Serial chest CT findings of intravascular large B-cell lymphoma of the lungs
Intravascular large B-cell lymphoma (IVLBCL) is a rare variant of diffuse large B-cell lymphoma that is characterized histologically by proliferating mononuclear cells within the lumens of capillaries, venules, arterioles, and small arteries (1,2). This is an aggressive lymphoma with poor prognosis that contributes to delays in diagnosis because of the variable symptoms (1). IVLBCL of the lung is mostly detected at autopsy due to rarity (3). Chest computed tomography (CT) findings of IVLBCL include bilateral diffuse ground glass attenuation (GGA) in the whole lung, but this is nonspecific and can be seen in patients with diverse diseases, which can cause delayed diagnosis of this rapidly progressive and diffuse vascular tumorous condition (3,4). There are no reports about serial chest CT and 18F-fluorodeoxyglucose (FDG) positron-emission tomography-CT (PET-CT) findings of IVLBCL, which could help to differentiate this unusual vascular lymphoma from diffuse lung disease. We report a case of a patient with IVLBCL of the lung who underwent serial chest CT that showed aggravated bilateral diffuse GGA of the whole lung area. This unusual case emphasizes the usefulness of serial chest CT for accurate and timely diagnosis of IVLBCL before lung biopsy.
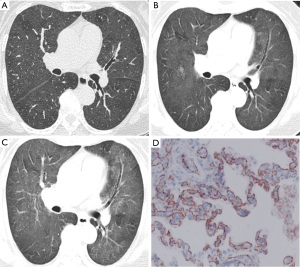
A 74-year-old female patient presented with a three-month history of dyspnea and cough. She was a housewife, non-smoker, and had no other disease history except asthma. Physical examination revealed that she had no skin lesions or neurologic abnormalities. Laboratory investigations revealed mild elevation of C-reactive protein (46.78 mg/L) and erythrocyte sedimentation rate (33 mm/h). Serum lactate dehydrogenase (LDH) was elevated at 2,160 IU/L. Pulmonary function test results were normal. Two months previously, the patient had undergone chest CT at a local hospital, and those scans showed bilateral diffuse GGA (Figure 1A). In our hospital, she again underwent chest CT, and the scans showed progressive bilateral GGA (Figure 1B). Despite conservative treatment for one month, her symptoms and chest CT findings showed progression (Figure 1C). She underwent bronchoscopy, but no definitive endobronchial lesions were found. Further, bronchial washing cytology showed only benign bronchial epithelial cells and chronic inflammatory cells. She then underwent PET-CT; mild 18F-FDG uptake was noted in both lungs, while strong uptake was noted in the spleen. Antibiotic and steroid treatment was initiated, but her general condition continued to deteriorate. Therefore, she underwent video-assisted thoracoscopic surgery (VATS) to take biopsies of the right upper and middle lung lobes. Light microscopic examination of the specimens revealed diffuse alveolar septal widening caused by large lymphoid cells filling the alveolar capillaries. The intravascular tumor cells were positive for the B-cell markers CD20 and CD31 staining confirmed that tumor cells were located predominantly in blood vessels (Figure 1D). The patient was diagnosed with malignant lymphoma, diffuse large B-cell, germinal center-like type. She underwent six cycles of chemotherapy (R-CHOP plus methotrexate). After chemotherapy, her general condition improved significantly and progressively without complications. Bilateral diffuse GGA on both lungs on chest CT scans improved, and FDG uptake by both the lung and spleen disappeared completely.
IVLBCL is characterized by the presence of lymphoma cells in the lumina of vessels in various organs. IVLBCL is defined as an extranodal B-cell lymphoma in the WHO classification system (1). The disease most commonly affects the skin and central nervous system, but can involve other organs, such as the lungs, liver, kidneys, and adrenal glands (1). Clinical symptoms of IVLBCL vary widely and are nonspecific. Obstruction of the small vessels of affected organs can contribute to this. Patients with IVLBCL of the lung might experience shortness of breath, hypoxemia, and sometimes pulmonary hypertension (3). The diagnosis of IVLBCL of the lung is especially difficult when skin lesions or neurological abnormalities are absent, because the clinical and radiographic findings are nonspecific, and the disease is very rare.
