The curative effect of synthetic treatment for refractory acute myocardial infarction
Introduction
Acute myocardial infarction (AMI) is a condition that refers to myocardial ischemic necrosis caused by thrombus that completely blocks the coronary artery. The mortality rate of AMI with shock can reach as high as 50–80% (1). Therefore, this has become a major concern for patients with coronary heart disease.
For AMI patients complicated with shock, percutaneous coronary intervention (PCI) is presently the most direct and effective means of opening the obstructed coronary arteries, due to its advantages of small trauma, high blood flow rate and good short-term effect (2). Intra-aortic balloon counterpulsation (IABP) has a specific curative effect on critical heart disease. Its main technical principle is that it can increase the blood flow of the coronary artery, reduce the front and back load of the heart, decrease heart rate, increase urine volume and improve blood pressure, helping the failed heart to undergo circulation, weather the crisis, and thereby obviously increase the success rate of rescue for AMI patients (3). When emergency PCI fails or is not performed smoothly, it is often referred to as refractory AMI. For these patients, the following synthetic approaches were used: (I) PCI + IABP; (II) emergency off-pump coronary artery bypass (E-OPCAB), which is one of the most effective methods to rescue patients when PCI fails (4); (III) hybrid cardiac surgery, namely, minimally invasive direct coronary bypass grafting (MIDCAB) combined with PCI for the treatment of multivessel coronary artery disease (5). For AMI patients in whom the culprit vessel is the left anterior descending (LAD), when PCI failure and severe stenosis in the other branches of the coronary artery occurs, one-stop hybrid cardiac surgery should be carried out; that is, PCI would be carried out for other coronary branches with severe stenosis, while MIDCAB would be carried out for the anterior descending branch (6). Intraoperative coronary flow measurement brings a quantified indicator for the effect of bypass grafting (7). Intraoperative or postoperative IABP can improve the therapeutic effect. For AMI patients in whom the culprit vessel is not LAD, when severe stenosis occurs in the LAD after a successful emergency PCI, multi-stop hybrid cardiac surgery with minimally invasive bypass grafting can improve its long-term curative effects (8,9).
From a developmental perspective, the authors consider that hybrid cardiac surgery for AMI would likely to be one of the important treatments for AMI in the future.
Methods
General information
This study was approved by the Ethics Committee of the First People’s Hospital of Lanzhou (No.19960603). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images. The data of 76 patients with coronary AMI accompanied by shock, who were treated with combined therapy from August 1999 to April 2017, were included into this study. Among these patients, 62 patients were male and 14 patients were female. The youngest patient was 32 years old and the oldest patient was 74 years old. Sixty patients received emergency PCI. Among these 60 patients, 39 patients received IABP, eight patients underwent PCI, but failed and turned to E-OPCAB, and eight patients were treated by hybrid cardiac surgery. Among these eight patients, four patients received “one-stop” procedure, while the remaining four patients received “multi-stop” procedure. Transthoracic ultrasonography: a total of 46 patients were examined before surgery, and all patients were examined at the intensive care unit (ICU) and ward after surgery. Furthermore, all patients were successfully rescued. However, one patient failed in PCI and turned to E-OPCAB but died due to intractable low cardiac output syndrome at day 4, while another 74-year-old patient underwent percutaneous transluminal coronary revascularisation (PTCR) + IABP and died of acute renal failure at day 11.
Comprehensive measures
PCI + IABP: for patients suffering from severe shock, IABP was carried out for lifesaving before PCI, and was IABP continued after PCI until the circulation became stable. After PCI, IABP was immediately carried out when shock was not corrected.
Stent placement through the internal mammary artery (IMA) graft and the LAD branch of the coronary artery was carried out to rescue AMI patients after bypass grafting.
When PCI failed, E-OPCAB was immediately carried out, in which intraoperative coronary flow measurement led to a quantified indicator of the effect of E-OPCAB.
One-stop hybrid cardiac surgery: When the culprit vessel was LAD, PCI failed and other coronary branches were severely narrowed, PCI was carried out for other coronary branches with severe stenosis, and E-MIDCAB was carried out for the LAD branch.
Multi-stop hybrid cardiac surgery: For patients who had a successful PCI for the culprit vessel and had severe stenosis in the non-culprit vessels, MIDCAB was carried out after the disease was stabilized.
