mesothelioma risks in the British population: a case-control study. Br J Cancer 2009;100:1175-83. [PubMed]
- Pan XL, Day HW, Wang W, et al. Residential proximity to naturally occurring asbestos and mesothelioma risk in California. Am J Respir Crit Care Med 2005;172:1019-25. [PubMed]
- Maule MM, Magnani C, Dalmasso P, et al. Modeling mesothelioma risk associated with environmental asbestos exposure. Environ Health Perspect 2007;115:1066-71. [PubMed]
- De Bruin ML, Burgers JA, Baas P, et al. Malignant mesothelioma after radiation treatment for Hodgkin lymphoma. Blood 2009;113:3679-81. [PubMed]
- Tsao AS, Wistuba I, Roth JA, et al. Malignant pleural mesothelioma. J Clin Oncol 2009;27:2081-90. [PubMed]
- Scherpereel A, Astoul P, Baas P, et al. Guidelines of the European Respiratory Society and the European Society of Thoracic Surgeons for the management of malignant pleural mesothelioma. Eur Respir J 2010;35:479-95. [PubMed]
- Iwatsubo Y, Pairon JC, Boutin C, et al. Pleural mesothelioma: dose-response relation at low levels of asbestos exposure in a French population-based case-control study. Am J Epidemiol 1998;148:133-42. [PubMed]
- Hillerdal G.. Mesothelioma: cases associated with non-occupational and low dose exposures. Occup Environ Med 1999;56:505-13. [PubMed]
- Hyland RA, Ware S, Johnson AR, et al. Incidence trends and gender differences in malignant mesothelioma in New South Wales, Australia. Scand J Work Environ Health 2007;33:286-92. [PubMed]
- Lin RT, Takahashi K, Karjalainen A, et al. Ecological association between asbestos-related diseases and historical asbestos consumption: an international analysis. Lancet 2007;369:844-9. [PubMed]
- Australian Mesothelioma Registry 1st Annual Report Mesothelioma in Australia 2011Safe Work Australia. Available online: www.mesothelioma-australia.com (cited 1 Oct 2012).
- Aiello Bowles EJ, Tuzzio L, Wiese CJ, et al. Understanding high-quality cancer care: a summary of expert perspectives. Cancer 2008;112:934-42. [PubMed]
- Ensuring Quality Cancer Care. Washington, DC: National Academy Press, 1999. Available online: http://www.nap.edu/openbook.php?record_id=6467&page=R1 (cited 15 Sept 2011).
- Driscoll TR, Baker GJ, Daniels S, et al. Clinical aspects of malignant mesothelioma in Australia. Aust N Z J Med 1993;23:19-25. [PubMed]
- ESMO Guidelines Working Group, Manegold C. Malignant pleural mesothelioma: ESMO clinical recommendations for diagnosis, treatment and follow-up. Ann Oncol 2007;18 Suppl 2:ii34-5. [PubMed]
- Stahel RA, Weder W, Lievens Y, et al. Malignant pleural mesothelioma: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 2010;21 Suppl 5:v126-8. [PubMed]
- Rice D, Rusch V, Pass H, et al. Recommendations for uniform definitions of surgical techniques for malignant pleural mesothelioma: a consensus report of the international association for the study of lung cancer international staging committee and the international mesothelioma interest group. J Thorac Oncol 2011;6:1304-12. [PubMed]
- Lianes P, Remon J, Bover I, et al. SEOM guidelines for the treatment of malignant pleural mesothelioma. Clin Transl Oncol 2011;13:569-73. [PubMed]
- Pinto C, Ardizzoni A, Betta PG, et al. Expert opinions of the first italian consensus conference on the management of malignant pleural mesothelioma. Am J Clin Oncol 2011;34:99-109. [PubMed]
- Ettinger DS, Akerley W, Borghaei H, et al. Malignant pleural mesothelioma. Clinical practice guidelines in oncology. J Natl Compr Canc Netw 2012;10:26-41. [PubMed]
- NHMRC additional levels of evidence and grades for recommendations for developers of guidelines. NHMRC. 2009. Available online: http://www.nhmrc.gov.au/guidelines/resources-guideline-developers (cited 1 Feb 2010).
- Musk AW, De Klerk N, Eccles JL, et al. Malignant mesothelioma in Pilbara Aborigines. Aust J Public Health 1995;19:520-2. [PubMed]
- Moerman LC, van der Laan SL. The Baryulgil Mine: Asbestos and Aboriginality. Paper prepared for presentation at AIRA, 2010, Sydney 2010. Available online: http://apira2010.econ.usyd.edu.au/conference_proceedings/APIRA-2010-066-Moerman-Accountability-asbestos-and-indigenous-rights.pdf (cited 15 Sept 2011).
- Yates DH, Corrin B, Stidolph PN, et al. Malignant mesothelioma in south east England: Clinicopathological experience of 272 cases. Thorax 1997;52:507-12. [PubMed]
- Churg A, Roggli V, Galateau-Salle F. Mesothelioma. In: Travis WD, Brambilla E, Muller-Hermelink HK, et al. eds. Pathology & Genetics: Tumours of the Lung Pleura, Thymus and Heart. Lyon: IARC Press, 2004:128-36.
- Galateau-Sallé F. eds. Pathology of Malignant Mesothelioma. London: Springer-Verlag, 2010.
- British Thoracic Society Standards of Care Committee. BTS statement on malignant mesothelioma in the UK, 2007. Thorax 2007;62 Suppl 2:ii1-ii19. [PubMed]
- Aerts JG, Delahaye M, van der Kwast TH, et al. The high post-test probability of a cytological examination renders further investigations to establish a diagnosis of epithelial malignant pleural mesothelioma redundant. Diagn Cytopathol 2006;34:523-7. [PubMed]
- Hammar SP, Henderson DW, Klebe S, et al. Neoplasms of the pleura. In: Tomashefski JF Jr. eds. Dail and Hammar’s Pulmonary Pathology. Third ed II: Neoplastic Lung Disease. New York: Springer, 2008:558-734.
- Husain AN, Colby TV, Ordonez NG, et al. Guidelines for pathologic diagnosis of malignant mesothelioma: A consensus statement from the International Mesothelioma Interest Group. Arch Pathol Lab Med 2009;133:1317-31. [PubMed]
- Maskell NA, Gleeson FV, Davies RJ. Standard pleural biopsy versus CT-guided cutting-needle biopsy for diagnosis of malignant disease in pleural effusions: a randomised controlled trial. Lancet 2003;361:1326-30. [PubMed]
- Metintas M, Ak G, Dundar E, et al. Medical thoracoscopy vs CT scan-guided Abrams pleural needle biopsy for diagnosis of patients with pleural effusions: a randomized, controlled trial. Chest 2010;137:1362-8. [PubMed]
- Zahid I, Sharif S, Routledge T, et al. What is the best way to diagnose and stage malignant pleural mesothelioma? Interact Cardiovasc Thorac Surg 2011;12:254-9. [PubMed]
- Adams RF, Gleeson FV. Percutaneous image-guided cutting-needle biopsy of the pleura in the presence of a suspected malignant effusion. Radiology 2001;219:510-4. [PubMed]
- Greillier L, Cavailles A, Fraticelli A, et al. Accuracy of pleural biopsy using thoracoscopy for the diagnosis of histologic subtype in patients with malignant pleural mesothelioma. Cancer 2007;110:2248-52. [PubMed]
- Rahman NM, Gleeson FV. Image-guided pleural biopsy. Curr Opin Pulm Med 2008;14:331-6. [PubMed]
- Medford AR, Agrawal S, Free CM, et al. A local anaesthetic video-assisted thoracoscopy service: prospective performance analysis in a UK tertiary respiratory centre. Lung Cancer 2009;66:355-8. [PubMed]
- Bueno R, Reblando J, Glickman J, et al. Pleural biopsy: a reliable method for determining the diagnosis but not subtype in mesothelioma. Ann Thorac Surg 2004;78:1774-6. [PubMed]
- Attanoos RL, Gibbs AR. The comparative accuracy of different pleural biopsy techniques in the diagnosis of malignant mesothelioma. Histopathology 2008;53:340-4. [PubMed]
