Does the hybrid algorithm has real impact on long-term outcomes or should only be used as a valuable approach for CTO crossing?
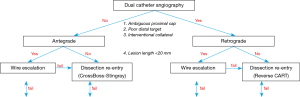
The hybrid algorithm to chronic total occlusion (CTO) percutaneous coronary intervention (PCI) (Figure 1) was published in 2012 and provided a systematic, angiography-based, approach to crossing coronary CTOs in 4 steps: (I) dual coronary angiography, which is essential to determine the characteristics of the lesion, especially occlusion length and the presence of collaterals appropriate for the retrograde approach; (II) systematic review of 4 lesions characteristics (proximal cap, lesion length, quality of distal vessel, and presence of interventional collaterals); (III) initial crossing strategy selection based on the aforementioned 4 parameters; and (IV) early change if the initially selected crossing strategy fails to achieve crossing within a reasonable period of time (1).
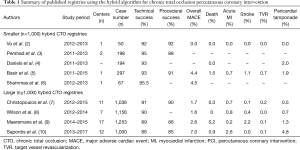
The hybrid algorithm provided a structured approach to CTO crossing and has been adopted by several operators in several countries with encouraging results (Table 1) (2-10). The Prospective Global Registry for the Study of Chronic Total Occlusion Intervention (Progress CTO) (7), the UK Hybrid CTO registry (8), and the Registry of Crossboss and Hybrid procedures in France, the Netherlands, Belgium and United Kingdom (RECHARGE) (9) registries have shown that application of the hybrid algorithm in CTO PCI can result in high procedural success (86–91%) and acceptable major adverse complication rates (1.6–2.6%). The OPEN-CTO Registry reported 86% procedural success rate in 1,000 consecutive CTO PCIs performed at 12 high volume US centers with an in-hospital major complication rate of 7.0% driven by clinical perforation (4.9%) (10). OPEN CTO demonstrated that successful CTO PCI was associated with significant improvement in angina, dyspnea and depression at 1 month follow-up, but longer-term outcomes after hybrid CTO PCI have received limited study.
Full table
One of the criticisms of the hybrid approach has been the recommendation for using antegrade dissection re-entry (ADR) for lesions ≥20 mm in length. ADR is best achieved using dedicated equipment (the CrossBoss catheter and the Stingray balloon and guidewire), which are not universally available and can be costly. Moreover, ADR could potentially increase the extent of dissection and stent length and predispose to complications, such as perforation. Alternative algorithms, such as the Asia Pacific CTO PCI algorithm (11), have been proposed, favoring antegrade wire escalation (AWE) instead of ADR. We recently presented and published the CrossBoss First randomized clinical trial that compared AWE with ADR in CTO PCI. CrossBoss First randomized 246 patients to CrossBoss (n=122) or wire escalation (n=124) at 11 US centers (12). Technical and procedural success were 87.8% and 84.1%, respectively and were similar in the two groups. Crossing time was similar: 56 (interquartile ranges, 33–93) min in the CrossBoss vs. 66 [36–105] min in the wire escalation group (P=0.323), as was as the incidence of procedural major adverse cardiovascular events (3.28% vs. 4.03%, P=1.000). However, on post hoc subgroup analyses, upfront use of the CrossBoss catheter was associated with shorter crossing time than wire escalation in CTOs due to in-stent restenosis {median 41 [23–58] vs. 66 [32–111] min, P=0.047}. Moreover, ADR was the final successful strategy in 22% of the AWE group patients, demonstrating the importance of ADR in achieving procedural success in CTO PCI. This is especially true for more complex occlusions, which are less likely to be crossed using AWE and more often require use of ADR or retrograde techniques (13,14).
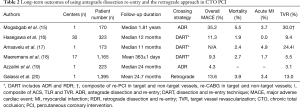
Another criticism of the hybrid approach has been a potential association of dissection/re-entry techniques with worse long-term outcomes, specifically higher rates of restenosis and reocclusion. This has been a concern for both ADR and retrograde dissection and re-entry (RDR) (Table 2) (15-20). Several studies have shown favorable long-term outcomes with use of ADR, but have been limited by small size and relatively short duration of follow-up.
Full table
Wilson et al. reported 1-year outcomes of 805 patients who underwent successful CTO revascularization using dissection and re-entry techniques (DART, both antegrade and retrograde) versus procedures that did not use dissection/re-entry (no DART group) at 7 UK centers between 2012 and 2014 as part of the UK hybrid registry. As has been previously reported (21), DART was used more frequently in more complex CTOs and was associated with longer stent length and larger contrast volume and radiation dose. The primary endpoint of the study was a composite of cardiac and non-cardiac death, myocardial infarction, unscheduled target vessel revascularization and target lesion revascularization and the mean follow-up time was 11.5±3.8 months. Follow-up angiography was scheduled in approximately one fourth of the patients (24%), mainly for distal vessel reassessment and was more frequently performed in the DART group (32% vs. 17%, P<0.001), which could potentially bias the results in favor of the no DART group. Overall, use of DART as the final CTO recanalization technique was not associated with higher rate of adverse event as compared with the no-DART group (10.3% vs. 7.0%, P=0.1). On multivariable analysis only lesions length (>25 mm) was independently associated with the incidence of adverse events at 12 months follow, suggesting that use of DART is safe.
