Successful phased approach to a patient with synchronous traumatic descending aortic pseudoaneurysm and bronchial rupture
Introduction
Both traumatic aortic pseudoaneurysm and bronchial rupture are rare but highly lethal injuries. Most of the victims may die before arriving the hospital. Patients who survive from combined aortic and bronchial rupture are even more rare. As far as we know, there have been only two cases with traumatic rupture of the aorta and bronchus in the English literature (1,2). Both cases had ascending aortic and left main bronchial rupture which were treated with simultaneous open surgery. Herein, we report the first case of combined descending aortic pseudoaneurysm and left main bronchial rupture from blunt chest trauma (BCT) which was successfully treated with a phased approach.
Case presentation
A 34-year-old female pedestrian was hit by a car on her back. She suffered from chest pain and dyspnea after injury. The patient was sent to a local hospital after the accident. Preliminary chest computed tomography (CT) scan revealed left hemopneumothorax, left multiple rib fractures, scapula and bilateral clavicle fractures. An emergent left exploratory thoracotomy was performed, followed by surgical fixation of the fractured clavicles. Pulmonary laceration and a little mediastinal hemorrhage were found during surgery. The lung was repaired by suturing while the mediastinum remained untouched. The ventilation of left lung was normal before closing the chest. However, she had progressive left pulmonary atelectasis after surgery. Bronchoscope was performed 6 days later and revealed bronchial stenosis.
The patient was referred to our center one week after the accident. Further bronchoscopic assessment confirmed bronchial injury (Figure 1A). Chest CT showed collapsed left lung and normal-shaped aorta (Figure 1B). However, suspicious aortic injury was found on contrast CT scan (Figure 1B). The diagnosis of aortic pseudoaneurysm was confirmed by CT angiography (CTA) (Figure 1C,D). The rupture was located at the proximal descending aorta near the aortic isthmus.

After the multidisciplinary discussion, we decided to adopt a phased approach for this patient. Aortic endovascular repair was performed first. The stent (Medtronic EVR Valiant TF 3030C150X) was placed through the right external iliac artery for severe contusions of the femoral artery. She stayed in the intensive care unit (ICU) for 7 days after the intervention. Another 4 days later, bronchial reconstruction was performed through left posterolateral thoracotomy. Dense adhesion and scar tissue developed surrounding the injured bronchus which was carefully dissected. The stricture was about 2-cm in length and was resected. Bronchial anastomosis was done with continuous suture using 3-0 Prolene stiches. The operation was finished in 150 min with 100 mL of blood loss. She stayed in the ICU for another 2 days after the operation.
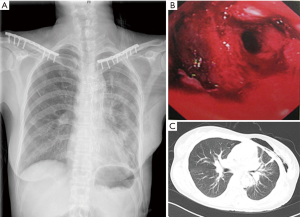
Repeated bronchoscopy was performed on the first 3 days after surgery to clear airway secretions. The chest tube was removed on postoperative day (POD) 7 when chest film confirmed fully re-expansion of left lung (Figure 2A). The patient recovered uneventfully and was discharged home on POD 14. Bronchoscopy and chest CT scan confirmed that the bronchial anastomosis worked well before discharging (Figure 2B,C). She is in good condition five years after the accident.
Discussion
The present case is the first report of combined traumatic descending aortic and bronchial rupture. However, both injuries were overlooked in this case at initial assessment because of atypical clinical manifestations. Early diagnoses of the injuries are critical to save lives.
Approximately 1% of the victims in vehicular accidents may have acute aortic injury while 80% of them may die before arriving the hospital (3,4). Aortic injury is the second leading cause of all trauma-related deaths and accounts for 16% of the deaths (3,4). Many survivors may not have any symptoms or sometimes, the signs may be covered by combined injuries. Contrast chest CT is the most preferred and effective diagnostic test for these patients (3). A previous study showed that the diagnosis of aortic injury was missed in 28% of the patients assessed by chest X-ray when compared with contrast CT scan (5). In our case, a regular chest CT without contrast was performed at initial assessment. However, the aortic injury was overlooked for the relatively normal-shaped aorta on CT scan.