- Kao SC, Yan TD, Lee K, et al. Accuracy of diagnostic biopsy for the histological subtype of malignant pleural mesothelioma. J Thorac Oncol 2011;6:602-5. [PubMed]
- Henderson DW, Shilkin KB, Whitaker D. Reactive mesothelial hyperplasia vs mesothelioma, including mesothelioma in situ: a brief review. Am J Clin Pathol 1998;110:397-404. [PubMed]
- Churg A, Colby TV, Cagle P, et al. The separation of benign and malignant mesothelial proliferations. Am J Surg Pathol 2000;24:1183-200. [PubMed]
- Whitaker D.. The cytology of malignant mesothelioma. Cytopathology 2000;11:139-51. [PubMed]
- Renshaw AA, Dean BR, Antman KH, et al. The role of cytologic evaluation of pleural fluid in the diagnosis of malignant mesothelioma. Chest 1997;111:106-9. [PubMed]
- Welker L, Muller M, Holz O, et al. Cytological diagnosis of malignant mesothelioma - Improvement by additional analysis of hyaluronic acid in pleural effusions. Virchows Arch 2007;450:455-61. [PubMed]
- Cury PM, Butcher DN, Corrin B, et al. The use of histological and immunohistochemical markers to distinguish pleural malignant mesothelioma and in situ mesothelioma from reactive mesothelial hyperplasia and reactive pleural fibrosis. J Pathol 1999;189:251-7. [PubMed]
- Attanoos RL, Griffin A, Gibbs AR. The use of immunohistochemistry in distinguishing reactive from neoplastic mesothelium. A novel use for desmin and comparative evaluation with epithelial membrane antigen, p53, platelet-derived growth factor-receptor, P-glycoprotein and Bcl-2. Histopathology 2003;43:231-8. [PubMed]
- King J, Thatcher N, Pickering C, et al. Sensitivity and specificity of immunohistochemical antibodies used to distinguish between benign and malignant pleural disease: a systematic review of published reports. Histopathology 2006;49:561-8. [PubMed]
- Saad RS, Cho P, Liu YL, et al. The value of epithelial membrane antigen expression in separating benign mesothelial proliferation from malignant mesothelioma: a comparative study. Diagn Cytopathol 2005;32:156-9. [PubMed]
- Kato Y, Tsuta K, Seki K, et al. Immunohistochemical detection of GLUT-1 can discriminate between reactive mesothelium and malignant mesothelioma. Mod Pathol 2007;20:215-20. [PubMed]
- Monaco SE, Shuai Y, Bansal M, et al. The diagnostic utility of p16 FISH and GLUT-1 immunohistochemical analysis in mesothelial proliferations. Am J Clin Pathol 2011;135:619-27. [PubMed]
- Chiosea S, Krasinskas A, Cagle PT, et al. Diagnostic importance of 9p21 homozygous deletion in malignant mesotheliomas. Mod Pathol 2008;21:742-7. [PubMed]
- Chung CT, Santos Gda C, Hwang DM, et al. FISH assay development for the detection of p16/CDKN2A deletion in malignant pleural mesothelioma. J Clin Pathol 2010;63:630-4. [PubMed]
- Klebe S, Brownlee NA, Mahar A, et al. Sarcomatoid mesothelioma: A clinical-pathologic correlation of 326 cases. Mod Pathol 2010;23:470-9. [PubMed]
- Klebe S, Mahar A, Henderson DW, et al. Malignant mesothelioma with heterologous elements: clinicopathological correlation of 27 cases and literature review. Mod Pathol 2008;21:1084-94. [PubMed]
- Mangano WE, Cagle PT, Churg A, et al. The diagnosis of desmoplastic malignant mesothelioma and its distinction from fibrous pleurisy: A histologic and immunohistochemical analysis of 31 cases including p53 immunostaining. Am J Clin Pathol 1998;110:191-9. [PubMed]
- Edwards JG, Abrams KR, Leverment JN, et al. Prognostic factors for malignant mesothelioma in 142 patients: Validation of CALGB and EORTC prognostic scoring systems. Thorax 2000;55:731-5. [PubMed]
- Neumann V, Rutten A, Scharmach M, et al. Factors influencing long-term survival in mesothelioma patients--results of the German mesothelioma register. Int Arch Occup Environ Health 2004;77:191-9. [PubMed]
- Schramm A, Opitz I, Thies S, et al. Prognostic significance of epithelial-mesenchymal transition in malignant pleural mesothelioma. Eur J Cardiothorac Surg 2010;37:566-72. [PubMed]
- Flores RM, Zakowski M, Venkatraman E, et al. Prognostic factors in the treatment of malignant pleural mesothelioma at a large tertiary referral center. J Thorac Oncol 2007;2:957-65. [PubMed]
- Curran D, Sahmoud T, Therasse P, et al. Prognostic factors in patients with pleural mesothelioma: the European Organization for Research and Treatment of Cancer experience. J Clin Oncol 1998;16:145-52. [PubMed]
- Antman K, Shemin R, Ryan L, et al. Malignant mesothelioma: prognostic variables in a registry of 180 patients, the Dana-Farber Cancer Institute and Brigham and Women’s Hospital experience over two decades, 1965-1985. J Clin Oncol 1988;6:147-53. [PubMed]
- Cury PM, Butcher DN, Fisher C, et al. Value of the mesothelium-associated antibodies thrombomodulin, cytokeratin 5/6, calretinin, and CD44H in distinguishing epithelioid pleural mesothelioma from adenocarcinoma metastatic to the pleura. Mod Pathol 2000;13:107-12. [PubMed]
- Klebe S, Nurminen M, Leigh J, et al. Diagnosis of epithelial mesothelioma using tree-based regression analysis and a minimal panel of antibodies. Pathology 2009;41:140-8. [PubMed]
- Sheibani K, Shin SS, Kezirian J, et al. Ber-EP4 antibody as a discriminant in the differential diagnosis of malignant mesothelioma versus adenocarcinoma. Am J Surg Pathol 1991;15:779-84. [PubMed]
- Dejmek A, Hjerpe A.. Carcinoembryonic antigen-like reactivity in malignant mesothelioma: A comparison between different commercially available antibodies. Cancer 1994;73:464-9. [PubMed]
- Skov BG, Lauritzen AF, Hirsch F, et al. The histopathological diagnosis of malignant mesothelioma v. pulmonary adenocarcinoma: Reproducibility of the histopathological diagnosis. Histopathology 1994;24:553-7. [PubMed]
- Dejmek A, Hjerpe A.. Reactivity of six antibodies in effusions of mesothelioma, adenocarcinoma and mesotheliosis: stepwise logistic regression analysis. Cytopathology 2000;11:8-17. [PubMed]
- Dejmek A, Hjerpe A.. The combination of CEA, EMA, and BerEp4 and hyaluronan analysis specifically identifies 79% of all histologically verified mesotheliomas causing an effusion. Diagn Cytopathol 2005;32:160-6. [PubMed]
- Hirano T, Gong Y, Yoshida K, et al. Usefulness of TA02 (napsin A) to distinguish primary lung adenocarcinoma from metastatic lung adenocarcinoma. Lung Cancer. 2003;41:155-62. [PubMed]
- Bishop JA, Sharma R, Illei PB. Napsin A and thyroid transcription factor-1 expression in carcinomas of the lung, breast, pancreas, colon, kidney, thyroid, and malignant mesothelioma. Hum Pathol 2010;41:20-5. [PubMed]
- Ordóñez NG. The immunohistochemical diagnosis of mesothelioma. Differentiation of mesothelioma and lung adenocarcinoma. Am J Surg Pathol 1989;13:276-91. [PubMed]
- Wirth PR, Legier J, Wright GL Jr. Immunohistochemical evaluation of seven monoclonal antibodies for differentiation of pleural mesothelioma from lung adenocarcinoma. Cancer 1991;67:655-62. [PubMed]
- Collins CL, Schaefer R, Cook CD, et al. Thrombomodulin expression in malignant pleural mesothelioma and pulmonary adenocarcinoma. Eur Respir Rev 1993;3:59-60.
- Miettinen M, Kvatich AJ. HBME-1: a monoclonal antibody useful in the differential diagnosis of mesothelioma, adenocarcinoma and soft tissue and bone tumor. AppL Immunohistochem 1995;3:115.
