Teaching an old dog new TRICS: re-evaluating transfusion triggers in high-risk cardiac surgery
Use of a restrictive or liberal red blood cell (RBC) transfusion trigger in cardiac surgery (CS) has been the subject of intense debate in the last decade (1-4). Multiple co-morbidities present in CS patients often necessitate perioperative transfusion of RBCs and other allogeneic blood products. CS procedures utilize over 20% of the blood supply in the United States (5). It is well known that allogeneic blood transfusion is associated with increased rates of hospital acquired infection, immunosuppression, circulatory overload, and mortality (6-8). On the other hand, there is some concern that restricting RBC transfusion may result in inadequate oxygen delivery to ischemic tissues, adversely affecting clinical outcomes (9).
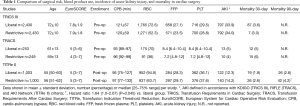
The Transfusion Requirements in Cardiac Surgery (TRICS) III trial is the first global and adequately powered study to compare a restrictive versus liberal RBC transfusion trigger in the high-risk cardiac surgical patients (n=5,243; Table 1) (3). Patients undergoing CS with cardiopulmonary bypass (CPB) were preoperatively randomized to a restrictive [hemoglobin (Hgb) <7.5 g/dL] or liberal transfusion trigger (Hgb <9.5 g/dL in the operating room and ICU, and Hgb <8.5 thereafter). The primary composite outcome of death, myocardial infarction, stroke, or new-onset renal failure requiring dialysis in the restrictive group was found to be non-inferior to the liberal group (11.4% restrictive vs. 12.5% liberal, 95% CI for non-inferiority −2.93–0.72; P<0.001). In elderly patients (≥75 years of age), outcomes were better with restrictive RBC transfusion.
Full table
Two previous randomized controlled trials in lower risk cardiac surgical patients showed conflicting results. The Transfusion Requirements After Cardiac Surgery (TRACS) trial randomized CS patients undergoing CPB to a liberal [Hematocrit (Hct) <30%] or restrictive (Hct <24%) transfusion trigger (n=502; Table 1) (2). The restrictive transfusion trigger was non-inferior to the liberal one for the primary end-points of severe morbidity and 30-day all-cause mortality (11% vs. 10% in liberal; P=0.85). Moreover, the number of RBCs transfused independently increased the risk for severe morbidity or 30-day mortality (HR for each transfused unit, 1.2; 95% CI, 1.1–1.4; P=0.002) regardless of the strategy implemented (2). Although these results supported a restrictive transfusion trigger, the generalizability of the study was limited by its single center design, exclusion of 50% patients after screening, and non-use of cell salvage or leukoreduced RBCs.
In contrast, the Transfusion Indication Threshold Reduction (TITRe2) trial was a multi-center study across the United Kingdom, which randomized CS patients with postoperative Hgb below 9 g/dL to a restrictive (Hgb <7.5 g/dL) or a liberal (Hgb <9 g/dL) transfusion trigger (n=2,003; Table 1) (4). The incidences of serious infection and ischemic events within 90 days were not different between the groups (35.1% restrictive vs. 33% liberal; P=0.30). However, an unforeseen increase in 90-day mortality was reported in the restrictive transfusion trigger group (4.2% vs. 2.6%; HR, 1.64; CI, 1.00–2.67; P=0.045) (4). The possibility of increased survival with liberal RBC transfusion caused some discord, with several letters to the editor criticizing the study for its substantial protocol non-adherence, post-operative enrollment, high rates of transfusion in both groups (63.7% restrictive vs. 94.9% liberal), and the small difference in Hgb nadir between groups (4,10-13).
TRICS III gives perioperative physicians some assurance that a restrictive transfusion trigger of 7.5 g/dL can be tolerated in high-risk CS patients with a high European System for Cardiac Operative Risk Evaluation (EuroSCORE), and a moderately long CPB duration of 120 min (Table 1) (4). Further, elderly patients may even benefit from more prudent/restrictive RBC transfusion. Managing patients off a single-fixed Hgb trigger during CS remains problematic in clinical practice though. Hemoglobin levels are dynamic during CPB, and the degree of hemodilution is in constant flux as blood is recycled form the surgical field. Also, our clinical observation is that cerebral oximetry values are maintained in some cases when Hgb levels are below 7 g/dL, while in other cases they fall at Hgb levels well above 7 g/dL, suggesting that hemoglobin concentration is merely one of many variables affecting organ perfusion.
