Successful surgical treatment of massive spontaneous hemothorax due to intrathoracic secondary degeneration of a neurofibroma from mediastinal involvement of type 1 neurofibromatosis
Introduction
Neurofibromatosis type 1 (NF1) is an autosomal dominant disorder characterized by café-au-lait macules, variable neurofibromas, axillary and inguinal freckling, and Lisch nodules in the iris (1). Additionally, various vascular involvement and other manifestations have been reported (1-3). Spontaneous hemothorax in patients with NF1 is very rare, but is usually associated with vascular involvement (2). Hemothorax due to an accompanied mediastinal tumor, such as intrathoracic meningocele, has also been observed in NF1 cases (3,4). Herein, we present a rare case of a successful surgical treatment of a fatal hemothorax caused by intrathoracic cystic hemorrhagic degeneration of a neurofibroma associated with mediastinal involvement of NF1.
Case presentation
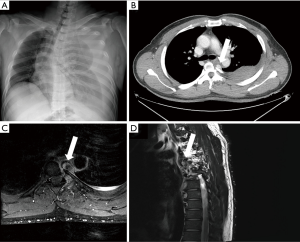
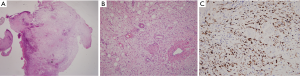
A 44-year-old man with NF1 was admitted to our emergency department for chest pain and dyspnea. The patient had typical cutaneous manifestation of NF1 (café au-lait spots and multiple various nodules). Physical examination revealed tachycardia (about 130 beats/minute), normal blood pressure (115/80 mmHg), and decreased breath sounds in the left lung field. Initial chest radiography showed a massive pleural effusion in the left hemithorax (Figure 1A). Pleural catheter drainage was performed and about 1,500 cc of blood was drained. Chest computed-tomography after drainage revealed a hemothorax and an approximately 2.6×4.0 cm2, soft tissue mass containing a well-enhanced oval lesion in the left posterior paravertebral space that abutted the descending aorta and the spinal canal at the fourth to sixth thoracic vertebra, suggesting a posterior mediastinal mass with bleeding (Figure 1B). However, because the patient had segmental osseous dysplasia of the adjacent vertebrae and due to adjacency of the mass to the spinal canal, magnetic resonance imaging (MRI) was performed, which revealed a posterior mediastinal mass combined with a hematoma with organization which consisted of proliferations of the spinal and the intercostal arteries with pseudoaneurysmal change. The MRI also revealed that the tumor had no relation to the spinal canal and no more active bleeding was found (Figure 1C,D). In addition, all image studies showed no spinal meningocele. We performed surgery to remove the tumor two days after the patient was admitted, with the intention of performing video-assisted thoracoscopic surgery (VATS). After removal of about 1,000 cc of the hematoma from the pleural cavity, the tumor was observed abutting the descending aorta at the level of the fourth to the sixth thoracic vertebra. There was no active bleeding, but diffuse bloody oozing from the tumor was observed. Because the tumor was diffusely infiltrative and looked like an aortic aneurysm, the origin could not be identified; however, it bled easily, so VATS became infeasible (Figure 2A). Thus, conversion to open thoracotomy was performed. The descending thoracic aorta was prepared for cross-clamping below and above the level of the tumor in case of inability to dissection of the tumor from the descending aorta. And then we successfully excised the tumor (Figure 2B). Gross findings showed that the tumor was grayish reddish to dark brown, with severe cystic degeneration and hemorrhagic change and rupture (Figure 2C). Microscopically, the excised specimen was non-encapsulated, hypocellular with myxoid background and contained Schwann cells, fibroblasts and mast cells. The surgical margin was free. Additionally, atypical and mitotic cells were absent (Figures 3A,B). The tumor tissue had S-100 protein-positive spindle cells with a biphasic pattern (Figure 3C). Accordingly, the tumor was diagnosed as a severe degeneration of a plexiform neurofibroma as mediastinal involvement of NF1. The patient had an uneventful postoperative course and was discharged on the 10th postoperative day. There was no recurrence of the tumor or hemothorax six months after surgery.