- Gotzos V, Vogt P, Celio MR. The calcium binding protein calretinin is a selective marker for malignant pleural mesotheliomas of the epithelial type. Pathol Res Pract 1996;192:137-47. [PubMed]
- Donna A, Betta PG, Chiodera P, et al. Newly marketed tissue markers for malignant mesothelioma: immunoreactivity of rabbit AMAD-2 antiserum compared with monoclonal antibody HBME-1 and a review of the literature on so-called antimesothelioma antibodies. Hum Pathol 1997;28:929-37. [PubMed]
- Kennedy AD, King G, Kerr KM. HBME-1 and antithrombomodulin in the differential diagnosis of malignant mesothelioma of pleura. J Clin Pathol 1997;50:859-62. [PubMed]
- Ordóñez NG. The value of antibodies 44-3A6, SM3, HBME-1, and thrombomodulin in differentiating epithelial pleural mesothelioma from lung adenocarcinoma: a comparative study with other commonly used antibodies. Am J Surg Pathol 1997;21:1399-408. [PubMed]
- Riera JR, Astengo-Osuna C, Longmate JA, et al. The immunohistochemical diagnostic panel for epithelial mesothelioma: a reevaluation after heat-induced epitope retrieval. Am J Surg Pathol 1997;21:1409-19. [PubMed]
- Wick MR. Immunophenotyping of malignant mesothelioma. Am J Surg Pathol 1997;21:1395-8. [PubMed]
- Di Loreto C, Puglisi F, Di Lauro V, et al. TTF-1 protein expression in pleural malignant mesotheliomas and adenocarcinomas of the lung. Cancer Lett 1998;124:73-8. [PubMed]
- Oates J, Edwards C.. HBME-1, MOC-31, WT1 and calretinin: an assessment of recently described markers for mesothelioma and adenocarcinoma. Histopathology 2000;36:341-7. [PubMed]
- Attanoos RL, Webb R, Dojcinov SD, et al. Malignant epithelioid mesothelioma: anti-mesothelial marker expression correlates with histological pattern. Histopathology 2001;39:584-8. [PubMed]
- Comin CE, Novelli L, Boddi V, et al. Calretinin, thrombomodulin, CEA, and CD15: a useful combination of immunohistochemical markers for differentiating pleural epithelial mesothelioma from peripheral pulmonary adenocarcinoma. Hum Pathol 2001;32:529-36. [PubMed]
- Foster MR, Johnson JE, Olson SJ, et al. Immunohistochemical analysis of nuclear versus cytoplasmic staining of WT1 in malignant mesotheliomas and primary pulmonary adenocarcinomas. Arch Pathol Lab Med 2001;125:1316-20. [PubMed]
- Roberts F, McCall AE, Burnett RA. Malignant mesothelioma: A comparison of biopsy and postmortem material by light microscopy and immunohistochemistry. J Clin Pathol 2001;54:766-70. [PubMed]
- Wick MR, Moran CA, Mills SE, et al. Immunohistochemical differential diagnosis of pleural effusions, with emphasis on malignant mesothelioma. Curr Opin Pulm Med 2001;7:187-92. [PubMed]
- Chu PG, Weiss LM. Expression of cytokeratin 5/6 in epithelial neoplasms: an immunohistochemical study of 509 cases. Mod Pathol 2002;15:6-10. [PubMed]
- Miettinen M, Sarlomo-Rikala M.. Expression of calretinin, thrombomodulin, keratin 5, and mesothelin in lung carcinomas of different types: an immunohistochemical analysis of 596 tumors in comparison with epithelioid mesotheliomas of the pleura. Am J Surg Pathol 2003;27:150-8. [PubMed]
- Ordóñez NG. Application of mesothelin immunostaining in tumor diagnosis. Am J Surg Pathol 2003;27:1418-28. [PubMed]
- Chu AY, Litzky LA, Pasha TL, et al. Utility of D2-40, a novel mesothelial marker, in the diagnosis of malignant mesothelioma. Mod Pathol 2005;18:105-10. [PubMed]
- Granville LA, Younes M, Churg A, et al. Comparison of monoclonal versus polyclonal calretinin antibodies for immunohistochemical diagnosis of malignant mesothelioma. Appl Immunohistochem Mol Morphol 2005;13:75-9. [PubMed]
- Saad RS, Lindner JL, Lin X, et al. The diagnostic utility of D2-40 for malignant mesothelioma versus pulmonary carcinoma with pleural involvement. Diagn Cytopathol 2006;34:801-6. [PubMed]
- Yaziji H, Battifora H, Barry TS, et al. Evaluation of 12 antibodies for distinguishing epithelioid mesothelioma from adenocarcinoma: identification of a three-antibody immunohistochemical panel with maximal sensitivity and specificity. Mod Pathol 2006;19:514-23. [PubMed]
- Hinterberger M, Reineke T, Storz M, et al. D2-40 and calretinin - a tissue microarray analysis of 341 malignant mesotheliomas with emphasis on sarcomatoid differentiation. Mod Pathol 2007;20:248-55. [PubMed]
- Mimura T, Ito A, Sakuma T, Ohbayashi C, et al. Novel marker D2-40, combined with calretinin, CEA, and TTF-1: an optimal set of immunodiagnostic markers for pleural mesothelioma. Cancer 2007;109:933-8. [PubMed]
- Hanna A, Pang Y, Bedrossian CW, et al. Podoplanin is a useful marker for identifying mesothelioma in malignant effusions. Diagn Cytopathol 2010;38:264-9. [PubMed]
- Tot T.. The value of cytokeratins 20 and 7 in discriminating metastatic adenocarcinomas from pleural mesotheliomas. Cancer 2001;92:2727-32. [PubMed]
- Powell G, Roche H, Roche WR. Expression of calretinin by breast carcinoma and the potential for misdiagnosis of mesothelioma. Histopathology 2011;59:950-6. [PubMed]
- Duhig EE, Kalpakos L, Yang IA, et al. Mesothelial markers in high-grade breast carcinoma. Histopathology 2011;59:957-64. [PubMed]
- Kushitani K, Takeshima Y, Amatya VJ, et al. Differential diagnosis of sarcomatoid mesothelioma from true sarcoma and sarcomatoid carcinoma using immunohistochemistry. Pathol Int 2008;58:75-83. [PubMed]
- Takeshima Y, Amatya VJ, Kushitani K, et al. Value of immunohistochemistry in the differential diagnosis of pleural sarcomatoid mesothelioma from lung sarcomatoid carcinoma. Histopathology 2009;54:667-76. [PubMed]
- Attanoos RL, Dojcinov SD, Webb R, et al. Anti-mesothelial markers in sarcomatoid mesothelioma and other spindle cell neoplasms. Histopathology 2000;37:224-31. [PubMed]
- Greillier L, Baas P, Welch JJ, et al. Biomarkers for malignant pleural mesothelioma: current status. Mol Diagn Ther 2008;12:375-90. [PubMed]
- Benjamin H, Lebanony D, Rosenwald S, et al. A diagnostic assay based on microRNA expression accurately identifies malignant pleural mesothelioma. J Mol Diagn 2010;12:771-9. [PubMed]
- Robinson BW, Creaney J, Lake R, et al. Mesothelin-family proteins and diagnosis of mesothelioma. Lancet 2003;362:1612-6. [PubMed]
- Creaney J, Robinson BW. Detection of malignant mesothelioma in asbestos-exposed individuals: the potential role of soluble mesothelin-related protein. Hematol Oncol Clin North Am 2005;19:1025-40. [PubMed]
- Robinson BW, Creaney J, Lake R, et al. Soluble mesothelin-related protein--a blood test for mesothelioma. Lung Cancer 2005;49 Suppl 1:S109-11. [PubMed]
- Onda M, Nagata S, Ho M, et al. Megakaryocyte potentiation factor cleaved from mesothelin precursor is a useful tumor marker in the serum of patients with mesothelioma. Clin Cancer Res 2006;12:4225-31. [PubMed]
- Scherpereel A, Grigoriu B, Conti M, et al. Soluble mesothelin-related peptides in the diagnosis of malignant pleural mesothelioma. Am J Respir Crit Care Med 2006;173:1155-60. [PubMed]
- Creaney J, van Bruggen I, Hof M, et al. Combined CA125 and mesothelin levels for the diagnosis of malignant mesothelioma. Chest 2007;132:1239-46. [PubMed]
- Cristaudo A, Foddis R, Vivaldi A, et al. Clinical significance of serum mesothelin in patients with mesothelioma and lung cancer. Clin Cancer Res 2007;13:5076-81. [PubMed]
- Scherpereel A, Lee YC. Biomarkers for mesothelioma. Curr Opin Pulm Med 2007;13:339-443. [PubMed]
- Tigrani DY, Weydert JA. Immunohistochemical expression of osteopontin in epithelioid mesotheliomas and reactive mesothelial proliferations. Am J Clin Pathol 2007;127:580-4. [PubMed]
- Creaney J, Yeoman D, Demelker Y, et al. Comparison of osteopontin, megakaryocyte potentiating factor, and mesothelin proteins as markers in the serum of patients with malignant mesothelioma. J Thorac Oncol 2008;3:851-7. [PubMed]
- Pass HI, Wali A, Tang N, et al. Soluble mesothelin-related peptide level elevation in mesothelioma serum and pleural effusions. Ann Thorac Surg 2008;85:265-72; discussion 272. [PubMed]
- Park EK, Sandrini A, Yates DH, et al. Soluble mesothelin-related protein in an asbestos-exposed population: the dust diseases board cohort study. Am J Respir Crit Care Med 2008;178:832-7. [PubMed]
- Pass HI, Carbone M. Current Status of Screening for Malignant Pleural Mesothelioma. Semin Thorac Cardiovasc Surg 2009;21:97-104. [PubMed]
- Rodríguez Portal JA, Rodríguez Becerra E, Rodríguez Rodríguez D, et al. Serum levels of soluble mesothelin-related peptides in malignant and nonmalignant asbestos-related pleural disease: relation with past asbestos exposure. Cancer Epidemiol Biomarkers Prev 2009;18:646-50. [PubMed]
- Hollevoet K, Nackaerts K, Thimpont J, et al. Diagnostic performance of soluble mesothelin and megakaryocyte potentiating factor in mesothelioma. Am J Respir Crit Care Med 2010;181:620-5. [PubMed]