Variability in CPB priming volume, use of cell salvage or hemoconcentration, antifibrinolytic drugs, and overall coagulation management also strongly influence the number of RBCs transfused during CS (14-17). The TRICS III protocol did not specify the use of cell salvage, but its intended use to increase Hgb levels often comes at the expense of worsened coagulopathy, post-operative bleeding, and residual circulating heparin (18). Many clotting factors and platelets are removed during centrifugation, and heparin, albeit a small amount, is contained in the salvaged blood. While anemic patients are more likely to receive RBC transfusions (19,20), the patients in TRICS III were not significantly anemic before surgery (mean Hgb 13.1 g/dL in restrictive versus 13.1 g/dL in liberal), which brings into question the study’s generalizability. Many busy CS centers have transfusion rates in the 10–30% range compared to the overall transfusion rate of 58% in TRICS III (21,22).
Further, the study’s treatment effect size was small, which may be from incomplete separation of Hgb values between groups (3). The nadir intraoperative Hgb value did not differ significantly between groups (8.7±1.6 in restrictive vs. 8.9±1.5 g/dL in liberal). Similarly, the mean post-operative Hgb was approximately 9 g/dL in the restrictive group and 10 g/dL in the liberal group, with significant overlap in the standard deviation. Compounding these factors, was the study protocol itself, which specified that patients in the liberal transfusion group have their transfusion trigger lowered from 9.5 to 8.5 g/dL once transferred to the ward. In fact, after transfer to the ward, there was only a 2% difference in the rate of RBC transfusion between groups compared to a 24% difference during surgery. Taking these elements into account, it is difficult to discern whether the two groups were all that different from each other in terms of blood oxygen delivery, which may have led to the study’s non-inferior result.
One final point to consider is that despite frequently cited concerns about impaired oxygen delivery with low blood hemoglobin level (23), hemoglobin concentration is in constant flux during CS due to its inverse relationship with intravascular volume. For this reason, some authors have suggested that total red cell mass may be a better surrogate for ischemic risk and physical fitness, since it refers to the body’s total content of RBCs (24,25). At present, no large randomized controlled trials have used red cell mass as a transfusion trigger.
In summary, we congratulate Mazer et al. for completing this truly global landmark study which attempted to solve an age-old clinical question about RBC transfusion. Completing a study of this size with excellent protocol adherence is a major logistical success and important data has been added to the RBC transfusion literature. Although the optimal transfusion trigger in CS patients remains uncertain, old dogs in transfusion need to keep learning new TRICS.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Carson JL, Brooks MM, Abbott JD, et al. Liberal versus restrictive transfusion thresholds for patients with symptomatic coronary artery disease. Am Heart J 2013;165:964-71.e1. [Crossref] [PubMed]
- Hajjar LA, Vincent JL, Galas FR, et al. Transfusion requirements after cardiac surgery: the TRACS randomized controlled trial. JAMA 2010;304:1559-67. [Crossref] [PubMed]
- Mazer CD, Whitlock RP, Fergusson DA, et al. Restrictive or liberal red-cell transfusion for cardiac surgery. N Engl J Med 2017;377:2133-44. [Crossref] [PubMed]
- Murphy GJ, Pike K, Rogers CA, et al. Liberal or restrictive transfusion after cardiac surgery. N Engl J Med 2015;372:997-1008. [Crossref] [PubMed]