Comments
Thoracic involvement of NF1, or von Recklinghausen disease, is related to pulmonary and mediastinal manifestations of this multisystem disorder, which is the most common type of phakomatosis (1,4). Thoracic manifestations are usually related to neurofibromas involving the mediastinum and the chest wall, lateral thoracic meningocele, and vascular involvement (1,3). Other thoracic manifestations include focal thoracic scoliosis, enlarged neural foramina, posterior vertebral scalloping, and characteristic rib abnormalities (1,3). Hemothorax has been reported in patients with NF1 and is usually associated with vasculopathy due to vascular involvement of NF1 (2,3). The incidence of vascular manifestations in NF1 has been reported to be 3.6% (3). There are two main hypotheses to explain vasculopathy in NF1 (2,4): (I) Direct vascular invasion from adjacent tumors; (II) resulting in ischemia-induced weakening and vascular dysplasia with thickening and concomitant reduced strength of the vessel wall and aneurysm formation. The most commonly involved sites causing hemothorax in NF1 are the intercostal and subclavian arteries, which are associated with a high mortality rate of up to 30% (2-4). However, spontaneous hemothorax caused by a mediastinal tumor in NF1 is extremely rare (4,5). In this case, chest CT with contrast enhancement showed a soft tissue mass in the paravertebral region presenting as extensive infiltration around the mediastinal vessels and accompanied by focal scoliosis due to an eroding thoracic spine which was suggestive of segmental osseous dysplasia. Because an intrathoracic meningocele is associated with NF1 and the tumor location was adjacent to the spinal canal, MRI was performed to help establish a surgical plan. Accordingly, mediastinal involvement of NF1 brought about a mediastinal tumor and highly dilated and fragile vascular proliferations around the mass. Pathology findings revealed that the tumor was a plexiform neurofibroma with severe cystic hemorrhagic degeneration. The cause of the hemothorax was considered to be severe cystic hemorrhagic degeneration of the neurofibroma and the highly dilated and fragile vascular proliferations around the mass.
Initially, we planned to use VATS to excise the tumor but, because the tumor looked to be an aortic aneurysm and would bleed easily and was complicated by vessel fragility, VATS no longer seemed feasible, so we converted to open thoracostomy. The descending thoracic aorta was prepared for cross-clamping below and above the tumor, and then we successfully excised the tumor. Careful interpretation of the chest CT and MRI findings revealed that the hemothorax originated from the tumor. In addition, eventual spinal instability and paraplegia with trivial injuries in NF1 is known. However, spinal instability was not studied because there were no signs and symptoms about spinal instability.
To the best of our knowledge, this case report is the first to describe a massive hemothorax due to secondary degeneration of a neurofibroma from mediastinal involvement of NF1. Although the cause of the hemothorax in our case and in previous reported cases was NF1, none of the previous cases presented with a hemothorax due to a mediastinal neurofibroma from NF1, as in the present case. Thoracic surgeons should consider a neurofibroma from mediastinal involvement of NF1 can cause a hemothorax, and that surgical excision can be associated with severe hemorrhage due to vascular fragility.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Kresak JL, Walsh M. Neurofibromatosis: A Review of NF1, NF2, and Schwannomatosis. J Pediatr Genet 2016;5:98-104. [Crossref] [PubMed]
- Patrini D, Panagiotopoulos N, Pararajasingham J, et al. Etiology and management of spontaneous haemothorax. J Thorac Dis 2015;7:520-6. [PubMed]
- Yusuf AS, Pillai A, Menon SK, et al. Massive spontaneous hemothorax, giant intrathoracic meningocele, and kyphoscoliosis in neurofibromatosis type 1. J Surg Tech Case Rep 2014;6:33-6. [Crossref] [PubMed]
- Kaneda H, Saito T, Konobu T, et al. Chest wall bleeding with giant intrathoracic meningocele in neurofibromatosis type 1. Interact Cardiovasc Thorac Surg 2011;12:328-30. [Crossref] [PubMed]
- Ishibashi H, Takasaki C, Okubo K. Successful excision of a massive bleeding schwannoma by thoracoscopic surgery. Asian Cardiovasc Thorac Ann 2016;24:484-6. [Crossref] [PubMed]