- Park EK, Thomas PS, Yates DH. Biomarkers for early detection of mesothelioma in asbestos-exposed subjects. Clin Chem Lab Med 2010;48:1673-4. [PubMed]
- Rai AJ, Flores RM, Mathew A, et al. Soluble mesothelin related peptides (SMRP) and osteopontin as protein biomarkers for malignant mesothelioma: Analytical validation of ELISA based assays and characterization at mRNA and protein levels. Clin Chem Lab Med 2010;48:271-8. [PubMed]
- Hollevoet K, Van Cleemput J, Thimpont J, et al. Serial measurements of mesothelioma serum biomarkers in asbestos-exposed individuals: a prospective longitudinal cohort study. J Thorac Oncol 2011;6:889-95. [PubMed]
- Creaney J, Francis RJ, Dick IM, et al. Serum soluble mesothelin concentrations in malignant pleural mesothelioma: relationship to tumor volume, clinical stage and changes in tumor burden. Clin Cancer Res 2011;17:1181-9. [PubMed]
- Shiomi K, Shiomi S, Ishinaga Y, et al. Impact of renal failure on the tumor markers of mesothelioma, N-ERC/mesothelin and osteopontin. Anticancer Res 2011;31:1427-30. [PubMed]
- Roe OD, Creaney J, Lundgren S, et al. Mesothelin-related predictive and prognostic factors in malignant mesothelioma: a nested case-control study. Lung Cancer 2008;61:235-43. [PubMed]
- Boudville N, Paul R, Robinson BW, et al. Mesothelin and kidney function--analysis of relationship and implications for mesothelioma screening. Lung Cancer 2011;73:320-4. [PubMed]
- Hollevoet K, Reitsma JB, Creaney J, et al. Serum mesothelin for diagnosing malignant pleural mesothelioma: an individual patient data meta-analysis. J Clin Oncol 2012;30:1541-9. [PubMed]
- Klebe S, Henderson DW. Early stages of mesothelioma, screening and biomarkers. Recent Results Cancer Res 2011;189:169-93. [PubMed]
- Kao SC, Reid G, van Zandwijk N, et al. Molecular biomarkers in malignant mesothelioma: state of the art. Pathology 2011;43:201-12. [PubMed]
- van der Bij S, Schaake E, Koffijberg H, et al. Markers for the non-invasive diagnosis of mesothelioma: a systematic review. Br J Cancer 2011;104:1325-33. [PubMed]
- Bégueret H, Galateau-Salle F, Guillou L, et al. Primary intrathoracic synovial sarcoma: a clinicopathologic study of 40 t(X;18)-positive cases from the French Sarcoma Group and the Mesopath Group. Am J Surg Pathol 2005;29:339-46. [PubMed]
- Weinbreck N, Vignaud JM, Begueret H, et al. SYT-SSX fusion is absent in sarcomatoid mesothelioma allowing its distinction from synovial sarcoma of the pleura. Mod Pathol 2007;20:617-21. [PubMed]
- Butchart EG, Ashcroft T, Barnsley WC, et al. Pleuropneumonectomy in the management of diffuse malignant mesothelioma of the pleura. Experience with 29 patients. Thorax 1976;31:15-24. [PubMed]
- Mattson K.. Natural history and clinical staging of malignant mesothelioma. Eur J Respir Dis 1982;63:87-91.
- Boutin C, Rey F.. Thoracoscopy in pleural malignant mesothelioma: a prospective study of 188 consecutive patients: Part 1: Diagnosis. Cancer 1993;72:389-93. [PubMed]
- Sugarbaker DJ, Strauss GM, Lynch TJ, et al. Node status has prognostic significance in the multimodality therapy of diffuse, malignant mesothelioma. J Clin Oncol 1993;11:1172-8. [PubMed]
- Rusch VW. A proposed new international TNM staging system for malignant pleural mesothelioma. From the International Mesothelioma Interest Group. Chest 1995;108:1122-8. [PubMed]
- Burgers JA, Damhuis RA. Prognostic factors in malignant mesothelioma. Lung Cancer 2004;45 Suppl 1:S49-54. [PubMed]
- Rusch VW, Venkatraman ES. Important prognostic factors in patients with malignant pleural mesothelioma, managed surgically. Ann Thorac Surg 1999;68:1799-804. [PubMed]
- Rusch VW, Rosenzweig K, Venkatraman E, et al. A phase II trial of surgical resection and adjuvant high-dose hemithoracic radiation for malignant pleural mesothelioma. J Thorac Cardiovasc Surg 2001;122:788-95. [PubMed]
- Aziz T, Jilaihawi A, Prakash D.. The management of malignant pleural mesothelioma; single centre experience in 10 years. Eur J Cardiothorac Surg 2002;22:298-305. [PubMed]
- Stewart DJ, Martin-Ucar A, Pilling JE, et al. The effect of extent of local resection on patterns of disease progression in malignant pleural mesothelioma. Ann Thorac Surg 2004;78:245-52. [PubMed]
- Tammilehto L, Kivisaari L, Salminen US, et al. Evaluation of the clinical TNM staging system for malignant pleural mesothelioma: an assessment in 88 patients. Lung Cancer 1995;12:25-34. [PubMed]
- Nowak AK, Armato SG 3rd, Ceresoli GL, et al. Imaging in pleural mesothelioma: a review of imaging research presented at the 9th International Meeting of the International Mesothelioma Interest Group. Lung Cancer 2010;70:1-6. [PubMed]
- Rusch VW, Giroux D, Kennedy C, et al. Initial Analysis of the International Association For the Study of Lung Cancer Mesothelioma Database. J Thorac Oncol 2012;7:1631-9. [PubMed]
- Rusch VW, Godwin JD, Shuman WP. The role of computed tomography scanning in the initial assessment and the follow-up of malignant pleural mesothelioma. J Thorac Cardiovasc Surg 1988;96:171-7. [PubMed]
- Basu S, Saboury B, Torigian DA, et al. Current Evidence Base of FDG-PET/CT Imaging in the Clinical Management of Malignant Pleural Mesothelioma: Emerging Significance of Image Segmentation and Global Disease Assessment. Mol Imaging Biol 2011;13:801-11. [PubMed]
- Schouwink JH, Kool LS, Rutgers EJ, et al. The value of chest computer tomography and cervical mediastinoscopy in the preoperative assessment of patients with malignant pleural mesothelioma. Ann Thorac Surg 2003;75:1715-8; discussion 1718-9.
- Alvarez JM, Hasani A, Segal A, et al. Bilateral thoracoscopy, mediastinoscopy and laparoscopy, in addition to CT, MRI and PET imaging, are essential to correctly stage and treat patients with mesothelioma prior to trimodality therapy. ANZ J Surg 2009;79:734-8. [PubMed]
- Wilcox BE, Subramaniam RM, Peller PJ, et al. Utility of integrated computed tomography-positron emission tomography for selection of operable malignant pleural mesothelioma. Clin Lung Cancer 2009;10:244-8. [PubMed]
- Maasilta P, Kivisaari L, Holsti LR, et al. Radiographic chest assessment of lung injury following hemithorax irradiation for pleural mesothelioma. Eur Respir J 1991;4:76-83. [PubMed]
- Flores RM, Akhurst T, Gonen M, et al. Positron emission tomography defines metastatic disease but not locoregional disease in patients with malignant pleural mesothelioma. J Thorac Cardiovasc Surg 2003;126:11-6. [PubMed]
- de Perrot M, Uy K, Anraku M, et al. Impact of lymph node metastasis on outcome after extrapleural pneumonectomy for malignant pleural mesothelioma. J Thorac Cardiovasc Surg 2007;133:111-6. [PubMed]
- Pilling J, Dartnell JA, Lang-Lazdunski L. Integrated positron emission tomography-computed tomography does not accurately stage intrathoracic disease of patients undergoing trimodality therapy for malignant pleural mesothelioma. Thorac Cardiovasc Surg 2010;58:215-9. [PubMed]
- Plathow C, Staab A, Schmaehl A, et al. Computed tomography, positron emission tomography, positron emission tomography/computed tomography, and magnetic resonance imaging for staging of limited pleural mesothelioma: initial results. Invest Radiol 2008;43:737-44. [PubMed]
- Sharif S, Zahid I, Routledge T, et al. Does positron emission tomography offer prognostic information in malignant pleural mesothelioma? Interact Cardiovasc Thorac Surg 2011;12:806-11. [PubMed]
- Erasmus JJ, Truong MT, Smythe WR, et al. Integrated computed tomography-positron emission tomography in patients with potentially resectable malignant pleural mesothelioma: Staging implications. J Thorac Cardiovasc Surg 2005;129:1364-70. [PubMed]
- Heelan RT, Rusch VW, Begg CB, et al. Staging of malignant pleural mesothelioma: comparison of CT and MR imaging. AJR Am J Roentgenol 1999;172:1039-47. [PubMed]
- Edwards JG, Stewart DJ, Martin-Ucar A, et al. The pattern of lymph node involvement influences outcome after extrapleural pneumonectomy for malignant mesothelioma. J Thorac Cardiovasc Surg 2006;131:981-7. [PubMed]
- Sørensen JB, Ravn J, Loft A, et al. Preoperative staging of mesothelioma by 18F-fluoro-2-deoxy-D-glucose positron emission tomography/computed tomography fused imaging and mediastinoscopy compared to pathological findings after extrapleural pneumonectomy. Eur J Cardiothorac Surg 2008;34:1090-6. [PubMed]
- Mineo TC, Ambrogi V, Pompeo E, et al. The value of occult disease in resection margin and lymph node after extrapleural pneumonectomy for malignant mesothelioma. Ann Thorac Surg 2008;85:1740-6. [PubMed]
- Rice DC, Erasmus JJ, Stevens CW, et al. Extended surgical staging for potentially resectable malignant pleural mesothelioma. Ann Thorac Surg 2005;80:1988-92; discussion 1992-3.
