Asthma in the context of global alliance against respiratory diseases (GARD) in Turkey
Introduction
The Global Alliance against Chronic Respiratory Diseases (GARD) is a voluntary alliance that is assisting World Health Organization (WHO) in the task of addressing non-communicable diseases (NCDs) at country level. The GARD approach was initiated in 2006 (1,2). GARD Turkey is the first comprehensive program developed by a government with all stakeholders of the country. GARD Turkey Project is the National Control Program of Turkish Ministry of Health on chronic airway disease (asthma and COPD) (3,4). This paper describes the segment of the program on asthma.
The initiation and the development of GARD Turkey
Turkish Thoracic Society (TTS) has become a GARD member in 2005. In 2007, Turkish Allergy and Clinic Immunology Society has joined the organization as the second member of Turkey. As a major national program, the GARD Turkey Project is the first of this nature involving bringing the Turkish Ministry of Health (MoH) and a group of non-governmental organizations (NGO) including TTS and 64 organizations together in joint management. The integrated approach of GARD has also been maintained by the GARD Turkey Project. The Turkish MoH has decided to apply this national control program in conformity with other NCD action plans, some of which have been finalized (i.e., cardiovascular diseases, obesity and tobacco control programs). The local city councils of GARD Turkey have been established in 81 province centers and by laws have been prepared. Local councils are composed of the local representatives of the GARD Turkey parties in each province and chaired by the director of MoH or vice in that particular province and responsible for the management and coordination of the activities of each group at local level. There are five working groups of the program, whose activities are explained below (3,5). Under the program executive committee and the general assembly’s work, conducting meetings of working groups and reporting, data collection and completion of stakeholder feedback, training and joint activities with Turkish Thoracic Society like the use of awareness materials across the country carried out by the Ministry of health provision.
In Turkey, GARD activities began with the formation of a committee by the TTS who undertook a situation analysis on the burden of chronic respiratory diseases. By using the data reported by Turkish MoH in the Turkey Health Report and National Burden of Chronic Diseases, the committee confirmed that chronic airway diseases including COPD and asthma represent a very important burden of disease in Turkey (6,7).
Burden of asthma in Turkey
In Turkey, there is a lack of nationwide studies in both asthma and rhinitis. Most of the studies concentrated on the prevalence of asthma in both children and adults from different regions of the country. In general, three different methodologies have been used for the epidemiological studies of childhood asthma in Turkey (8): (I) “The International Study of Asthma and Allergies in Childhood (ISAAC)” questionnaire; (II) the ATS questionnaire adapted by Turkish National Society of Allergy and Clinical Immunology; and (III) Aberg’s questionnaire. For the adult studies, a majority of studies used the “European Community Respiratory Health Survey (ECRHS)” questionnaire. These studies showed that, depending on the geographical region, the asthma prevalence varies between 2–15% in children and 2–5% in adults (8). Asthma is among the top 20 diseases causing high mortality in Turkey, and it is ranked as 20th in males residing in urban areas, and 17th in females in rural areas (8).
Childhood infections, passive smoking, family history of asthma and allergies, premature birth, living at lower altitudes and higher atmospheric pressure may increase the risk of asthma. The data suggest that, as in most countries, asthma is more common in males during childhood and among females after adolescence. Successive studies using the same methodology suggest that the prevalence of asthma is increasing in Istanbul, Izmir and Adana but in the latter province has been more constant over several years (8).
GARD Turkey action plans
“Turkish Chronic Respiratory Diseases Prevention and Control Program and Action Plan” which ran from 2009 to 2013 was the first of this nature involving the MoH and an NGO (the TTS) in joint management of a major national program. The goals of the project are in line with the GARD action plan to prevent and control chronic respiratory diseases, to reduce mortality and morbidity from chronic respiratory diseases, and also to reduce the social and economic burden of these diseases (8). Since 2009 the program has been conducted successfully with many achievements (5). The latest updated action plan for 2014–2017 has also been published in Turkish (9).
