Right upper sleeve lobectomy by video-assisted thoracic surgery
Introduction
Sleeve lobectomy (SL) can preserve more pulmonary parenchyma and offer equal oncologic efficiency with pneumonectomy, which has been regarded as a preferred approach for selected central non-small cell lung cancer (NSCLC) (1,2). With noticeable advances in both VATS experiences and devices in past decade, some doctors have performed this technique in more challenging procedures such as bronchial SL and double-SL (3,4).
Nevertheless, VATS SL remains a challenging procedure and is mastered only by sophisticated surgeons. This is a result of two-dimensional vision of thoracoscopy and endoscopic bronchial anastomosis is difficult. Here, we demonstrated a case of complete VATS right upper SL and systematic lymph node dissection (Figure 1).

Clinical data
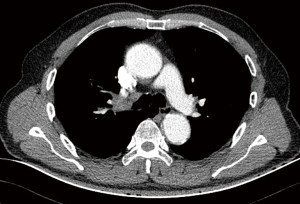
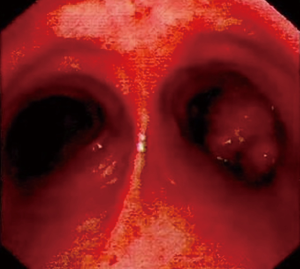
A 62-year-old male patient was admitted to our department for irritable coughing for one month. He had a smoking history for 20 years, 20 packs per day. A 3.5 cm × 2 cm mass was detected in the right upper lobe with obstructing right upper bronchus on chest CT (Figure 2). Bronchoscopy displayed the tumor protruding from the opening of the right upper lobe bronchus and obstructing the bronchus completely (Figure 3). Pathologic examination was proved to be squamous cell carcinoma.
Operative techniques
The operation was undertaken under general anesthesia with one-lung ventilation. The patient was placed with left lateral decubitus position. The traditional three incisions technique was performed. The camera port (1.5-cm long incision) was located on the 7th intercostal space in the midaxillary line. The primary process port (4-cm long incision) and the assistant process port (1.5-cm long incision) were chosen at the level of 4th intercostal space in anterior axillary line and the 7th intercostal space in the post-axillary line respectively.
First, dissociation of the lower lung ligament and dissection of the mediastinal lymph nodes of level 9, 7 were performed by ultrasonic scalpel (ETHICON Harmonic). Mediastinal pleura of superior and anterior hilum were divided and lymph nodes of hilum (level 10) were dissected. Second, the right upper lobe vein and apico-anterior truncus were mobilized and transected with a vascular endostapler (Endo-GIA, Medtronic, USA) respectively. Third, oblique and horizontal fissures were separated by linear endostapler respectively following dissection of the station 11 lymph nodes. The two posterior ascending branches were then fully freed and cut by a vascular endostapler. Fourth, azygos vein was transected with a vascular stapler for better exposure. Then lymph nodes of level 4R, 2R were cleared. The right main bronchus and bronchus intermedius were adequately divided. The intermediate bronchus and right main bronchus were cut circumferentially by a knife and scissors. The specimen was removed with a protective bag, and two margins of bronchial stumps were confirmed tumor-free by frozen historical examination. Fifth, end-end anastomosis was initiated from the junction of cartilage-membrane. Continuous suture was performed from posterior wall to anterior wall with 3-0 prolene. Following tightening the prolene suture, the knot was tied outside of anastomosis. Bronchial anastomosis was checked without air leak under water. A 26-F chest tube was placed through camera incision.
Pathologic examination revealed stage IB squamous carcinoma (T2aN0M0). X-ray revealed fully expanded of middle and lower lobes. Chest drainage was removed on the fourth day after operation and the patient was discharged on postoperative eighth day.
Comments
We suggest dissecting mediastinal and hilar lymph nodes firstly, which facilitates exposure of posterior wall of intermediate bronchus and separating the oblique fissure. Bronchial anastomosis is the crucial step and remains challenging procedure. The key points of this procedure conclude systemic dissection of mediastinal (station 2, 4R, 7) and station 11 lymph nodes, transection of azygos vein and fully dissociation of the secondary carina and main bronchus (6). Continuous suture is commended to anastomosis, because it is helpful for uniform tensions and reducing operative duration (3). The “difficult-to-easy” and “from far to near” principle should be adopted and sutures should be performed from posterior wall to anterior wall (7). Meanwhile, tangling of sutures is a common pitfall in SL and should be prevented by proper suturing order (8).
Acknowledgements
This video was granted the Award of Great Potential in the 2017 Master of Thoracic Surgery—Video-assisted Thoracoscopic Surgery Video Contest.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Ma Z, Dong A, Fan J, et al. Does sleeve lobectomy concomitant with or without pulmonary artery reconstruction (double sleeve) have favorable results for non-small cell lung cancer compared with pneumonectomy? A meta-analysis. Eur J Cardiothorac Surg 2007;32:20-8. [Crossref] [PubMed]
- Cusumano G, Marra A, Lococo F, et al. Is sleeve lobectomy comparable in terms of short- and long-term results with pneumonectomy after induction therapy? A multicenter analysis. Ann Thorac Surg 2014;98:975-83. [Crossref] [PubMed]
- Huang J, Li S, Hao Z, et al. Complete video-assisted thoracoscopic surgery (VATS) bronchial sleeve lobectomy. J Thorac Dis 2016;8:553-74. [Crossref] [PubMed]
- Lyscov A, Obukhova T, Ryabova V, et al. Double-sleeve and carinal resections using the uniportal VATS technique: a single centre experience. J Thorac Dis 2016;8:S235-41. [PubMed]
- Guo J, Liu Y, Liang C. Video-assisted thoracoscopic right upper lobe sleeve lobectomy. Asvide 2018;5:646. Available online: http://www.asvide.com/article/view/26155
- Fan JQ, Yao J, Chang ZB, et al. Left lower sleeve lobectomy and systematic lymph node dissection by complete video-assisted thoracic surgery. J Thorac Dis 2014;6:1826-30. [PubMed]
- Ma Q, Liu D. VATS right upper lobe bronchial sleeve resection. J Thorac Dis 2016;8:2269-71. [Crossref] [PubMed]
- Chen H, Huang L, Xu G, et al. Modified bronchial anastomosis in video-assisted thoracoscopic sleeve lobectomy: a report of 32 cases. J Thorac Dis 2016;8:2233-40. [Crossref] [PubMed]


