How to recognize silent atrial fibrillation in pacemakers and defibrillators—the value of atrial electrograms
Clinical vignette and discussion
A 76-year-old patient with a dual-chamber pacemaker implanted in 2012 due to complete atrioventricular (AV)-block, attended to routinary pacemaker check-up. The device interrogation showed the presence of multiple atrial high rate episodes (AHRE) with variable duration, from few minutes to several hours, compatible with silent atrial fibrillation (AF). Intracardiac electrograms (EGMs) confirmed the diagnosis of AF (Figure 1). During the episodes the patient was on ventricular pacing at a normal heart rate and completely asymptomatic. On the other hand, the presence of AHRE compatible with silent AF is related with a higher risk of stroke (1). However, the application of anticoagulation therapy in patients with device-detected AHRE is yet unclear and challenging in the absence of randomized studies.
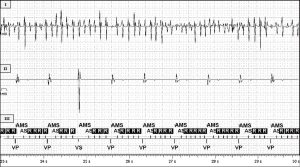
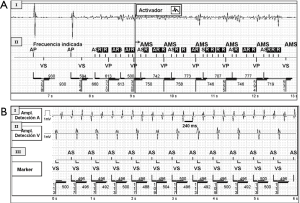
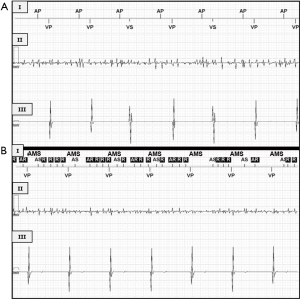
Diagnosis of silent paroxysmal AF represents a challenge, since the arrhythmia may be brief, completely asymptomatic and difficult to detect. Today’s cardiac implantable electronic devices (pacemakers and defibrillators) diagnostics include system diagnostics revealing battery status, energy consumption, lead impedance…but also algorithms for detecting and treating cardiac arrhythmias (2). The device detects the onset of AF episodes as AHRE when the atrial rate exceeds the programmed arrhythmia detection rate during a programmable number of beats. However, when interpreting counter data, we should evaluate for possible inappropriate device behavior or programming. Factors that limit the value of diagnostic counters include over-sensing, under-sensing, far-field sensing, cross-talk, interferences (noise), detection criteria not fulfilled by an arrhythmia, inappropriate programmed detection criteria… (3) (Figure 2). Under-sensing is not uncommon in AF, due to the small amplitude of atrial EGMs (Figure 3). The incorporation of stored EGMs has been an important milestone in improving the diagnostic capabilities of these devices. Multiple studies have clearly shown that data retrieved from diagnostic counters may be misleading (4). This does not imply that the devices are functioning inappropriately. It merely emphasizes the limitations of detection algorithms, which follow mathematical rules to classify events on a beat-to-beat basis. Stored EGMs are an essential tool to evaluate an appropriate or inappropriate detection documenting the intracavitary signals during the episodes and therefore to confirm the diagnosis of the arrhythmia detected by the device (5).
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Benezet-Mazuecos J, Rubio JM, Farré J. Atrial high rate episodes in patients with dual-chamber cardiac implantable electronic devices: unmasking silent atrial fibrillation. Pacing Clin Electrophysiol 2014;37:1080-6. [Crossref] [PubMed]
- Seidl K, Meisel E, VanAgt E, et al. Is the atrial high rate episode diagnostic feature reliable in detecting paroxysmal episodes of atrial tachyarrhythmias? Pacing Clin Electrophysiol 1998;21:694-700. [Crossref] [PubMed]
- Almehairi M, Baranchuk A, Johri A, et al. An unusual cause of automatic mode switching in the absence of an atrial tachyarrhythmia. Pacing Clin Electrophysiol 2014;37:777-80. [Crossref] [PubMed]
- Nowak B. Pacemaker stored electrograms: teaching us what is really going on in our patients. Pacing Clin Electrophysiol 2002;25:838-49. [Crossref] [PubMed]
- Pollak WM, Simmons JD, Interian A Jr, et al. Clinical utility of intraatrial pacemaker stored electrograms to diagnose atrial fibrillation and flutter. Pacing Clin Electrophysiol 2001;24:424-9. [Crossref] [PubMed]