Results
All patients were successfully rescued. However, two patients died in the perioperative period. Among these two patients, one patient failed in PCI and turned to E-OPCAB but died of refractory low cardiac output syndrome on day 4, while the other 74-year-old patient was died of renal failure on day 11 after PCI + IABP.
Typical cases
Case 1
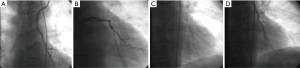
Xiao, male, 62 years old. This patient was diagnosed with AMI in the Emergency Department of Gaolan County Hospital and transferred to the Heart Research Institute at 2:00 p.m. on March 6, 2017. Emergency blood test and electrocardiogram examination were performed, and the patient was sent to the catheterization room for emergency PCI. Coronary angiography revealed the following: segments after LAD6 were 100% occluded, antegrade thrombolysis in myocardial infarction (TIMI) blood flow was grade 0, left circumflex (LCX) was 100% occluded, antegrade TIMI blood flow was grade 0, the right coronary artery (RCA)2 segment narrowed by 60%, the endometrium was unsmooth, and antegrade TIMI blood flow was grade 2 (Figure 1A).

The patient was scheduled to undergo PCI in the LAD and LCX. A guidewire was inserted and passed through the LAD, the narrowed segment in LAD6 was repeatedly dilated with a 1.5 mm × 1.5 mm balloon, but it failed, and 500,000 units of urokinase was injected. After 10 minutes, angiography revealed a small blood flow at the distal end of the LAD and LCX (Figure 1B). PCI was planned to continue to place the stent. However, heart rate increased (170 bpm) and blood pressure decreased (60/40 mmHg). Hence, the patient was transferred to Intensive Medicine for rescue.
After the patient was transferred to Intensive Medicine, IABP was carried out at 18:30 and 1:1 counterpulsation was initiated, which was assisted by the micro pumping of renal and suprarenal hormones, dopamine and nitroglycerin. Due to ecphysesis (35/min) and decreased oxygen saturation (80%), respiration was controlled using are spirator at 19:40. After 9 days, the respirator was removed (March 15), and the IABP was removed 11 days later. After removal, coronary angiography revealed the following: the distal blood flow of the LAD and LCX significantly improved (Figure 1C). On March 24, OPCAB was carried out. At 11 days after the surgery, the patient recovered and was discharged from the hospital.
Case 2
Wei, male, 69 years old. This patient was admitted in the hospital at December 3, 2014 due to AMI with shock. This patient underwent coronary artery bypass grafting 3 years ago. PCI was carried out immediately after admission. Left internal mammary angiography revealed 90% stenosis at the distal anastomotic end of the LAD branch, and 85% stenosis at the LCX branch (Figure 2A,B). One stent was implanted in the circumflex branch, while one stent was implanted through the LAD branch of the left IMA (Figure 2C,D). After the operation, IABP was placed, and the patient’s condition of shock gradually improved. The patient recovered and was discharged at day 7.
Case 3
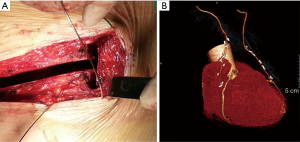
Hou, male, 59 years old. This patient was admitted in the hospital at December 14, 2014 due to AMI with shock. Emergency PCI: 90% stenosis of the LAD, 90% stenosis of the RCA and 85% stenosis of the LCX were observed. Blood pressure decreased and heart rate increased when stents were planned to be placed during balloon dilatation at the LCX, 500,000 U of urokinase was rapidly injected at the LAD, and PCI was ended. Then, the patient was transferred to Intensive Medicine for rescue. The patient gradually recovered. After 2 weeks, the patient underwent MIDCAB at the bilateral internal mammary arteries, in which small incisions were performed under the sternum (Figure 3A,B).
Discussion
IABP has a special curative effect on critical heart disease, and the reasonable use of IABP can significantly improve the rescue success rate of AMI patients (10). For patients with AMI accompanied by shock, who require emergency PCI, the timing of IABP (before or after PCI) should depend on the condition of the patient. If the condition of the patient is relatively stable, PCI can be initially carried out. If shock progressively exacerbates, IABP can be initially placed combined with a micro pump. Then, PCI would be carried out when a relatively stable condition is achieved. If the circulation is unstable during PCI and the stent is difficult to implant, too much time should not be spent in placing the stent, PCI should be ended in time and turned to IABP, and the patient should be transferred to the ICU. After the condition of the patient becomes stable, OPCAB or PCI should be carried out.