Does this data mean that antegrade and retrograde crossing techniques should be frontline CTO crossing strategy? This may not necessarily be true. In the UK hybrid registry, 30-day major complication rates were numerally higher with more complex crossing techniques: AWE, 1.8%; retrograde wire escalation (RWE, 2.3%); ADR, 0.6%; and RDR, 2.9%. Moreover, retrograde strategies were associated with numerically higher rates of Ellis grade 3 perforation (AWE 1.0%, ADR 1.2%, RWE 2.3%, RDR 2.9%). Using retrograde techniques carries increased risk as compared with antegrade techniques (22) and should, therefore, be used with caution and when truly necessary to achieve recanalization.
Moreover, despite the reassurance provided by the UK hybrid registry long-term outcomes, when (antegrade or retrograde) dissection/re-entry is used, every attempt should be made to minimize the extent of dissection. In a recent meta-analysis extensive dissection and re-entry was associated with higher risk for subsequent adverse events (23). Extensive dissection re-entry, such as the subintimal tracking and re-entry (STAR) should only be used as bailout, because of significant side branch loss potentially leading to periprocedural myocardial infarction and/or high restenosis and reocclusion rates due to poor outflow. Similarly, new techniques are emerging for minimizing the extent of dissection in the reverse controlled antegrade and retrograde subintimal tracking (reverse CART) technique. For example the “directed” reverse CART (also called “contemporary reverse CART”) technique involves use of small antegrade balloon size and more active, intentional vessel tracking and penetration with a controllable retrograde wire within the CTO segment (24). In cases of extensive dissection it may be preferable to not implant stents, and just perform balloon angioplasty with stenting deferred until a later time, once the dissections have healed (investment procedure).
In summary, the results of the study by Wilson et al. provide reassurance that using (limited) DART techniques is unlikely to significantly impair the long-term outcomes after CTO PCI. Without DART techniques the success rate of CTO PCI would likely be significantly lower, especially in more complex CTOs. Mastering DART techniques remains important for CTO PCI operators and should be done progressively, starting with ADR, advancing to retrograde via septal collaterals or bypass grafts and finally to retrograde via epicardial collaterals.
Acknowledgements
None.
Footnote
Conflicts of Interest: ES Brilakis: consulting/speaker honoraria from Abbott Vascular, ACIST, Amgen, Asahi, CSI, Elsevier, GE Healthcare, Medicure, Medtronic, and Nitiloop; research support from Boston Scientific and Osprey. Board of Directors: Cardiovascular Innovations Foundation. Board of Trustees: Society of Cardiovascular Angiography and Interventions. P Tajti has no conflicts of interest to declare.
References
- Brilakis ES, Grantham JA, Rinfret S, et al. A percutaneous treatment algorithm for crossing coronary chronic total occlusions. JACC Cardiovasc Interv 2012;5:367-79. [Crossref] [PubMed]
- Vo MN, McCabe JM, Lombardi WL, et al. Adoption of the hybrid CTO approach by a single non-CTO operator: procedural and clinical outcomes. J Invasive Cardiol 2015;27:139-44. [PubMed]
- Pershad A, Eddin M, Girotra S, et al. Validation and incremental value of the hybrid algorithm for CTO PCI. Catheter Cardiovasc Interv 2014;84:654-9. [Crossref] [PubMed]
- Daniels DV, Banerjee S, Alaswad K, et al. Safety and efficacy of the hybrid approach in coronary chronic total occlusion percutaneous coronary intervention: The Hybrid Video Registry. Catheter Cardiovasc Interv 2018;91:175-9. [Crossref] [PubMed]
- Basir MB, Karatasakis A, Alqarqaz M, et al. Further validation of the hybrid algorithm for CTO PCI; difficult lesions, same success. Cardiovasc Revasc Med 2017;18:328-31. [Crossref] [PubMed]
- Shammas NW, Shammas GA, Robken J, et al. The learning curve in treating coronary chronic total occlusion early in the experience of an operator at a tertiary medical center: The role of the hybrid approach. Cardiovasc Revasc Med 2016;17:15-8. [Crossref] [PubMed]