Working groups (WG)
WG1: monitoring the chronic diseases and the control program evaluation
WG1 of the control program is responsible for monitoring the chronic respiratory diseases and the evaluation of the control program. WG1 had targets such as collection of COPD and asthma specific prevalence and incidence data. They aimed to define the methods for obtaining reliable and comparable data as well as to monitor the disease burden by defined intervals. Establishment of a unit for collecting analyzing and reporting data within MoH was one of their important plans. They had a workshop for renovating the recording system, collecting the current data and planning a new data collection system throughout the country. They conducted a survey for chronic diseases and risk factors in Turkey (10). This was a cross-sectional survey carried out with the aim of collecting continuous data model on NCD and their common risk factors. It was carried out with a unique design implemented for the first time in our country. A sample from the population registered in all family physicians in Turkey was selected and data were recorded to Family Medicine Information System by family physicians. The survey included information about chronic disease and their leading risk factors as well as biochemical analyses in blood and urine, anthropometric measurements (such as height, weight, waist circumference, hip circumference) and pulmonary function tests (PFT). In this national survey, data were collected quickly and cost-efficiently because we used Family Medicine Information system. As a result of this survey; the age and sex standardized doctor diagnosed asthma prevalence was 4.5% (2.8% in male and 6.2 in female). This was in agreement with the studies conducted before by using ECRHS questionnaire (8-10). The prevalence of asthma was higher among female in all age groups. It was higher in rural areas than in urban areas and in central Anatolia, Western Black Sea, Eastern Black sea and western Anatolia than other regions (10). Almost 60% of the doctor diagnosed asthma patients used regular medication. Study showed that asthma is prevalent in Turkey and accessibility to treatment should be increased in asthma patients (10).
Low level of asthma control is a significant health problem in Turkey which is similar to the other parts of the world (11-17). It is also an economical problem as mean annual direct medical costs of asthma may be as high as $1,465.7 per person with the medication cost being the major element (81%) of the total direct cost (18). The direct cost of the asthma attack was reported as 214.9 euro per attack. The cost of severe attacks was reported as 308.2 euro which was significantly higher than moderate and mild attacks (19).
Asthma insights and reality in Turkey (AIRET) study (16) was conducted in 2005 with a methodology similar to the previous AIR surveys and a representative, urban population from 15 different cities was screened. 8350 houses were included. Recruitment continued until the required number of asthmatic patients with a valid interview was achieved in each area, resulting in a total sample of 400 asthmatic patients. AIRET Study demonstrated that only 1.25% of the asthma cases were able to meet all GINA criteria of asthma control. About three-quarters of children and 90% of adults were experiencing daytime symptoms during the last 4 weeks and two thirds of both children and adults were having night awakenings. Almost half the patients required an urgent/emergency visit and almost 60% of both children and adults required a rescue medication more than two times a week during the last month. Although GINA guidelines recommend no limitation of activities, social life was affected in almost 80% of our asthmatics. Only 37.5% of children and 30.3% of adults with persistent disease (as defined in GINA guidelines) were using daily preventative drugs. Of these, 90% of adults and 22% of children were current users of inhaled corticosteroids (16,20).
A cross-sectional multicenter survey in tertiary level hospitals in Turkey one year after AIRET Study was conducted in 2,336 patients with asthma, from 28 tertiary hospitals demonstrated that 51.5% of the patients were “controlled” [Asthma Control Test (ACT) ≥20] and 48.5% was defined as “uncontrolled” (ACT <20) (16). Thirty-two percent of study subjects reported using reliever medication more than two times a week. The rate of patients with nighttime symptoms at least once in a week was 28.3%, and 69.4% of the subjects described daily symptoms. Use of inhaled corticosteroids in any form was reported by 74.1% of patients. Almost one third (31%) of the subjects were prescribed fixed combination therapy (17).
Published national asthma management and prevention guidelines in 2000 and 2009 aimed to standardize asthma management and increase asthma control (21). But the results of the year 2011 comparing the data of asthma control test via text messaging and via paper-pencil also demonstrated the low control level of asthma patients in Turkey (22). At the baseline visit, the asthma control for texting patients were as totally controlled in 21.05%, partly controlled in 43.15%, and uncontrolled in 35.80%. For the paper-and-pencil group, physicians rated asthma as totally controlled in 22.30%, partly controlled in 38.60%, and uncontrolled in 39.10% (22).
Effective management of asthma requires the development of a partnership between the patient and his or her health care professionals. But it was demonstrated that Istanbul pharmacy workers have limited knowledge about asthma and inhaler devices (23). Yildiz demonstrated that the asthma control could increase with repeated checking of patients’ inhaler techniques, and with correction of the errors (24).