Coronary angiography should be carried out in time when patients present with AMI after E-OPCAB, in order to determine the site of the culprit vessel. If infarct or stenosis occurs at the distal end of the anastomosis, PCI can be performed through the IMA graft to get through to the culprit vessel (11).
At present, emergency PCI remains as the most direct and effective means of opening infarcted coronary vessels. However, when emergency PCI fails, the mortality rate of AMI considerably increases. E-OPCAB is one of the most effective methods to rescue patients when the above methods fail, which can improve the success rate of rescue for AMI.
Hybrid cardiac surgery is the combination of MIDCAB and PCI in the treatment of multivessel coronary artery disease (12). Its advantage is that it has the benefits of IMA-anterior descending branch bypass grafting (one part of the coronary artery bypass surgery) and takes the advantage of the feature of small trauma of PCI in the treatment of lesions in other coronary arteries, making the greatest clinical benefit for patients (13). In the present study, the hybrid cardiac surgery approach was used to treat multivessel coronary artery disease and rescue AMI patients, improving the success rate. Hybrid cardiac surgery in the treatment of coronary AMI has advantages of small trauma, fast recovery, and a satisfactory medium- and long-term curative effect, making this suitable for coronary AMI patients in whom the culprit vessel was the anterior descending branch and PCI has failed, patients with severe stenosis in the anterior descending branch in whom the culprit vessel was not the anterior descending branch and PCI has succeeded, and patients with multivessel disease who failed to achieve a satisfactory outcome through surgery alone or catheter intervention alone.
“One-stop” hybrid cardiac surgery in the treatment of AMI: for the patients in whom the culprit vessel is the LAD, PCI has failed and the other coronary branches have severe stenosis, PCI was carried out for other coronary branches with severe stenosis and E-MIDCAB was carried out for the anterior descending branch (14,15).
Left internal mammary artery (LIMA) and anterior descending branch bypass grafting have been considered as the gold standard for coronary revascularization (16). Interventional catheter and vein transplantation cannot achieve the same treatment effect (17). Hybrid surgery simultaneously combines the advantages of interventional and surgical treatment, providing a new pathway for the treatment of patients with multivessel disease (18). Hybrid surgery in the treatment of AMI, especially when the culprit vessel is the LAD and PCI has failed. The use of one-stop hybrid cardiac surgery of PCI and MIDCAB in the same period leads to effective myocardial reperfusion in the infarcted region and reduces the mortality rate of AMI patients. This technique simultaneously deals with the pathological changes of the culprit vessel and stenotic vessels and has a good long-term effect.
“Multi-stop” hybrid cardiac surgery in the treatment of AMI: for AMI patients in whom the culprit vessel is not the LAD, the LAD with severe stenosis undergoes MIDCAB step by step after successful emergency PCI, or if the culprit vessel is LAD, emergency MIDCAB is carried out after PCI fails, and PCI is carried out for the other diseased branches. The “multi-stop” hybrid cardiac surgery reflects the principles in rescuing AMI patients, that is, “emergency first, followed by radical cure”. PCI is performed for the culprit vessel first, and other severe vessels with stenosis are treated when the condition becomes stable. This method is safe and reliable (19).
In “multi-stop” hybrid cardiac surgery, when the condition permits, bilateral IMA OPCAB can be adopted by performing a small incision under the sternum, allowing the left and right coronary arteries to completely become arteries through small incisions, and achieving a satisfactory long-term curative effect (20).
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This study was approved by the Ethics Committee of the First People’s Hospital of Lanzhou (No. 19960603). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Jung C, Lauten A, Ferrari M. Microcirculation in cardiogenic shock: from scientific bystander to therapy target. Crit Care 2010;14:193-9. [Crossref] [PubMed]
- Tsagalou EP, Anastasiou-Nana MI, Nanas JN. Intra-aortic balloon counterpulsation for the treatment of myocardial infarction complicated by acute severe heart failure. Congest Heart Fail 2009;15:35-40. [Crossref] [PubMed]
- Wei L, Xiang M, Lins M. Evaluation of application of Intra-aortic balloon counterpulsation in patients with cardiogenic shock complicated with acute myocardial infarction. Chin J Emerg Med 2002;11:389-91.
