Quantification of pleural plaques by computed tomography and correlations with pulmonary function: preliminary study
Introduction
Exposure to asbestos represents an important health hazard and this issue remains a topic of public interest because of the ubiquity of asbestos in daily life, and its association with pulmonary fibrosis and malignant diseases. Asbestos-related diseases include benign asbestos-related pleural effusion, pleural plaques, diffuse pleural thickening, asbestosis, bronchogenic carcinoma, and malignant pleural mesothelioma (1). In South Korea, computed tomography (CT) scans are used to assess asbestos-related diseases as required by the Asbestos Damage Relief Law and Compensation Act (2).
Pleural plaques are the most common manifestation of asbestos exposure and serve as a marker of asbestos exposure (1,3). These plaques are focal smooth areas of pleural thickening that predominantly involves parietal pleura of the lateral or posterolateral wall and the dome of the diaphragm (1). And occupationally exposed workers have more pleural plaque than environmentally exposed individuals (4). CT is the most accurate imaging method for the detection and characterization of pleural plaques (1,5). However, the quantification of pleural plaque by CT has not been well established.
Relationship between pleural plaque and pulmonary function impairment remains controversial. Several studies have reported pleural plaque has no significant effect on pulmonary function (3,6-8), although others have shown diminished pulmonary function in subjects with pleural plaques (9-13). However, chest radiography has low sensitivity and specificity for detecting pleural plaques, and might include diffuse pleural thickening and/or pulmonary abnormalities. Therefore, in this study, patients with pleural plaque detected on CT without other pulmonary parenchymal abnormalities, diffuse pleural thickening, or other abnormalities that might affect pulmonary function were included.
The aims of this study were to quantify pleural plaque volume (PPV) by CT and investigate relations between PPV and pulmonary function after excluding factors that might affect pulmonary function.
Methods
Study population
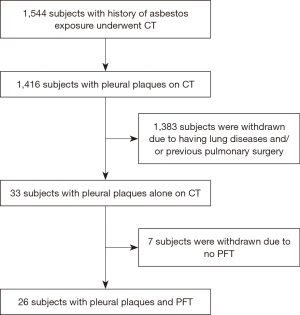
This retrospective study was approved by our Institutional review board (approval #2015-141). A total of 1,544 individuals that registered with the Korea Environment Corporation for asbestos damage relief from January 2011 to December 2015 were included. All had a history of environmental and/or occupational asbestos exposure and had undergone chest CT. Of these 1,544, 1,416 were diagnosed to have pleural plaque on CT. In addition, 1,383 with CT evidence of lung diseases and/or previous surgery; emphysema, bronchiectasis, pulmonary neoplasm, asbestosis, interstitial lung disease, pneumonia, atelectasis, round atelectasis, pulmonary edema, pneumothorax, pleural effusion, previous infectious sequelae, diffuse pleural thickening, previous pulmonary resection and pleurodesis, were excluded. In matters of emphysema, we only included trace centrilobular emphysema by CT-definable subtypes of chronic obstructive pulmonary disease, which is minimal centrilobular lucencies, occupying <0.5 percent of lung zone (14). Of the remaining 33 with pleural plaques alone on CT, 7 were excluded due to the absence of pulmonary function test (PFT). As a result, 26 subjects with pleural plaque and PFT results were included (Figure 1). Of 26 subjects, all subjects were environmentally exposed to asbestos and 18 had history of occupational asbestos exposure.
PFT
The PFT flow-volume curve parameters subjected to analysis were; forced vital capacity (FVC), forced expiratory volume in 1 second (FEV1), and FEV1/FVC ratio. Diffusing capacity of the lung for carbon monoxide (DLCO) results were also included. All subjects underwent PFT within 3 weeks from obtaining CT examination and no subject had an acute medical condition at time of PFT.
CT examination
CT scans were performed using various CT scanners at the institutions. All the CT scans were obtained using a CT protocol designed to evaluate pulmonary and pleural abnormalities related to asbestos exposure. It consisted of supine and prone thin section (1–1.5 mm) images obtained at 1 cm intervals and continuous supine thick section (3–5 mm) images.
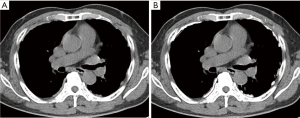
Manual volumetric measurement of pleural plaques using computer software
Data generated from CT scans were directly transferred to Syngo Volume (Syngo Multi-Modality Workplace, VE40, Siemens Healthineers, Forchheim, Germany) and reviewed by two radiologists by consensus (YK Cha, JS Kim). They were blinded to all clinical data when tracing the outlines of pleural plaques. PPVs were determined by tracing the total outline of pleural plaques on parietal, diaphragmatic, mediastinal, and fissural pleura on mediastinal window setting CT images at supine position by user defined subjective outlines. Mediastinal window setting was window level of 35 Hounsfield units (HU) and window width of 350 HU. All pleural plaques were traced from lung apex to hemidiaphragm and total PPVs were calculated by summation (Figure 2).