Newly published national, multicenter, prospective, observational study (ASKO Study) conducted in 122 secondary and tertiary centers with 1,116 asthma patients followed-up for 12 months demonstrated that patients are frequently over-treated and patients do not adhere to visits as expected (24). Total control rate improved and reached to 52% at 3 to 6 months and to 63% by the end of 12 months. Among patients with high treatment compliance, the percentage of patients with uncontrolled disease was only 5% (25).
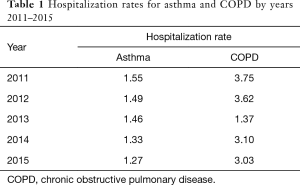
GARD educational activities may have contributed a slow decrease for asthma hospitalization (Table 1) (26).
Full table
WG2: awareness and advocacy
WG2, which is responsible for advocacy and awareness of the program and tried to introduce the program to health professionals, educational units and to public. This group conducted two studies regarding the awareness of asthma and COPD among public and health care professionals (27), 8,527 people from the rural and urban areas were reached to investigate the awareness of asthma and COPD among public (27). They completed a questionnaire which was prepared to evaluate disease knowledge for COPD and asthma. 49.6% of the subjects knew that COPD is a lung disease, 51.1% indicated that smoking is the most important risk factor for COPD and 48% identified quitting smoking as the most important preventive measure. Every other person had baseline knowledge on COPD. However, only 25.2% knew that there are treatment options for COPD. 51.1% knew asthma is a genetic disease and 58% said it is not an infectious disease. Eighty percent of subjects said asthma can be seen in all age groups. Only 27% answered as “No” to the question asking ‘Are asthma medications caused drug dependency’ while 55.2% said “They do not know”. In conclusion, awareness of COPD and asthma seem to be insufficient among Turkish people (27).
Turkish Statistical Institute randomly selected 680 doctors, and of these 84% described asthma as airway obstruction. Dyspnea was reported as the most common symptom of asthma (78.8%) and inspiratory rhonchi was reported as the most common physical exam finding (42.3%). Around 50% of doctors thought impairment of PFT was important for diagnosis and evaluation of severity of asthma while 24.2% thought physical exam was more important. When treatment options were evaluated 87.6% chose inhaled treatment for asthma (28).
They have prepared standard educational material for patients and public as well as the materials for awareness and advocacy of GARD Turkey Project and diseases in a workshop. These standard materials are now being used throughout the whole country. They did public educational activities on COPD, asthma, pulmonary rehabilitation, inhaler devices by short films, posters, booklets, media and as world day activities. 1.8 million people were reached by showing digital ads on digital news websites. Another 1.8 million people were reached by newspaper notices. By using all of these mediums approximately 25 million people were educated.
WG3: prevention of the development of disease
WG3 which is responsible for preventing the development of disease aimed to reduce smoking, environmental smoking, indoor air pollution, outdoor air pollution, occupational risk factors, allergen exposure and prevention and management of childhood infections and also generalizing physical activities and healthy nutrition. An expert panel prepared and published a report entitled “Evaluation of indoor and outdoor pollution and climate change in respect of the control of chronic respiratory diseases” (29). A workshop for indoor—outdoor pollution and climate change has taken place in June 2014 and position report and action plan have been published (29).
WG4: early detection of diseases and prevention of progress
WG4 which is responsible for early detection of diseases and prevention of progress and increasing awareness of early detection among public and health professionals aimed to availability and expand the use of spirometry. They prepared a paper on the standards of spirometry (30). They aimed to provide easy access to healthcare services, medicine and treatment equipment. They had plans for proper recording and monitoring. Decreasing allergen burden was also aimed by this group.
WG4 has been considered as advisory board for drug and social security system. They prepared the curriculum and educational materials of educators for primary care settings about asthma, COPD, home care and pulmonary rehabilitation, as well as tobacco control. This curriculum has been prepared in a workshop where physicians and expert academicians from three levels of health centers attended and teaching slide sets as well as video recordings have been standardized accordingly.