- Tournoy KG, Burgers SA, Annema JT, et al. Transesophageal endoscopic ultrasound with fine needle aspiration in the preoperative staging of malignant pleural mesothelioma. Clin Cancer Res 2008;14:6259-63. [PubMed]
- Rice DC, Steliga MA, Stewart J, et al. Endoscopic ultrasound-guided fine needle aspiration for staging of malignant pleural mesothelioma. Ann Thorac Surg 2009;88:862-8; discussion 8-9. [PubMed]
- Rice DC, Stevens CW, Correa AM, et al. Outcomes after extrapleural pneumonectomy and intensity-modulated radiation therapy for malignant pleural mesothelioma. Ann Thorac Surg 2007;84:1685-92; discussion 1692-3.
- Herndon JE, Green MR, Chahinian AP, et al. Factors predictive of survival among 337 patients with mesothelioma treated between 1984 and 1994 by the Cancer and Leukemia Group B. Chest 1998;113:723-31. [PubMed]
- Francart J, Vaes E, Henrard S, et al. A prognostic index for progression-free survival in malignant mesothelioma with application to the design of phase II trials: a combined analysis of 10 EORTC trials. Eur J Cancer 2009;45:2304-11. [PubMed]
- Kao SC, Pavlakis N, Harvie R, et al. High blood neutrophil-to-lymphocyte ratio is an indicator of poor prognosis in malignant mesothelioma patients undergoing systemic therapy. Clin Cancer Res 2010;16:5805-13. [PubMed]
- Pinato DJ, Mauri FA, Ramakrishnan R, et al. Inflammation-based prognostic indices in malignant pleural mesothelioma. J Thorac Oncol 2012;7:587-94. [PubMed]
- Nojiri S, Gemba K, Aoe K, et al. Survival and prognostic factors in malignant pleural mesothelioma: a retrospective study of 314 patients in the west part of Japan. Jpn J Clin Oncol 2011;41:32-9. [PubMed]
- Schneider J, Hoffmann H, Dienemann H, et al. Diagnostic and prognostic value of soluble mesothelin-related proteins in patients with malignant pleural mesothelioma in comparison with benign asbestosis and lung cancer. J Thorac Oncol 2008;3:1317-24. [PubMed]
- Grigoriu BD, Scherpereel A, Devos P, et al. Utility of osteopontin and serum mesothelin in malignant pleural mesothelioma diagnosis and prognosis assessment. Clin Cancer Res 2007;13:2928-35. [PubMed]
- Francis RJ, Byrne MJ, van der Schaaf AA, et al. Early prediction of response to chemotherapy and survival in malignant pleural mesothelioma using a novel semiautomated 3-dimensional volume-based analysis of serial 18F-FDG PET scans. J Nucl Med 2007;48:1449-58. [PubMed]
- Nowak AK, Francis RJ, Phillips MJ, et al. A novel prognostic model for malignant mesothelioma incorporating quantitative FDG-PET imaging with clinical parameters. Clin Cancer Res 2010;16:2409-17. [PubMed]
- Ceresoli GL, Chiti A, Zucali PA, et al. Early response evaluation in malignant pleural mesothelioma by positron emission tomography with [18F]fluorodeoxyglucose. J Clin Oncol 2006;24:4587-93. [PubMed]
- Veit-Haibach P, Schaefer NG, Steinert HC, et al. Combined FDG-PET/CT in response evaluation of malignant pleural mesothelioma. Lung Cancer 2010;67:311-7. [PubMed]
- Gerbaudo VH, Mamede M, Trotman-Dickenson B, et al. FDG PET/CT patterns of treatment failure of malignant pleural mesothelioma: relationship to histologic type, treatment algorithm, and survival. Eur J Nucl Med Mol Imaging. 2011;38:810-21. [PubMed]
- van Meerbeeck JP, Gaafar R, Manegold C, et al. Randomized phase III study of cisplatin with or without raltitrexed in patients with malignant pleural mesothelioma: an intergroup study of the European Organisation for Research and Treatment of Cancer Lung Cancer Group and the National Cancer Institute of Canada. J Clin Oncol 2005;23:6881-9. [PubMed]
- Milano MT, Zhang H. Malignant pleural mesothelioma: a population-based study of survival. J Thorac Oncol 2010;5:1841-8. [PubMed]
- Musk AW, Olsen N, Alfonso H, et al. Predicting survival in malignant mesothelioma. Eur Respir J 2011;38:1420-4. [PubMed]
- Berghmans T, Paesmans M, Lalami Y, et al. Activity of chemotherapy and immunotherapy on malignant mesothelioma: a systematic review of the literature with meta-analysis. Lung Cancer 2002;38:111-21. [PubMed]
- Baas P.. Chemotherapy for malignant mesothelioma: from doxorubicin to vinorelbine. Semin Oncol 2002;29:62-9. [PubMed]
- Ellis P, Davies AM, Evans WK, et al. The use of chemotherapy in patients with advanced malignant pleural mesothelioma: a systematic review and practice guideline. J Thorac Oncol 2006;1:591-601. [PubMed]
- Muers MF, Stephens RJ, Fisher P, et al. Active symptom control with or without chemotherapy in the treatment of patients with malignant pleural mesothelioma (MS01): a multicentre randomised trial. Lancet 2008;371:1685-94. [PubMed]
- Vogelzang NJ, Rusthoven JJ, Symanowski J, et al. Phase III study of pemetrexed in combination with cisplatin versus cisplatin alone in patients with malignant pleural mesothelioma. J Clin Oncol 2003;21:2636-44. [PubMed]
- Carteni G, Manegold C, Garcia GM, et al. Malignant peritoneal mesothelioma-Results from the International Expanded Access Program using pemetrexed alone or in combination with a platinum agent. Lung Cancer 2009;64:211-8. [PubMed]
- Fennell DA, Gaudino G, O’Byrne KJ, et al. Advances in the systemic therapy of malignant pleural mesothelioma. Nat Clin Pract Oncol 2008;5:136-47. [PubMed]
- O’Brien ME, Watkins D, Ryan C, et al. A randomised trial in malignant mesothelioma (M) of early (E) versus delayed (D) chemotherapy in symptomatically stable patients: the MED trial. Ann Oncol 2006;17:270-5. [PubMed]
- van den Bogaert DP, Pouw EM, van Wijhe G, et al. Pemetrexed maintenance therapy in patients with malignant pleural mesothelioma. J Thorac Oncol 2006;1:25-30. [PubMed]
- Jassem J, Ramlau R, Santoro A, et al. Phase III trial of pemetrexed plus best supportive care compared with best supportive care in previously treated patients with advanced malignant pleural mesothelioma. J Clin Oncol 2008;26:1698-704. [PubMed]
- Razak ARA, Chatten KJ, Hughes AN. Retreatment with pemetrexed-based chemotherapy in malignant pleural mesothelioma (MPM): a second line treatment option. Lung Cancer 2008;60:294-7. [PubMed]
- Ceresoli GL, Zucali PA, Gianoncelli L, et al. Second-line treatment for malignant pleural mesothelioma. Cancer Treat Rev 2010;36:24-32. [PubMed]
- Jakobsen JN, Sorensen JB. Review on clinical trials of targeted treatments in malignant mesothelioma. Cancer Chemother Pharmacol 2011;68:1-15. [PubMed]
- Ho M, Hassan R, Zhang J, et al. Humoral immune response to mesothelin in mesothelioma and ovarian cancer patients. Clin Cancer Res 2005;11:3814-20. [PubMed]
- Robinson BW, Robinson C, Lake RA. Localised spontaneous regression in mesothelioma -- possible immunological mechanism. Lung Cancer 2001;32:197-201. [PubMed]
- Lew F, Tsang P, Holland JF, et al. High frequency of immune dysfunctions in asbestos workers and in patients with malignant mesothelioma. J Clin Immunol 1986;6:225-33. [PubMed]
- Hegmans JP, Veltman JD, Lambers ME, et al. Consolidative dendritic cell-based immunotherapy elicits cytotoxicity against malignant mesothelioma. Am J Respir Crit Care Med 2010;181:1383-90. [PubMed]
- Hassan R, Sharon E, Pastan I.. Mesothelin targeted chemo-immunotherapy for treatment of malignant mesothelioma and lung adenocarcinoma. Ann Oncol 2010;21:ii42.