Statistical analysis
The Student’s t-test was used to compare the PFT for subjects with or without diaphragmatic, mediastinal, or diaphragmatic plus mediastinal pleural plaque. Simple linear regression analysis and multiple regression analysis were used to evaluate correlations between PPVs and PFT variables. Subjects were divided into three PPV groups, that is, <10, 10–20, and ≥20 mL, and analysis of variance was used to evaluate relations between PPVs and PFT results. Statistical significance was accepted for P values <0.05.
Results
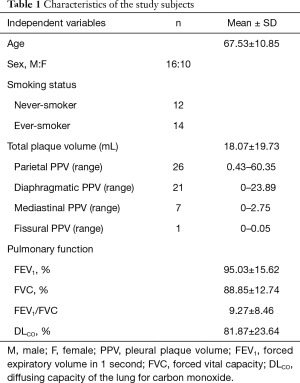
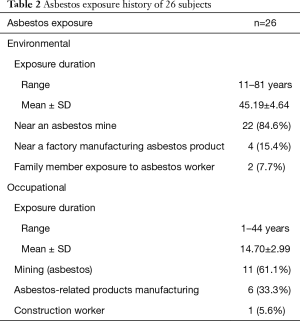
Of the 1,544 subjects that underwent CT scans between January 2011 to December 2015, 26 met the inclusion criteria. Baseline subject characteristics are presented in Table 1. Mean age was 67.5 years (range, 47 to 85 years) and the male/female ratio was 16:10. Fourteen patients (54%) were current- or ex-smokers and 12 patients (46%) were never-smokers. Ever-smokers had an average smoking history of 16.3 pack-years (range, 4 to 60 pack-years). Five patients had trace centrilobular emphysema in both lungs. Parietal PPV ranged from 0.43 to 60.35 mL; diaphragmatic PPV from 0 to 23.89 mL; mediastinal PPV from 0 to 2.75 mL, and fissural PPV from 0 to 0.05 mL. Total PPV ranged from 0.64 to 73.48 mL (mean ± SD, 18.07±19.73). Pulmonary function indices are presented in Table 1. All subjects had high level of asbestos exposure. Of 26 subjects, all subjects were environmentally exposed to asbestos, because they lived close to asbestos mines and asbestos handling or manufacturing plant within 2 km, and 18 had history of occupational asbestos exposure (Table 2). Asbestos exposure duration and PFT were not statistically significant.
Full table
Full table
No significant difference in PFT results was observed between subjects with or without diaphragmatic, mediastinal, or diaphragmatic plus mediastinal pleural plaque.
In simple linear regression analysis, there were no significant relationship between total PPV and PFT results. In addition, there were no significant differences according to smoking status, age and sex (Table 3).
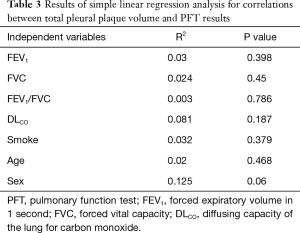
Full table
Similarly, multiple regression analysis showed no significant relationship between total PPV and PFT results. However, men had a significantly greater mean PPV than women (P=0.03) (Table 4).
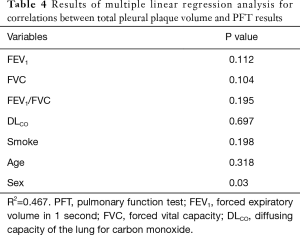
Full table
Analysis of variance was used to evaluate differences in PFT results between the <10, 10–20, and ≥20 mL PPV groups. No significant intergroup differences were found, but FEV1, FVC, and DLCO values in the ≥20 mL PPV group were lower than in the other two groups (Table 5), indicating a restrictive pattern of pulmonary function.
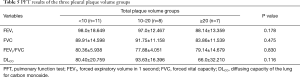
Full table
Discussion
To explore correlations between PPVs and pulmonary functional impairment, a reliable means of quantifying pleural plaques is essential. Various quantification methods for chest radiographs have been developed, but the most widely used method is from the International Labor Office (15). Some chest radiograph based studies (9-13) have reported the presence of pleural plaque is associated with decreased pulmonary function, but several studies based on CT (3,6-8) have reported no significant correlation. Differences in the results may be due to low sensitivity and specificity of chest radiograph for assessing pleural plaque and studies based on chest radiograph had a problem with inclusion of diffuse pleural thickening and other pulmonary abnormalities (9,10,12,13).