As part of the control program to raise the awareness of health personnel and community, and increase health literacy, informative meetings were held about COPD with 67,186 health personnel and 670,757 community members, about asthma with 60,564 health personnel and 571,847 community members, about pulmonary rehabilitation with 31,108 health personnel and 160,776 community members. In addition, a total of 633 press conferences, 522 radio-TV speeches, 2,887 news broadcasts (internet, newspapers, magazines, etc.), distribution of 2,514,830 printed materials (posters, brochures, etc.), 21,084 visual materials (cd, video, billboard etc.), 587 marches, 114,179 tree plantings (for the purpose of forming GARD forest), 4,709 stands, 119,213 spirometry measurements were carried out and information about awareness was regularly shared via social media (Facebook, Twitter, Instagram etc.). However, there is a need for studies to assess the contribution of existing studies to attitudes and behavioral changes both in health care personnel and in the community. Training module, educator guide and exhibitor guide of asthma and COPD diagnosis and treatment for primary care physicians has been prepared. In accordance with the prepared educational guidelines first 130 pulmonary diseases specialist trainers have been trained on asthma and COPD early diagnosis and appropriate treatment. 15,598 primary care physicians (PCP) have been educated face to face by these trainers using the same structured materials. On-line educational module, have been prepared on asthma and COPD diagnosis and treatment, that has been a must to be taken for 17,000 PCP.
From 11 different cities, 1,817 and 1,788 primary health care physicians attended to the asthma and COPD face to face educations, respectively. Pre and post-tests were applied to the participants to measure the effectiveness of the education. Ratio of correct answers to asthma questions before and after the educational course were 42.0% and 71.3%, respectively (31).
WG5: effective treatment of the diseases and prevention of complication development
WG5 is responsible for effective treatment of the diseases and prevention of complications, education of patients and health care professionals about appropriate treatment. They aimed to expand home care services and pulmonary rehabilitation services. One of their targets was also to provide easy access to medicine and treatment equipment as well as proper recording and monitoring. They had a workshop for homecare integrated with all home care and rehabilitation programs of other NCDs and published a report (32). Through their efforts important changes were made in the reimbursement rules of pulmonary rehabilitation and home care.
Pediatric coordination group has been established and they made pediatric action plans for each WG. The National control plan has been updated and pediatric data have added and published for 2014–2017 in conformity with WHO action Plan (9).
International activities
The Project has been referred in the GARD International Country report paper published recently (33). The launch of national GARD-led initiatives and a variety of projects in partnership with government health departments, as exemplified by GARD’s role in Turkey, Portugal and Italy were mentioned in that paper.
GARD Turkey Project has been accepted by European Innovation Partnership on Active and Healthy Aging (EIP on AHA). AIRWAYS ICPs was initiated by Area 5 of the Action Plan B3 of the EIP on AHA. All stakeholders are involved (health and social care, patients, and policy makers). The objective of AIRWAYS-ICPs is to launch a collaboration to develop multi-sectoral care pathways for chronic respiratory diseases in European countries and regions. (34,35). A patient-centered mobile application (Allergy Diary) (App for iOS and Android smartphones) has been developed and uses VAS scores and allows the daily assessment of rhinitis and asthma control by patients themselves. It is available for free download in 21 countries and 16 languages and has already been tested by over 8,000 users of all ages (17) GARD Turkey has been one of the partners of this program (36).
Conclusions
The greatest achievement of GARD is its ability to establish collaborative partnerships and develop a common vision with a large number of parties including professional medical societies, patient organizations, NGOs, governments and, of course, WHO in order to address chronic respiratory diseases and allergy worldwide as we have experienced in Turkey. Preventing and controlling CRDs, and keeping them on the global health agenda, will require the ongoing efforts of all involved in GARD. We believe GARD Turkey is a good example of GARD countries in many aspects.
Acknowledgements
The source for funding of GARD Turkey activities over the last 10 years has been multiple, including: (I) voluntary “in kind” contribution of the coordinators and other leaders of GARD, GINA and ARIA initiatives; (II) voluntary and “in kind” contributions of the Ministry of Health Turkey; (III) voluntary and “in kind” contributions of Turkish Thoracic Society and Turkish Society of Allergy and Clinical Immunology; (IV) unrestricted project-based contributions from the private companies (Boehringer Ingelheim Turkey, GSK Turkey, Novartis Turkey) to Turkish Thoracic Society for GARD Turkey.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Bousquet J, Khaltaev N. Editors. Global surveillance, prevention and control of chronic respiratory diseases. A comprehensive approach. Geneva: World Health Organization, 2007:p146.
- Global Alliance against Chronic Respiratory Diseases Action Plan 2008-2013. Geneva: World Health Organization, 2008:p28.