- Vachani A, Moon E, Albelda SM. Gene therapy for mesothelioma. Curr Treat Options Oncol 2011;12:173-80. [PubMed]
- Grossebner MW, Arifi AA, Goddard M, et al. Mesothelioma--VATS biopsy and lung mobilization improves diagnosis and palliation. Eur J Cardiothorac Surg 1999;16:619-23. [PubMed]
- Tan C, Sedrakyan A, Browne J, et al. The evidence on the effectiveness of management for malignant pleural effusion: a systematic review. Eur J Cardiothorac Surg 2006;29:829-38. [PubMed]
- Shaw P, Agarwal R.. Pleurodesis for malignant pleural effusions. Cochrane Database Syst Rev 2004;CD002916. [PubMed]
- Soysal O, Karaoglanoglu N, Demiracan S, et al. Pleurectomy/decortication for palliation in malignant pleural mesothelioma: results of surgery. Eur J Cardiothorac Surg 1997;11:210-3. [PubMed]
- Halstead JC, Lim E, Venkateswaran RM, et al. Improved survival with VATS pleurectomy-decortication in advanced malignant mesothelioma. Eur J Surg Oncol 2005;31:314-20. [PubMed]
- Yan TD, Cao CQ, Boyer M, et al. Improving survival results after surgical management of malignant pleural mesothelioma: an Australian institution experience. Ann Thorac Cardiovasc Surg 2011;17:243-9. [PubMed]
- Grondin SC, Sugarbaker DJ. Pleuropneumonectomy in the treatment of malignant pleural mesothelioma. Chest 1999;116:450S-4S. [PubMed]
- Weder W, Stahel RA, Bernhard J, et al. Multicenter trial of neo-adjuvant chemotherapy followed by extrapleural pneumonectomy in malignant pleural mesothelioma. Ann Oncol 2007;18:1196-202. [PubMed]
- Sharif S, Zahid I, Routledge T, et al. Extrapleural pneumonectomy or supportive care: Treatment of malignant pleural mesothelioma? Interact Cardiovasc Thorac Surg 2011;12:1040-5. [PubMed]
- von Meyenfeldt EM, Gooiker GA, van Gijn W, et al. The relationship between volume or surgeon specialty and outcome in the surgical treatment of lung cancer: a systematic review and meta-analysis. J Thorac Oncol 2012;7:1170-8. [PubMed]
- Chowdhury MM, Dagash H, Pierro A. A systematic review of the impact of volume of surgery and specialization on patient outcome. Br J Surg 2007;94:145-61. [PubMed]
- Rusch VW, Piantadosi S, Holmes EC. The role of extrapleural pneumonectomy in malignant pleural mesothelioma. A Lung Cancer Study Group trial. J Thorac Cardiovasc Surg 1991;102:1-9. [PubMed]
- Stewart DJ, Martin-Ucar AE, Edwards JG, et al. Extra-pleural pneumonectomy for malignant pleural mesothelioma: the risks of induction chemotherapy, right-sided procedures and prolonged operations. Eur J Cardiothorac Surg 2005;27:373-8. [PubMed]
- Cao CQ, Yan TD, Bannon PG, et al. A systematic review of extrapleural pneumonectomy for malignant pleural mesothelioma. J Thorac Oncol 2010;5:1692-703. [PubMed]
- Sugarbaker DJ, Flores RM, Jaklitsch MT, et al. Resection margins, extrapleural nodal status, and cell type determine postoperative long-term survival in trimodality therapy of malignant pleural mesothelioma: results in 183 patients. J Thorac Cardiovasc Surg 1999;117:54-63; discussion 63-5.. [PubMed]
- Sugarbaker DJ, Garcia JP. Multimodality therapy for malignant pleural mesothelioma. Chest 1997;112:272S-5S. [PubMed]
- Van Schil PE, Baas P, Gaafar R, et al. Trimodality therapy for malignant pleural mesothelioma: Results from an EORTC phase II multicentre trial. Eur Respir J 2010;36:1362-9. [PubMed]
- Weder W, Opitz I, Stahel R.. Multimodality strategies in malignant pleural mesothelioma. Semin Thorac Cardiovasc Surg 2009;21:172-6. [PubMed]
- Sugarbaker DJ, Norberto JJ. Multimodality management of malignant pleural mesothelioma. Chest 1998;113:61S-5S. [PubMed]
- Flores RM, Krug LM, Rosenzweig KE, et al. Induction chemotherapy, extrapleural pneumonectomy, and postoperative high-dose radiotherapy for locally advanced malignant pleural mesothelioma: a phase II trial. J Thorac Oncol 2006;1:289-95. [PubMed]
- Treasure T, Lang-Lazdunski L, Waller D, et al. Extra-pleural pneumonectomy versus no extra-pleural pneumonectomy for patients with malignant pleural mesothelioma: clinical outcomes of the Mesothelioma and Radical Surgery (MARS) randomised feasibility study. Lancet Oncol 2011;12:763-72. [PubMed]
- Weder W, Stahel RA, Baas P, et al. The MARS feasibility trial: conclusions not supported by data. Lancet Oncol 2011;12:1093-4. [PubMed]
- Hasani A, Alvarez JM, Wyatt JM, et al. Outcome for patients with malignant pleural mesothelioma referred for Trimodality therapy in Western Australia. J Thorac Oncol 2009;4:1010-6. [PubMed]
- Flores RM, Pass HI, Seshan VE, et al. Extrapleural pneumonectomy versus pleurectomy/decortication in the surgical management of malignant pleural mesothelioma: results in 663 patients. J Thorac Cardiovasc Surg 2008;135:620-6, 626.e1-3.
- Nakas A, Trousse DS, Martin-Ucar AE, et al. Open lung-sparing surgery for malignant pleural mesothelioma: the benefits of a radical approach within multimodality therapy. Eur J Cardiothorac Surg 2008;34:886-91. [PubMed]
- Maziak DE, Gagliardi A, Haynes AE, et al. Surgical management of malignant pleural mesothelioma: a systematic review and evidence summary. Lung Cancer 2005;48:157-69. [PubMed]
- Okada M, Mimura T, Ohbayashi C, et al. Radical surgery for malignant pleural mesothelioma: results and prognosis. Interact Cardiovasc Thorac Surg 2008;7:102-6. [PubMed]
- Pass HI, Kranda K, Temeck BK, et al. Surgically debulked malignant pleural mesothelioma: results and prognostic factors. Ann Surg Oncol 1997;4:215-22. [PubMed]
- Krug LM, Pass HI, Rusch VW, et al. Multicenter phase II trial of neoadjuvant pemetrexed plus cisplatin followed by extrapleural pneumonectomy and radiation for malignant pleural mesothelioma. J Clin Oncol 2009;27:3007-13. [PubMed]
- Ceresoli GL, Locati LD, Ferreri AJ, et al. Therapeutic outcome according to histologic subtype in 121 patients with malignant pleural mesothelioma. Lung Cancer 2001;34:279-87. [PubMed]
- Richards WG, Zellos L, Bueno R, et al. Phase I to II study of pleurectomy/decortication and intraoperative intracavitary hyperthermic cisplatin lavage for mesothelioma. J Clin Oncol 2006;24:1561-7. [PubMed]
- Price A.. What is the role of radiotherapy in malignant pleural mesothelioma? Oncologist 2011;16:359-65. [PubMed]
- Gordon W Jr, Antman KH, Greenberger JS, et al. Radiation therapy in the management of patients with mesothelioma. Int J Radiat Oncol Biol Phys 1982;8:19-25. [PubMed]
- Ball DL, Cruickshank DG. The treatment of malignant mesothelioma of the pleura: review of a 5-year experience, with special reference to radiotherapy. Am J Clin Oncol 1990;13:4-9. [PubMed]
- Davis SR, Tan L, Ball DL. Radiotherapy in the treatment of malignant mesothelioma of the pleura, with special reference to its use in palliation. Australas Radiol 1994;38:212-4. [PubMed]
- de Graaf-Strukowska L, van der Zee J, van Putten W, et al. Factors influencing the outcome of radiotherapy in malignant mesothelioma of the pleura--a single-institution experience with 189 patients. Int J Radiat Oncol Biol Phys 1999;43:511-6. [PubMed]
- Jenkins P, Milliner R, Salmon C.. Re-evaluating the role of palliative radiotherapy in malignant pleural mesothelioma. Eur J Cancer 2011;47:2143-9. [PubMed]
- Waite K, Gilligan D.. The role of radiotherapy in the treatment of malignant pleural mesothelioma. Clin Oncol (R Coll Radiol) 2007;19:182-7. [PubMed]
- Ung YC, Yu E, Falkson C, et al. The role of radiation therapy in malignant pleural mesothelioma: a systematic review. Radiother Oncol 2006;80:13-8. [PubMed]
- Chapman E, Garcia Dieguez M. Radiotherapy for malignant pleural mesothelioma (Review). Cochrane Database of Systematic Reviews 2010. Available online: http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD003880.pub4/pdf/standard (cited 15 Sept 2011).