CT provides a better means of detecting and quantifying pleural plaque than chest radiography (6,16-18), but few have investigated the possible association between the presence of pleural plaque and pulmonary function (6-8,19,20), and fewer have attempted to quantify pleural plaques. Schwartz et al. (19) quantified asbestos-related pleural fibrosis volume on CT images by using their dedicated computer program by tracing pleural lesions and calculating the volumes and surface areas of pleural lesions. Van Cleemput et al. (6) quantified pleural plaque on CT images by using a computer mouse and measuring lengths, but calculated pleural plaque surface areas but not the volume of plaque. Copley et al. (7) assessed extents of pleural thickening and pleural plaques using a radiographic score based on the International Labor Office, a subjective simple CT score, a subjective comprehensive CT score, an objective nonautomated method, and an objective computer-aided semiautomatic method. They concluded that the subjective CT method had advantages in terms of ease of application and the accurate assessment of pleural lesions. This study also included diffuse pleural thickening. Meirelles et al. (18) proposed a CT visual semiquantitative measurement method for assessing pleural plaques, and quantified pleural plaque burden using a scoring system based on the percentage of parietal pleural surface involved and the maximum thickness of parietal pleural plaques. Intraobserver and interobserver agreements ranged from good to excellent for pleural plaque measurements. However, they did not measure mediastinal and fissural pleural plaques. In our study, PPVs were quantified using an objective CT method by tracing all visualized pleural plaque. We believe that this is the first attempt to quantify all PPV by CT without diffuse pleural thickening.
Recently, magnetic resonance (MR) images is reaching an important role in diagnosis of malignant pleural mesothelioma differentiating between benign pleural diseases, by diffusion-weighted imaging (DWI). In study by Revelli et al. (21), they found out that there was statistically significant difference between non-neoplastic pleural diseases, epithelioid and sarcomatoid subtypes of malignant pleural mesothelioma regarding to apparent diffusion coefficient (ADC) values. Coolen et al. (22) also found that pleural pointillism, which is the presence of multiple, hyperintense pleural spots in high-b-value DWI is useful to differentiate malignant pleural mesothelioma from benign pleural diseases.
In our study, no significant relationship was found between total PPV and pulmonary function nor between group of PPV, but higher PPV group tended to be associated with a restrictive pattern. We believe that our study is the first to subdivide PPV and examine relations between PPV and pulmonary function among these groups. But these PFT results are still within normal limits, it may not have a real clinical relevance for the subjects with decreased pulmonary function. Similarly, study by Clin et al. (20) showed that patients with isolated pleural plaques and/or diaphragmatic pleural plaques exhibited significant decreases in total lung capacity, FVC and FEV1 which showed a trend towards a restrictive pattern. However, they concluded that since PFT results were within normal limits, the PFT decreases were unlikely to be of clinical relevance. Clark et al. (8) also failed to find statistical differences between controls with a normal high-resolution CT scan and subjects with pleural plaque only, but also noted subjects with pleural plaque only tended to have slightly lower mean total lung capacity, FVC, FEV1, FEV1/FVC and DLCO values than their controls. In 2009, the American College of Chest Physicians published results of the Delphi study (23), which assessed and quantified the opinions of experts in asbestos-related disease on various clinical issues. Physicians disagreed strongly with the statement, “Pleural plaques alter lung function to a clinically significant degree.” All the experts in asbestos-related disease also strongly disagreed with the statement. These opinions are consistent with our results, which show pleural plaque alone does not significantly affect pulmonary function.
Our study has several potential limitations. First, this study was performed retrospectively with a limited sample size. Since we focused on the correlation between pulmonary function and PPV, we included patients with pleural plaque only. This meant that despite a large potential cohort of subjects with pleural plaque on CT, the number of exclusions was exceptional; the previous pulmonary surgery or the presence of asbestosis, emphysema, or other lung parenchymal abnormalities, and the sample size was limited. And further studies with larger sample sizes are required to validate our results. Second, we subdivided PPV and examined statistical difference of pulmonary function among these groups, but the number of each group was too small. And there is a limit to having statistical significance. Third, we used an objective CT method to trace pleural plaque, but this method introduces the possibility of measurement error. In particular, it was often difficult to differentiate pleural plaque, extrapleural structures or dependent atelectasis when pleural plaques were thin. Fourth, quantifying PPVs was time consuming and tedious, and our method would not be easily applied, though this limitation could be overcome by appropriate automating software.
In conclusion, we quantified PPVs using CT images and found higher PPV had a trend toward restrictive pattern. However, the presence of pleural plaque alone was not significantly associated with pulmonary function.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This retrospective study was approved by our Institutional review board (approval #2015-141).