- Spiess BD. Transfusion of blood products affects outcome in cardiac surgery. Semin Cardiothorac Vasc Anesth 2004;8:267-81. [Crossref] [PubMed]
- Blumberg N, Triulzi DJ, Heal JM. Transfusion-induced immunomodulation and its clinical consequences. Transfus Med Rev 1990;4:24-35. [Crossref] [PubMed]
- Spiess BD. Blood transfusion: the silent epidemic. Ann Thorac Surg 2001;72:S1832-7. [Crossref] [PubMed]
- Goodnough LT, Brecher ME, Kanter MH, et al. Transfusion medicine. First of two parts--blood transfusion. N Engl J Med 1999;340:438-47. [Crossref] [PubMed]
- Sardar P, Nairooz R, Dutu L, et al. Liberal versus restrictive transfusion strategy for patients with coronary artery disease. Am Heart J 2013;166:e25. [Crossref] [PubMed]
- Kramer RS, Groom RC, Hayes TE. Liberal or restrictive transfusion after cardiac surgery. N Engl J Med 2015;373:191-2. [PubMed]
- Mutneja HR, Arora S, Vij A. Liberal or restrictive transfusion after cardiac surgery. N Engl J Med 2015;373:190. [Crossref] [PubMed]
- Plumb JO, Grocott MP. Liberal or restrictive transfusion after cardiac surgery. N Engl J Med 2015;373:192-3. [PubMed]
- Reeves BC, Rogers CA, Murphy GJ. Liberal or restrictive transfusion after cardiac surgery. N Engl J Med 2015;373:193. [PubMed]
- Goldberg J, Paugh TA, Dickinson TA, et al. Greater volume of acute normovolemic hemodilution may aid in reducing blood transfusions after cardiac surgery. Ann Thorac Surg 2015;100:1581-7; discussion 1587. [Crossref] [PubMed]
- Gorlinger K, Dirkmann D, Hanke AA, et al. First-line therapy with coagulation factor concentrates combined with point-of-care coagulation testing is associated with decreased allogeneic blood transfusion in cardiovascular surgery: a retrospective, single-center cohort study. Anesthesiology 2011;115:1179-91. [PubMed]
- Mehaffey JH, Schubert SA, Gelvin MG, et al. A New Intraoperative Protocol for Reducing Perioperative Transfusions in Cardiac Surgery. Ann Thorac Surg 2017;104:176-81. [Crossref] [PubMed]
- Myles PS, Smith JA, Forbes A, et al. Tranexamic Acid in Patients Undergoing Coronary-Artery Surgery. N Engl J Med 2017;376:136-48. [Crossref] [PubMed]
- Shen S, Zhang J, Wang W, et al. Impact of intra-operative cell salvage on blood coagulation in high-bleeding-risk patients undergoing cardiac surgery with cardiopulmonary bypass: a prospective randomized and controlled trial. J Transl Med 2016;14:228. [Crossref] [PubMed]
- Weltert L, Rondinelli B, Bello R, et al. A single dose of erythropoietin reduces perioperative transfusions in cardiac surgery: results of a prospective single-blind randomized controlled trial. Transfusion 2015;55:1644-54. [Crossref] [PubMed]
- Scott DA, Tung HM, Slater R. Perioperative hemoglobin trajectory in adult cardiac surgical patients. J Extra Corpor Technol 2015;47:167-73. [PubMed]
- Dietrich W, Thuermel K, Heyde S, et al. Autologous blood donation in cardiac surgery: reduction of allogeneic blood transfusion and cost-effectiveness. J Cardiothorac Vasc Anesth 2005;19:589-96. [Crossref] [PubMed]
- Gross I, Seifert B, Hofmann A, et al. Patient blood management in cardiac surgery results in fewer transfusions and better outcome. Transfusion 2015;55:1075-81. [Crossref] [PubMed]
- Orlov D, O'Farrell R, McCluskey SA, et al. The clinical utility of an index of global oxygenation for guiding red blood cell transfusion in cardiac surgery. Transfusion 2009;49:682-8. [Crossref] [PubMed]
- Shander A, Ferraris VA. More or less? The Goldilocks Principle as it applies to red cell transfusions. Br J Anaesth 2017;118:816-9. [Crossref] [PubMed]
- Otto JM, Plumb JOM, Wakeham D, et al. Total haemoglobin mass, but not haemoglobin concentration, is associated with preoperative cardiopulmonary exercise testing-derived oxygen-consumption variables. Br J Anaesth 2017;118:747-54. [Crossref] [PubMed]