- Christopoulos G, Karmpaliotis D, Alaswad K, et al. Application and outcomes of a hybrid approach to chronic total occlusion percutaneous coronary intervention in a contemporary multicenter US registry. Int J Cardiol 2015;198:222-8. [Crossref] [PubMed]
- Wilson WM, Walsh SJ, Yan AT, et al. Hybrid approach improves success of chronic total occlusion angioplasty. Heart 2016;102:1486-93. [Crossref] [PubMed]
- Maeremans J, Walsh S, Knaapen P, et al. The Hybrid Algorithm for Treating Chronic Total Occlusions in Europe: The RECHARGE Registry. J Am Coll Cardiol 2016;68:1958-70. [Crossref] [PubMed]
- Sapontis J, Salisbury AC, Yeh RW, et al. Early Procedural and Health Status Outcomes After Chronic Total Occlusion Angioplasty: A Report From the OPEN-CTO Registry (Outcomes, Patient Health Status, and Efficiency in Chronic Total Occlusion Hybrid Procedures). JACC Cardiovasc Interv 2017;10:1523-34. [Crossref] [PubMed]
- Harding SA, Wu EB, Lo S, et al. A New Algorithm for Crossing Chronic Total Occlusions From the Asia Pacific Chronic Total Occlusion Club. JACC Cardiovasc Interv 2017;10:2135-43. [Crossref] [PubMed]
- Karacsonyi J, Tajti P, Rangan BV, et al. Randomized Comparison of a CrossBoss First Versus Standard Wire Escalation Strategy for Crossing Coronary Chronic Total Occlusions: The CrossBoss First Trial. JACC Cardiovasc Interv 2018;11:225-33. [Crossref] [PubMed]
- Danek BA, Karatasakis A, Karmpaliotis D, et al. Use of antegrade dissection re-entry in coronary chronic total occlusion percutaneous coronary intervention in a contemporary multicenter registry. Int J Cardiol 2016;214:428-37. [Crossref] [PubMed]
- Maeremans J, Dens J, Spratt JC, et al. Antegrade Dissection and Reentry as Part of the Hybrid Chronic Total Occlusion Revascularization Strategy: A Subanalysis of the RECHARGE Registry (Registry of CrossBoss and Hybrid Procedures in France, the Netherlands, Belgium and United Kingdom). Circ Cardiovasc Interv 2017;10:e004791. [Crossref] [PubMed]
- Mogabgab O, Patel VG, Michael TT, et al. Long-term outcomes with use of the CrossBoss and stingray coronary CTO crossing and re-entry devices. J Invasive Cardiol 2013;25:579-85. [PubMed]
- Hasegawa K, Tsuchikane E, Okamura A, et al. Incidence and impact on midterm outcome of intimal versus subintimal tracking with both antegrade and retrograde approaches in patients with successful recanalisation of chronic total occlusions: J-PROCTOR 2 study. EuroIntervention 2017;12:e1868-e73. [Crossref] [PubMed]
- Amsavelu S, Christakopoulos GE, Karatasakis A, et al. Impact of Crossing Strategy on Intermediate-term Outcomes After Chronic Total Occlusion Percutaneous Coronary Intervention. Can J Cardiol 2016;32:1239.e1-.e7.
- Maeremans J, Avran A, Walsh S, et al. One-Year Clinical Outcomes of the Hybrid CTO Revascularization Strategy After Hospital Discharge: A Subanalysis of the Multicenter RECHARGE Registry. J Invasive Cardiol 2018;30:62-70. [PubMed]
- Azzalini L, Dautov R, Brilakis ES, et al. Procedural and longer-term outcomes of wire- versus device-based antegrade dissection and re-entry techniques for the percutaneous revascularization of coronary chronic total occlusions. Int J Cardiol 2017;231:78-83. [Crossref] [PubMed]
- Galassi AR, Sianos G, Werner GS, et al. Retrograde Recanalization of Chronic Total Occlusions in Europe: Procedural, In-Hospital, and Long-Term Outcomes From the Multicenter ERCTO Registry. J Am Coll Cardiol 2015;65:2388-400. [Crossref] [PubMed]
- Christopoulos G, Wyman RM, Alaswad K, et al. Clinical Utility of the Japan-Chronic Total Occlusion Score in Coronary Chronic Total Occlusion Interventions: Results from a Multicenter Registry. Circ Cardiovasc Interv 2015;8:e002171. [Crossref] [PubMed]
- Karmpaliotis D, Michael TT, Brilakis ES, et al. Retrograde coronary chronic total occlusion revascularization: procedural and in-hospital outcomes from a multicenter registry in the United States. JACC Cardiovasc Interv 2012;5:1273-9. [Crossref] [PubMed]
- Karatasakis A, Danek BA, Karacsonyi J, et al. Mid-term outcomes of chronic total occlusion percutaneous coronary intervention with subadventitial vs. intraplaque crossing: A systematic review and meta-analysis. Int J Cardiol 2018;253:29-34. [Crossref] [PubMed]
- Matsuno S, Tsuchikane E, Harding SA, et al. Overview and Proposed Terminology for the Reverse Controlled Antegrade and Retrograde Tracking (reverse CART) Techniques. EuroIntervention 2018. [Epub ahead of print].