- Gupta V, Mychalczak B, Krug L, et al. Hemithoracic radiation therapy after pleurectomy/decortication for malignant pleural mesothelioma. Int J Radiat Oncol Biol Phys 2005;63:1045-52. [PubMed]
- Stevens CW, Forster KM, Smythe WR, et al. Radiotherapy for mesothelioma. Hematol Oncol Clin North Am 2005;19:1099-115. [PubMed]
- Maasilta P.. Deterioration in lung function following hemithorax irradiation for pleural mesothelioma. Int J Radiat Oncol Biol Phys 1991;20:433-8. [PubMed]
- Kutcher GJ, Kestler C, Greenblatt D, et al. Technique for external beam treatment for mesothelioma. Int J Radiat Oncol Biol Phys 1987;13:1747-52. [PubMed]
- Gupta V, Krug LM, Laser B, et al. Patterns of local and nodal failure in malignant pleural mesothelioma after extrapleural pneumonectomy and photon-electron radiotherapy. J Thorac Oncol 2009;4:746-50. [PubMed]
- Baldini EH, Recht A, Strauss GM, et al. Patterns of failure after trimodality therapy for malignant pleural mesothelioma. Ann Thorac Surg 1997;63:334-8. [PubMed]
- Ahamad A, Stevens CW, Smythe WR, et al. Promising early local control of malignant pleural mesothelioma following postoperative intensity modulated radiotherapy (IMRT) to the chest. Cancer J 2003;9:476-84. [PubMed]
- Rice DC, Smythe WR, Liao Z, et al. Dose-dependent pulmonary toxicity after postoperative intensity-modulated radiotherapy for malignant pleural mesothelioma. Int J Radiat Oncol Biol Phys 2007;69:350-7. [PubMed]
- Allen AM, Czerminska M, Janne PA, et al. Fatal pneumonitis associated with intensity-modulated radiation therapy for mesothelioma. Int J Radiat Oncol Biol Phys 2006;65:640-5. [PubMed]
- Kristensen CA, Nottrup TJ, Berthelsen AK, et al. Pulmonary toxicity following IMRT after extrapleural pneumonectomy for malignant pleural mesothelioma. Radiother Oncol 2009;92:96-9. [PubMed]
- Allen AM, Schofield D, Hacker F, et al. Restricted field IMRT dramatically enhances IMRT planning for mesothelioma. Int J Radiat Oncol Biol Phys 2007;69:1587-92. [PubMed]
- Miles EF, Larrier NA, Kelsey CR, et al. Intensity-modulated radiotherapy for resected mesothelioma: the Duke experience. Int J Radiat Oncol Biol Phys 2008;71:1143-50. [PubMed]
- Chi A, Liao Z, Nguyen NP, et al. Intensity-modulated radiotherapy after extrapleural pneumonectomy in the combined-modality treatment of malignant pleural mesothelioma. J Thorac Oncol 2011;6:1132-41. [PubMed]
- Feigen M, Lee ST, Lawford C, et al. Establishing locoregional control of malignant pleural mesothelioma using high-dose radiotherapy and (18) F-FDG PET/CT scan correlation. J Med Imaging Radiat Oncol 2011;55:320-32. [PubMed]
- NCCN Guidelines for Treatment of Cancer by Site: Malignant Pleural Mesothelioma. National Comprehensive Cancer Network. Available online: http://www.nccn.org/professionals/physician_gls/f_guidelines.asp#site
- Low EM, Khoury GG, Matthews AW, et al. Prevention of tumour seeding following thoracoscopy in mesothelioma by prophylactic radiotherapy. Clin Oncol (R Coll Radiol) 1995;7:317-8. [PubMed]
- De Ruysscher D, Slotman B.. Treatment of intervention sites of malignant pleural mesothelioma with radiotherapy: a Dutch-Belgian survey. Radiother Oncol 2003;68:299-302. [PubMed]
- Lee C, Bayman N, Swindell R, et al. Prophylactic radiotherapy to intervention sites in mesothelioma: a systematic review and survey of UK practice. Lung Cancer 2009;66:150-6. [PubMed]
- Nagendran M, Pallis A, Patel K, et al. Should all patients who have mesothelioma diagnosed by video-assisted thoracoscopic surgery have their intervention sites irradiated? Interact Cardiovasc Thorac Surg 2011;13:66-9. [PubMed]
- Boutin C, Rey F, Viallat JR. Prevention of malignant seeding after invasive diagnostic procedures in patients with pleural mesothelioma. A randomized trial of local radiotherapy. Chest 1995;108:754-8. [PubMed]
- Bydder S, Phillips M, Joseph DJ, et al. A randomised trial of single-dose radiotherapy to prevent procedure tract metastasis by malignant mesothelioma. Br J Cancer 2004;91:9-10. [PubMed]
- O’Rourke N, Garcia JC, Paul J, et al. A randomised controlled trial of intervention site radiotherapy in malignant pleural mesothelioma. Radiother Oncol 2007;84:18-22. [PubMed]
- McAleer MF, Tsao AS, Liao Z. Radiotherapy in malignant pleural mesothelioma. Int J Radiat Oncol Biol Phys 2009;75:326-37. [PubMed]
- Standards for Providing Quality Palliative Care for all Australians. Canberra: Palliative Care Australia, 2005.
- Nowak AK, Stockler MR, Byrne MJ. Assessing quality of life during chemotherapy for pleural mesothelioma: feasibility, validity, and results of using the European Organization for Research and Treatment of Cancer Core Quality of Life Questionnaire and Lung Cancer Module. J Clin Oncol 2004;22:3172-80. [PubMed]
- Hillerdal G.. Malignant mesothelioma 1982: review of 4710 published cases. Br J Dis Chest 1983;77:321-43. [PubMed]
- Zimmermann C, Riechelmann R, Krzyzanowska M, et al. Effectiveness of specialized palliative care: a systematic review. JAMA 2008;299:1698-709. [PubMed]
- Temel JS, Greer JA, Muzikansky A, et al. Early palliative care for patients with metastatic non-small-cell lung cancer. N Engl J Med 2010;363:733-42. [PubMed]
- Waller A, Girgis A, Johnson C, et al. Implications of a needs assessment intervention for people with progressive cancer: impact on clinical assessment, response and service utilisation. Psychooncology 2012;21:550-7. [PubMed]
- Cancer pain relief. World Health Organization. 1986. Available from: http://www.who.int/iris/handle/10665/43944 (cited 15 Sept 2011).
- Ahmedzai SH, Baldwin DR, Currow DC. Supportive Care in Respiratory Disease. Second ed: Oxford University Press, 2012:400.
- Jackson MB, Pounder D, Price C, et al. Percutaneous cervical cordotomy for the control of pain in patients with pleural mesothelioma. Thorax 1999;54:238-41. [PubMed]
- Kanpolat Y, Savas A, Ucar T, et al. CT-guided percutaneous selective cordotomy for treatment of intractable pain in patients with malignant pleural mesothelioma. Acta Neurochir (Wien) 2002;144:595-9. [PubMed]
- Jennings AL, Davies AN, Higgins JP, et al. A systematic review of the use of opioids in the management of dyspnoea. Thorax 2002;57:939-44. [PubMed]
- Abernethy AP, Currow DC, Frith P, et al. Randomised, double blind, placebo controlled crossover trial of sustained release morphine for the management of refractory dyspnoea. BMJ 2003;327:523-8. [PubMed]
- Currow DC, McDonald C, Oaten S, et al. Once-daily opioids for chronic dyspnea: a dose increment and pharmacovigilance study. J Pain Symptom Manage 2011;42:388-99. [PubMed]
- Bausewein C, Booth S, Gysels M, et al. Non-pharmacological interventions for breathlessness in advanced stages of malignant and non-malignant diseases. The Cochrane Collaboration, 2011.
- Lee YC, Fysh ET. Indwelling pleural catheter: changing the paradigm of malignant effusion management. J Thorac Oncol 2011;6:655-7. [PubMed]
- Suzuki K, Servais EL, Rizk NP, et al. Palliation and pleurodesis in malignant pleural effusion: the role for tunneled pleural catheters. J Thorac Oncol 2011;6:762-7. [PubMed]
- Uronis HE, Currow DC, McCrory DC, et al. Oxygen for relief of dyspnoea in mildly- or non-hypoxaemic patients with cancer: a systematic review and meta-analysis. Br J Cancer 2008;98:294-9. [PubMed]
- Ben-Aharon I, Gafter-Gvili A, Paul M, et al. Interventions for alleviating cancer-related dyspnea: a systematic review. J Clin Oncol 2008;26:2396-404. [PubMed]
- Galbraith S, Fagan P, Perkins P, et al. Does the use of a handheld fan improve chronic dyspnea? A randomized, controlled, crossover trial. J Pain Symptom Manage 2010;39:831-8. [PubMed]
- Isenring E, Hill J, Davidson W, et al. Evidence-based practice guidelines for the nutritional management of patients receiving radiation therapy. Nutrition and Dietetics 2008;65:S1-S20.