- Hirose H, Amano A, Yoshida S, et al. Surgical management of unstable patients in the evolving phase of acute myocardial infraction. Ann Thorac Surg 2000;69:425-8. [Crossref] [PubMed]
- Halkos ME, Vassiliades TA, Douglas JS, et al. Hybrid coronary revascularization versus off-pump coronary artery bypass grafting for the treatment of multivessel coronary artery disease. Ann Thorac Surg 2011;92:1695-701. [Crossref] [PubMed]
- Ortiz M, Brinkhaus B, Enck P, et al. Autonomic Function in Seasonal Allergic Rhinitis and Acupuncture - an Experimental Pilot Study within a Randomized Trial. Forsch Komplementmed 2015;22:85-92. [PubMed]
- D'Ancona G, Karamanoukian HL, Ricci M, et al. Graft patency verification in coronary artery bypass grafting: principles and clinical applications of transit time flow measurement. Angiology 2000;51:725-31. [Crossref] [PubMed]
- Xie J, Wang Y, Li J, et al. Hybrid cardiac surgery in treatment of acute myocardial infarction: a report of 6 cases. Chin J Emerg Med 2016;25:227-9.
- Gosev I, Leacche M. Hybrid Coronary Revascularization: The future of coronary artery bypass surgery or an unfulfilled promise? Circulation 2014;130:869-71. [Crossref] [PubMed]
- Thiele H, Sick P, Boudriot E, et al. Randomized comparison of intra-aortic balloon support with a percutaneous left ventricular assist device in patients with revascularized acute myocardial infarction complicated by cardiogenic shock. Eur Heart J 2005;26:1276-83. [Crossref] [PubMed]
- Kou Z, Wang Y, Gan Y, et al. Placement of stents in coronary artery from left arteriae mammaria interna in left anterior descending for cure coronary atherosclerotic heart disease: a case report. Chin J Clin Thorac Cardiovasc Surg 2017;(2):85-6.
- Byrne JG, Leacche M, Vaughan DE, et al. Hybrid cardiovascular procedures. JACC Cardiovasc Interv 2008;1:459-68. [Crossref] [PubMed]
- Holzhey DM, Jacobs S, Mochalski M, et al. Minimally invasive hybrid coronary artery revascularization. Ann Thorac Surg 2008;86:1856-60. [Crossref] [PubMed]
- Wu H, Sun H, Jiang X, et al. Simultaneous hybrid revascularization by peripheral artery stenting and off-pump coronary artery bypass: the early results. Ann Thorac Surg 2011;91:661-4. [Crossref] [PubMed]
- Shen L, Hu S, Wang H, et al. One-stop hybrid coronary revascularization versus coronary artery bypass graft and percutaneous coronary intervention for the treatment of multivessel coronary artery disease: three-year follow-up results from a single institution. J Am Coll Cardiol 2013;61:2525-33. [Crossref] [PubMed]
- Mariani MA, Boonstra PW, Grandjean JG, et al. Minimally invasive coronary artery bypass grafting versus coronary angioplasty for isolated type C stenosis of the left anterior descending artery. J Thorac Cardiovasc Surg 1997;114:434-9. [Crossref] [PubMed]
- Lloyd CT, Calafiore AM, Wilde P, et al. Integrated left anterior small thoracotomy and angioplasty for coronary artery revascularization. Ann Thorac Surg 1999;68:908-11. [Crossref] [PubMed]
- Harskamp RE, Puskas JD, Tijssen JG, et al. Comparison of hybrid coronary revascularization versus coronary artery bypass grafting in patients ≥65 years with multivessel coronary artery disease. Am J Cardiol 2014;114:224-9. [Crossref] [PubMed]
- Kim KB, Cho KR, Jeong DS. Midterm angiographic follow-up after off-pump coronary artery bypass: serial comparison using early, 1 year, and 5-year postoperative angiograms. J Thorac Cardiovasc Surg 2008;135:300-7. [Crossref] [PubMed]
- Gan Y, Zhao Q, Wang Y, et al. Minimally invasive coronary artery bypass grafting on bilateral internal mammary artery with limited lower sternotomy: a case report. Chin J Thorac Cardiovasc Surg 2015;31:700-1.