Chest CT findings of IVLBCL are diverse and include GGA, interlobular septal thickening, and thickening of bronchovascular bundles, suggesting lymphatic and hematological spread (5,6). Therefore, differential diagnoses should include subacute hypersensitivity pneumonitis, diffuse alveolar hemorrhage, nonspecific interstitial pneumonia, and neoplastic conditions. If diffuse GGA is present, IVLBCL should be included in differential diagnosis, and pathologic confirmation such as transbronchial lung biopsy (TBLB) or VATS should be performed proactively. TBLB and VATS are minimally invasive techniques, but bleeding, infections, postoperative pain, and recurrence at the port site are possible complications (7,8). Recently, several studies have reported that PET-CT is useful for diagnosis of IVLBCL (9,10). Although increased pulmonary FDG uptake also can be observed in patients with interstitial lung disease, which can mimic IVLBCL of lung, the intensity of FDG uptake in patients with idiopathic pulmonary fibrosis is lower than that in patients with IVLBCL (3).
In our case, the initial chest CT scan on admission showed bilateral diffuse GGA in the whole lung area. Serial chest CT revealed exacerbated extension and intensity of GGA without new consolidation, reticulation, traction bronchiectasis, or honeycombing in the whole lung area, especially the periphery of the lung, compared with the initial CT. These serial CT features might correlate with thickened alveolar septa and perivascular spaces because of distension of small vessels such as septal capillaries, venules, and arterioles filled with atypical lymphoid cells, rather than lymphatic channels (3,6). Furthermore, the absence of reticulation, traction bronchiectasis, honeycombing, or architectural distortion on CT images can rule out fibrotic interstitial lung disease (3). Therefore, these serial CT feature can help to differentiate IVLBCL from inflammation or interstitial lung disease.
In conclusion, although IVLBCL is difficult to diagnose, accurate and timely diagnosis is associated with a good prognosis and long-term survival. To date, the gold standard for diagnosis of IVLBCL is histopathology, which requires lung biopsy. Serial chest CT and PET-CT are non-invasive, and the findings described here can aid in diagnosis of IVLBCL of the lung.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Shimada K, Kinoshita T, Naoe T, et al. Presentation and management of intravascular large B-cell lymphoma. Lancet Oncol 2009;10:895-902. [Crossref] [PubMed]
- Chen Y, Ding C, Lin Q, et al. Primary intravascular large B-cell lymphoma of the lung: a review and case report. J Thorac Dis 2014;6:E242-5. [PubMed]
- Cha MJ, Lee KS, Hwang HS, et al. Pulmonary Intravascular Lymphomatosis: Clinical, CT, and PET Findings, Correlation of CT and Pathologic Results, and Survival Outcome. Radiology. 2016;280:602-10. [Crossref] [PubMed]
- Yamagata T, Okamoto Y, Ota K, et al. A case of pulmonary intravascular lymphomatosis diagnosed by thoracoscopic lung biopsy. Respiration 2003;70:414-8. [Crossref] [PubMed]
- Yu H, Chen G, Zhang R, et al. Primary intravascular large B-cell lymphoma of lung: a report of one case and review. Diagn Pathol 2012;7:70. [Crossref] [PubMed]
- Khojeini EV, Song JY. Intravascular large B-cell lymphoma presenting as interstitial lung disease. Case Rep Pathol 2014;2014:928065. [Crossref] [PubMed]
- Imperatori A, Rotolo N, Gatti M, et al. Peri-operative complications of video-assisted thoracoscopic surgery (VATS). Int J Surg 2008;6 Suppl 1:S78-81. [Crossref] [PubMed]
- Solaini L, Prusciano F, Bagioni P, et al. Video-assisted thoracic surgery (VATS) of the lung: analysis of intraoperative and postoperative complications over 15 years and review of the literature. Surg Endosc 2008;22:298-310. [Crossref] [PubMed]
- Morales-Oyarvide V, Mino-Kenudson M. High-grade lung adenocarcinomas with micropapillary and/or solid patterns: a review. Curr Opin Pulm Med 2014;20:317-23. [Crossref] [PubMed]
- Yamashita H, Suzuki A, Takahashi Y, et al. Intravascular large B-cell lymphoma with diffuse FDG uptake in the lung by 18FDG-PET/CT without chest CT findings. Ann Nucl Med 2012;26:515-21. [Crossref] [PubMed]