- Yorgancioğlu A, Türktaş H, Kalaycı Ö, et al. The WHO global alliance against chronic respiratory diseases in Turkey (GARD Turkey). Tuberk Toraks 2009;57:439-52. [PubMed]
- Yorgancıoğlu A, Yardım N, Ergün P, et al. Integration of GARD Turkey national program with other non-communicable diseases plans in Turkey. Tuberk Toraks 2010;58:213-28. [PubMed]
- GARD Turkey website. Available online: www.gard.org.tr
- Ünüvar N, Mollahaliloğlu S, Yardım N. Turkey Burden of Diseases Study 2004, Republic of Turkey Ministry of Health Refik Saydam Hygiene Center Pesidency School of Public Health, Ankara, Aydoğdu Matbaacılık 2007, 56 p. Available online: http://ekutuphane.sagem.gov.tr/kitaplar/turkey_burden_of_disease_study.pdf
- Yardım N, Mallahaliloğlu S, Hülür Ü, et al. Health at Glance Turkey 2007, Ankara, Ministry of Health Refik Saydam Hygiene Center Presidency School of Public Health, 2008, 291p. Available online https://sbu.saglik.gov.tr/Ekutuphane/kitaplar/200803041111400_HEALTHATGALANCE.pdf
- Kronik Hava Yolu Hastalıklarını Önleme ve Kontrol Programı (2009-2013) T.C. Sağlık Bakanlığı Temel Sağlık Hizmetlerİ Genel Müdürlüğü, Ankara, Anıl Matbaacılık, 2009, 134p. Available online: http://www.ssuk.org.tr/eski_site_verileri/pdf/KHH_OnlemeKontrolEylemPlani.pdf
- Kronik Hava Yolu Hastalıklarını Önleme ve Kontrol Programı (2014-2017) T.C. Sağlık Bakanlığı, Türkiye Halk Sağlığı Kurumu, Ankara, Anıl Matbaa Ltd Sti, 2014, 128p. Available online: https://sbu.saglik.gov.tr/Ekutuphane/Yayin/507
- Ünal B, Ergör G, Editors. Chronic diseases risk foctors survey in Turkey. Republic of Turkey, Ministry of Health, Public Health Agency of Turkey. Ankara, 322p. Available online: https://sbu.saglik.gov.tr/Ekutuphane/Yayin/463
- Rabe KF, Vermiere PA, Soriano JB, et al. Clinical management of asthma in 1999: the asthma insights and reality in Europe (AIRE) study. Eur Respir J 2000;16:802-7. [Crossref] [PubMed]
- Lai CK, De Guia TS, Kim YY, et al. Asthma control in the Asia-Pacific region: the asthma insights and reality in Asia-Pacific study. J Allergy Clin Immunol 2003;111:263-8. [Crossref] [PubMed]
- Adams RJ, Fuhlbrigge A, Guilbert T, et al. Inadequate use of asthma medication in the United States: results of Asthma in America national population survey. J Allergy Clin Immunol 2002;110:58-64. [Crossref] [PubMed]
- Adachi M, Morikawa A, Ishihara K. Asthma insights & reality in Japan (AIRJ). Arerugi 2002;51:411-20. [PubMed]
- Neffen H, Fritscher C, Cuevas F, et al. The Asthma insights and reality in Latin America survey. Rev Panam Salud Publica 2005;17:191-7. [Crossref] [PubMed]
- Sekerel BE, Gemicioglu B, Soriano JB. Asthma insights and reality in Turkey (AIRET) study. Respir Med 2006;100:1850-4. [Crossref] [PubMed]
- Turktas H, Mungan D, Uysal A, et al. Determinants of asthma control in tertiary level in Turkey: a cross-sectional multicenter survey. J Asthma 2010;47:557-62. [Crossref] [PubMed]
- Celik GE, Bavbek S, Paşaoğlu G, et al. Direct medical cost of asthma in Ankara, Turkey. Respiration 2004;71:587-93. [Crossref] [PubMed]
- Bavbek S, Mungan D, Türktaş H, et al. ADVISE Study Group. A cost-of-illness study estimating the direct cost per asthma exacerbation in Turkey. Respir Med 2011;105:541-8. [Crossref] [PubMed]
- Global Initiative for Asthma (GINA). Global strategy for asthma management and prevention (Update 2017). Avaliable online: https://cdn.mednet.co.il/2017/08/%D7%A0%D7%A1%D7%A4%D7%97-%D7%90-GINA-2017.pdf