References
- Kim JS, Lynch DA. Imaging of nonmalignant occupational lung disease. J Thorac Imaging 2002;17:238-60. [Crossref] [PubMed]
- Cha YK, Kim JS, Kim Y, et al. Radiologic Diagnosis of Asbestosis in Korea. Korean J Radiol 2016;17:674-83. [Crossref] [PubMed]
- Peacock C, Copley SJ, Hansell DM. Asbestos-related benign pleural disease. Clin Radiol 2000;55:422-32. [Crossref] [PubMed]
- Kim Y, Myong JP, Lee JK, et al. CT Characteristics of Pleural Plaques Related to Occupational or Environmental Asbestos Exposure from South Korean Asbestos Mines. Korean J Radiol 2015;16:1142-52. [Crossref] [PubMed]
- Aberle DR, Gamsu G, Ray CS. High-resolution CT of benign asbestos-related diseases: clinical and radiographic correlation. AJR Am J Roentgenol 1988;151:883-91. [Crossref] [PubMed]
- Van Cleemput J, De Raeve H, Verschakelen JA, et al. Surface of localized pleural plaques quantitated by computed tomography scanning: no relation with cumulative asbestos exposure and no effect on lung function. Am J Respir Crit Care Med 2001;163:705-10. [Crossref] [PubMed]
- Copley SJ, Wells AU, Rubens MB, et al. Functional consequences of pleural disease evaluated with chest radiography and CT. Radiology 2001;220:237-43. [Crossref] [PubMed]
- Clark KA, Flynn JJ, Goodman JE, et al. Pleural plaques and their effect on lung function in Libby vermiculite miners. Chest 2014;146:786-94. [Crossref] [PubMed]
- Fridriksson HV, Hedenstrom H, Hillerdal G, et al. Increased lung stiffness of persons with pleural plaques. Eur J Respir Dis 1981;62:412-24. [PubMed]
- Jarvholm B, Sanden A. Pleural plaques and respiratory function. Am J Ind Med 1986;10:419-26. [Crossref] [PubMed]
- Schwartz DA, Fuortes LJ, Galvin JR, et al. Asbestos-induced pleural fibrosis and impaired lung function. Am Rev Respir Dis 1990;141:321-6. [Crossref] [PubMed]
- Kilburn KH, Warshaw R. Pulmonary functional impairment associated with pleural asbestos disease. Circumscribed and diffuse thickening. Chest 1990;98:965-72. [Crossref] [PubMed]
- Oliver LC, Eisen EA, Greene R, et al. Asbestos-related pleural plaques and lung function. Am J Ind Med 1988;14:649-56. [Crossref] [PubMed]
- Lynch DA, Austin JH, Hogg JC, et al. CT-Definable Subtypes of Chronic Obstructive Pulmonary Disease: A Statement of the Fleischner Society. Radiology 2015;277:192-205. [Crossref] [PubMed]
- International Labor Organization. Guidelines for the use of the ILO international classification of radiographs of pneumoconiosis. (rev. 1980). Geneva, Switzerland: International Labor Office Occupational Health and Safety Series;1980.
- Friedman AC, Fiel SB, Fisher MS, et al. Asbestos-related pleural disease and asbestosis: a comparison of CT and chest radiography. AJR Am J Roentgenol 1988;150:269-75. [Crossref] [PubMed]
- al Jarad N, Poulakis N, Pearson MC, et al. Assessment of asbestos-induced pleural disease by computed tomography--correlation with chest radiograph and lung function. Respir Med 1991;85:203-8. [Crossref] [PubMed]
- Meirelles GS, Kavakama JI, Jasinowodolinski D, et al. Pleural plaques in asbestos-exposed workers: reproducibility of a new high-resolution CT visual semiquantitative measurement method. J Thorac Imaging 2006;21:8-13. [Crossref] [PubMed]
- Schwartz DA, Galvin JR, Yagla SJ, et al. Restrictive lung function and asbestos-induced pleural fibrosis. A quantitative approach. J Clin Invest 1993;91:2685-92. [Crossref] [PubMed]
- Clin B, Paris C, Ameille J, et al. Do asbestos-related pleural plaques on HRCT scans cause restrictive impairment in the absence of pulmonary fibrosis? Thorax 2011;66:985-91. [Crossref] [PubMed]
- Revelli M, Chiesa F, Del Prato A, et al. Role of respiratory-triggered diffusion-weighted MRI in the assessment of pleural disease. Br J Radiol 2016. [Epub ahead of print]. [Crossref] [PubMed]
- Coolen J, De Keyzer F, Nafteux P, et al. Malignant pleural mesothelioma: visual assessment by using pleural pointillism at diffusion-weighted MR imaging. Radiology 2015;274:576-84. [Crossref] [PubMed]
- Banks DE, Shi R, McLarty J, et al. American College of Chest Physicians consensus statement on the respiratory health effects of asbestos. Results of a Delphi study. Chest 2009;135:1619-27. [Crossref] [PubMed]