Tracheobronchial rupture was also missed even during surgical exploration. This is another rare but severe injury with less than 2% of incidence following BCT (4). Most of the ruptures may happen within 2 cm to the carina and are difficult to be diagnosed. The injury can be divided into two distinct patterns, including complete and incomplete rupture. The symptoms of tracheobronchial rupture depend on the severity and site of injury which may vary from subcutaneous emphysema, pneumothorax and massive air leak in the chest tube. Complete bronchial rupture is usually life-threatening with unstable breathing and circulation which always require emergency surgery. However, incomplete rupture may initially have no symptoms which may lead to delayed diagnosis. Because of the nonspecific symptoms in patients with incomplete rupture, the diagnosis could be missed in approximately 5–80% of the victims during the first 24–48 hours after injury (6). In some cases, patients with injured airway may have almost normal breathing. For this reason, the diagnosis may by missed for a long period (7). The present case had pulmonary laceration but normal ventilation of the left lung during surgical exploration. Bronchial rupture was overlooked for this reason. However, mediastinal hemorrhage was found. This could be a potential sign of injury to the vital structures in the mediastinum, and required further diagnostic tests including chest contrast CT scan and bronchoscope.
Simultaneous surgical repair of both injuries was adopted decades ago with satisfactory results (1,2). With the improvements in endovascular grafting, thoracic endovascular aortic repair is becoming the more preferred choice for acute aortic injuries if no contraindications (8). Endovascular repair avoids cross clamping the aorta, the use of cardiopulmonary bypass, and is more mini-invasive to the patients, especially for those multi-trauma patients who may not tolerate open surgery. In this case, we adopted a phased intervention strategy. Aortic pseudoaneurysm was repaired with endograft first because the injury was more dangerous. However, the present patient was intolerable to open surgery immediately after the endovascular repair. Delayed reconstruction of the bronchus was set up for this patient because she had stable ventilation with collapsed left lung. The collapsed lung could re-expand as long as 17 years after the trauma (7). In this case, the left lung worked well after bronchial reconstruction performed 20 days after injury.
In conclusion, special attention should be paid to rule out acute aortic and tracheobronchial rupture in patients with severe BCT. As for combined descending aortic and tracheobronchial rupture, phased intervention with endovascular repair of the aorta followed by surgical repair of the bronchus is acceptable.
Acknowledgements
Funding: The work was supported by the grant (16PJ292) to Dr. Mei from the Health and Family Planning Commission of Sichuan Province, China.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any related images.
References
- Sadow SH, Murray CA 3rd, Wilson RF, et al. Traumatic rupture of ascending aorta and left main bronchus. Ann Thorac Surg 1988;45:682-3. [Crossref] [PubMed]
- Marzelle J, Nottin R, Dartevelle P, et al. Combined ascending aorta rupture and left main bronchus disruption from blunt chest trauma. Ann Thorac Surg 1989;47:769-71. [Crossref] [PubMed]
- Neschis DG, Scalea TM, Flinn WR, et al. Blunt aortic injury. N Engl J Med 2008;359:1708-16. [Crossref] [PubMed]
- Karmy-Jones R, Wood DE. Traumatic injury to the trachea and bronchus. Thorac Surg Clin 2007;17:35-46. [Crossref] [PubMed]
- Exadaktylos AK, Duwe J, Eckstein F, et al. The role of contrast-enhanced spiral CT imaging versus chest X-rays in surgical therapeutic concepts and thoracic aortic injury: a 29-year Swiss retrospective analysis of aortic surgery. Cardiovasc J S Afr 2005;16:162-5. [PubMed]
- Prokakis C, Koletsis EN, Dedeilias P, et al. Airway trauma: a review on epidemiology, mechanisms of injury, diagnosis and treatment. J Cardiothorac Surg 2014;9:117. [Crossref] [PubMed]
- Toker A, Tanju S, Dilege S. Reimplantation of the left lung 17 years after a bronchial rupture. Ann Thorac Surg 2008;85:1436-8. [Crossref] [PubMed]
- Patelis N, Katsargyris A, Klonaris C. Endovascular Repair of Traumatic Isthmic Ruptures: Special Concerns. Front Surg 2017;4:32. [Crossref] [PubMed]