- Yıldız F, Oğuzülgen IK, Dursun B, et al. TTS Asthma and Allergy Working Group Guideline Committee for Asthma Turkish Thoracic Society asthma management and prevention guideline: key points. Tuberk Toraks 2011;59:291-11. [Crossref] [PubMed]
- Uysal MA, Mungan D, Yorgancioglu A, et al. Study Group. Turkish Asthma Control Test (TACT), Turkey. Asthma control test via text messaging: could it be a tool for evaluating asthma control? J Asthma 2013;50:1083-9. [Crossref] [PubMed]
- Gemicioglu B, Borekci S, Can G. Investigation of knowledge of asthma and inhaler devices in pharmacy workers. J Asthma 2014;51:982-8. [Crossref] [PubMed]
- Yıldız F. ASIT Study Group. Factors influencing asthma control: results of a real-life prospective observational asthma inhaler treatment (ASIT) study. J Asthma Allergy 2013;6:93-101. [Crossref] [PubMed]
- Mısırlıgil Z, Çımrın A, Günen H, et al. Real life profile of asthma and chronic obstructive pulmonary disease patients in Turkey. Tuberk Toraks 2017;65:169-79. [Crossref] [PubMed]
- T.C. Sağlık Bakanlığı, Sağlık Hizmetleri Genel Müdürlüğü, Teşhis İlişkili Gruplar Veri Sistemi, 2011-2015, offline. Available online: http://dosyamerkez.saglik.gov.tr/Eklenti/3385,tig-sertifikali-egitim-programi-basvurularipdf.pdf
- Yıldız F, Bingöl Karakoç G, Ersu Hamutçu R, et al. The evaluation of asthma and COPD awareness in Turkey (GARD Turkey Project-National Control Program of Chronic Airway Diseases). Tuberk Toraks 2013;61:175-82. [Crossref] [PubMed]
- Ersu R, Bingöl Karakoç G, Yildiz F, et al. Evaluation of asthma and COPD awareness in primary care doctors in Turkey. Tuberk Toraks 2016;64:152-62. [Crossref] [PubMed]
- Türkiye’nin hava kirliliği ve İklim değişikliği sorunlarına sağlık açısından yaklaşım T.C. Sağlık Bakanlığı Temel Sağlık Hizmetleri Genel Müdürlüğü, Ankara, Anıl Matbaacılık 2010, 172p. Available online: http://www.ihsm.gov.tr/ihsmkronik/dosya/turkiyenin_havakirliligi_veiklimdegisikligi_sorunlari.pdf
- Ulubay G, Köktürk N, Görek Dilektaşlı A, et al. Turkish Thoracic Society national spirometry and laboratory standards. Tuberk Toraks 2017;65:117-30. [Crossref] [PubMed]
- Öner Erkekol F, Köktürk N, Mungan D, et al. Assessing the knowledge in primary health care following an educational course structured in the context of GARD chronic airway diseases national control program. Tuberk Toraks 2017;65:80-9. [Crossref] [PubMed]
- Ergün P, Çinal A, Yardım N, Yorgancıoğlu A. Göğüs Hastalıklarında Evde Sağlık Hizmeti Sunumu T.C. Sağlık Bakanlığı Temel Sağlık Hizmetleri Genel Müdürlüğü, Ankara, Anıl Matbaacılık, 2011, 106p. Available online: https://sbu.saglik.gov.tr/Ekutuphane/kitaplar/gogushasatliklarisunumugard.pdf
- Yorgancioglu A, Cruz AA, Bousquet J, et al. The Global Alliance against Respiratory Diseases (GARD) Country Report. Prim Care Respir J 2014;23:98-101. [Crossref] [PubMed]
- Bousquet J, Addis A, Adcock I, et al. Integrated care pathways for airway diseases (AIRWAYS-ICPs). Eur Respir J 2014;44:304-23. [Crossref] [PubMed]
- Bousquet J, Barbara C, Bateman E, et al. AIRWAYS-ICPs (European Innovation Partnership on Active and Healthy Ageing) from concept to implementation. Eur Respir J 2016;47:1028-33. [Crossref] [PubMed]
- Bousquet J, Agache I, Aliberti MR, et al. Transfer of innovation on allergic rhinitis and asthma multimorbidity in the elderly (MACVIA-ARIA) - Reference Site Twinning (EIP on AHA). Allergy 2018;73:77-92. [Crossref] [PubMed]