- Hollen PJ, Gralla RJ, Liepa AM, et al. Adapting the Lung Cancer Symptom Scale (LCSS) to mesothelioma: Using the LCSS-Meso conceptual model for validation. Cancer 2004;101:587-95. [PubMed]
- Survey of mesothelioma patients and their carers. British Lung Foundation. 2009. Available online: www.blf.org.uk/Publication/Detail/mesothelioma (cited 24 Jan 2012).
- Lee SF, O’Connor MM, Chapman Y, et al. A very public death: dying of mesothelioma and asbestos-related lung cancer (M/ARLC) in the Latrobe Valley, Victoria, Australia. Rural Remote Health 2009;9:1183. [PubMed]
- Hughes N, Arber A.. The lived experience of patients with pleural mesothelioma. Int J Palliat Nurs 2008;14:66-71. [PubMed]
- Clayson H, Seymour J, Noble B.. Mesothelioma from the patient’s perspective. Hematol Oncol Clin North Am 2005;19:1175-90. [PubMed]
- Clinical practice guidelines for the psychosocial care of adults with cancer. Canberra: National Breast Cancer Centre 2003.
- Schofield P, Carey M, Love A, et al. ‘Would you like to talk about your future treatment options’? Discussing the transition from curative cancer treatment to palliative care. Palliat Med 2006;20:397-406. [PubMed]
- Schofield P, Diggens J, Charleson C, et al. Effectively discussing complementary and alternative medicine in a conventional oncology setting: communication recommendations for clinicians. Patient Educ Couns 2010;79:143-51. [PubMed]
- Hudson PL, Schofield P, Kelly B, et al. Responding to desire to die statements from patients with advanced disease: recommendations for health professionals. Palliat Med 2006;20:703-10. [PubMed]
- Kissane DW, Bylund CL, Banerjee SC, et al. Communication skills training for oncology professionals. J Clin Oncol 2012;30:1242-7. [PubMed]
- Uitterhoeve RJ, Bensing JM, Grol RP, et al. The effect of communication skills training on patient outcomes in cancer care: a systematic review of the literature. Eur J Cancer Care (Engl) 2010;19:442-57. [PubMed]
- Paul CL, Clinton-McHarg T, Sanson-Fisher RW, et al. Are we there yet? The state of the evidence base for guidelines on breaking bad news to cancer patients. Eur J Cancer 2009;45:2960-6. [PubMed]
- Dooley JJ, Wilson JP, Anderson VA. Stress and depression of facing death: Investigation of psychological symptoms in patients with mesothelioma. Aust J Psychol 2010;62:160-8.
- Carlson LE, Waller A, Mitchell AJ. Screening for distress and unmet needs in patients with cancer: review and recommendations. J Clin Oncol 2012;30:1160-77. [PubMed]
- Moore S, Darlison L, Tod AM. Living with mesothelioma. A literature review. Eur J Cancer Care (Engl) 2010;19:458-68. [PubMed]
- Palmer C, Thain C.. Strategies to ensure effective and empathetic delivery of bad news. Cancer Nursing Practice 2010;9:24-7.
- Moore S, Teehan C, Cornwall A, et al. ‘Hands of Time’: the experience of establishing a support group for people affected by mesothelioma. Eur J Cancer Care (Engl) 2008;17:585-92. [PubMed]
- Hawley R, Monk A.. Malignant mesothelioma: current practice and research directions. Collegian 2004;11:22-6.
- Abrahm JL. Palliative care for the patient with mesothelioma. Semin Thorac Cardiovasc Surg 2009;21:164-71. [PubMed]
- Chapman E, Hughes D, Landy A, et al. Challenging the representations of cancer pain: experiences of a multidisciplinary pain management group in a palliative care unit. Palliat Support Care 2005;3:43-9. [PubMed]
- Lebovits AH, Chahinian AP, Holland JC. Exposure to asbestos: psychological responses of mesothelioma patients. Am J Ind Med 1983;4:459-66. [PubMed]
- Ernst E, Cassileth BR. The prevalence of complementary/alternative medicine in cancer: a systematic review. Cancer 1998;83:777-82. [PubMed]
- Girgis A, Adams J, Sibbritt D.. The use of complementary and alternative therapies by patients with cancer. Oncol Res 2005;15:281-9. [PubMed]
- Schofield PE, Juraskova I, Butow PN. How oncologists discuss complementary therapy use with their patients: an audio-tape audit. Support Care Cancer 2003;11:348-55. [PubMed]
- Tasaki K, Maskarinec G, Shumay DM, et al. Communication between physicians and cancer patients about complementary and alternative medicine: exploring patients’ perspectives. Psychooncology 2002;11:212-20. [PubMed]
- Hong NJ, Wright FC, Gagliardi AR, et al. Examining the potential relationship between multidisciplinary cancer care and patient survival: an international literature review. J Surg Oncol 2010;102:125-34. [PubMed]
- Riedel RF, Wang X, McCormack M, et al. Impact of a multidisciplinary thoracic oncology clinic on the timeliness of care. J Thorac Oncol 2006;1:692-6. [PubMed]
- Leo F, Venissac N, Poudenx M, et al. Multidisciplinary management of lung cancer: how to test its efficacy? J Thorac Oncol 2007;2:69-72. [PubMed]
- Kendall M, Boyd K, Campbell C, et al. How do people with cancer wish to be cared for in primary care? Serial discussion groups of patients and carers. Fam Pract 2006;23:644-50. [PubMed]
- Gorman DR, Mackinnon H, Storrie M, et al. The general practice perspective on cancer services in Lothian. Fam Pract 2000;17:323-8. [PubMed]
- Mitchell GK. The role of general practice in cancer care. Aust Fam Physician 2008;37:698-702. [PubMed]
- Hall SE, Holman CD, Threlfall T, et al. Lung cancer: An exploration of patient and general practitioner perspectives on the realities of care in rural Western Australia. Aust J Rural Health 2008;16:355-62. [PubMed]
- Vinod SK, Delaney GP, Bauman AE, et al. Lung cancer patterns of care in south western Sydney, Australia. Thorax 2003;58:690-4. [PubMed]
- Olsson JK, Schultz EM, Gould MK. Timeliness of care in patients with lung cancer: A systematic review. Thorax 2009;64:749-56. [PubMed]
- Mooney K, King A.. Lung Cancer: The patient’s journey. J Thorac Oncol 2011;6:S30.
- Fischel RJ, Dillman RO. Developing an effective lung cancer program in a community hospital setting. Clin Lung Cancer 2009;10:239-43. [PubMed]
- Luxford T, Vinod S, Koh E, et al. Use of a validated assessment tool in lung cancer patients to identify symptom burden: the value of a nursing-led care coordination model. Asia Pac J Clin Oncol 2009;5:A168.
- Martin-Ucar AE, Waller DA, Atkins JL, et al. The beneficial effects of specialist thoracic surgery on the resection rate for non-small-cell lung cancer. Lung Cancer 2004;46:227-32. [PubMed]
- Simunovic M, Rempel E, Thériault ME, et al. Influence of hospital characteristics on operative death and survival of patients after major cancer surgery in Ontario. Can J Surg 2006;49:251-8. [PubMed]
- Bach PB, Cramer LD, Schrag D, et al. The influence of hospital volume on survival after resection for lung cancer. N Engl J Med 2001;345:181-8. [PubMed]
- Barocas DA, Mitchell R, Chang SS, et al. Impact of surgeon and hospital volume on outcomes of radical prostatectomy. Urol Oncol 2010;28:243-50. [PubMed]
- Chen CS, Liu TC, Lin HC, et al. Does high surgeon and hospital surgical volume raise the five-year survival rate for breast cancer? A population-based study. Breast Cancer Res Treat 2008;110:349-56. [PubMed]
- Sosa JA, Bowman HM, Gordon TA, et al. Importance of hospital volume in the overall management of pancreatic cancer. Ann Surg 1998;228:429-38. [PubMed]
- Finlayson EV, Birkmeyer JD. Effects of hospital volume on life expectancy after selected cancer operations in older adults: a decision analysis. J Am Coll Surg 2003;196:410-7. [PubMed]
- Rogers SO Jr, Wolf RE, Zaslavsky AM, et al. Relation of surgeon and hospital volume to processes and outcomes of colorectal cancer surgery. Ann Surg 2006;244:1003-11. [PubMed]
- Hillner BE, Smith TJ, Desch CE. Hospital and physician volume or specialization and outcomes in cancer treatment: importance in quality of cancer care. J Clin Oncol 2000;18:2327-40. [PubMed]
- Kim SY, Park JH, Kim SG, et al. Disparities in utilization of high-volume hospitals for cancer surgery: results of a Korean population-based study. Ann Surg Oncol 2010;17:2806-15. [PubMed]
- Lien YC, Huang MT, Lin HC. Association between surgeon and hospital volume and in-hospital fatalities after lung cancer resections: the experience of an Asian country. Ann Thorac Surg 2007;83:1837-43. [PubMed]
- Yan TD, Boyer M, Tin MM, et al. Extrapleural pneumonectomy for malignant pleural mesothelioma: outcomes of treatment and prognostic factors. J Thorac Cardiovasc Surg 2009;138:619-24. [PubMed]